Abstract
Background
Hypotension and hypoxemic respiratory failure are common among neonates with hypoxic–ischemic encephalopathy (HIE) undergoing therapeutic hypothermia (TH). Right ventricular (RV) dysfunction is associated with adverse neurodevelopment. Individualized management utilizing targeted neonatal echocardiography (TnECHO) may enhance care.
Methods
We evaluated the influence of TnECHO programs on cardiovascular practices in HIE/TH patients utilizing a 77-item REDCap survey. Nominated representatives of TnECHO (n = 19) or non-TnECHO (n = 96) sites were approached.
Results
Seventy-one (62%) sites responded. Baseline neonatal intensive care unit characteristics and HIE volume were comparable between groups. Most centers monitor invasive blood pressure; however, we identified 17 unique definitions of hypotension. TnECHO centers were likelier to trend systolic/diastolic blood pressure and request earlier echocardiography. TnECHO responders were less likely to use fluid boluses; TnECHO responders more commonly chose an inotrope first-line, while non-TnECHO centers used a vasopressor. For HRF, TnECHO centers chose vasopressors with a favorable pulmonary vascular profile. Non-TnECHO centers used more dopamine and more extracorporeal membrane oxygen for patients with HRF.
Conclusions
Cardiovascular practices in neonates with HIE differ between centers with and without TnECHO. Consensus regarding the definition of hypotension is lacking and dopamine use is common. The merits of these practices among these patients, who frequently have comorbid pulmonary hypertension and RV dysfunction, need prospective evaluation.
Impact
-
Cardiovascular care following HIE while undergoing therapeutic hypothermia varies between centers with access to trained hemodynamics specialists and those without.
-
Because cardiovascular dysfunction is associated with brain injury, precision medicine-based care may be an avenue to improving outcomes.
-
Therapeutic hypothermia has introduced new physiological considerations and enhanced survival. It is essential that hemodynamic strategies evolve to keep pace; however, little literature exists.
-
Lack of consensus regarding fundamental definitions (e.g., hypotension) highlights the importance of collaboration among the scientific community to advance the field.
-
The value of enhanced cardiovascular care guided by hemodynamic specialists requires prospective evaluation.
Similar content being viewed by others
Introduction
Term infants presenting with neonatal encephalopathy (NE) may have diverse contributors to their neurological phenotype, which may include developmental, metabolic, thrombotic, or other etiologies, of which hypoxia–ischemia is one common pathophysiology. NE is a leading cause of death or disability around the world.1 Therapeutic hypothermia (TH), which is now standard of care across developed countries, has reduced the risk of death and/or disability in survivors; however, 45–55% of neonates with NE continue to suffer adverse neurodevelopmental consequences despite optimal application of TH.2 Hypoxemic respiratory failure (HRF) secondary to acute pulmonary hypertension (aPH), also referred to as persistent pulmonary hypertension (PPHN), occurs in 6–25% of patients with NE/TH2,3,4 Concurrent diagnosis of transient myocardial ischemia or requirement for cardiovascular support for at least 24 h occurs in 62% patients.5 It has been speculated that cardiorespiratory compromise following birth, which includes cardiac dysfunction, hypotension, aPH or a combination thereof, may contribute to impaired long-term outcomes. Recent evidence suggests that both aPH6 and right ventricular (RV) dysfunction7 may be associated with mortality and/or abnormal neurological outcome in these neonates. This raises the possibility that early targeted cardiovascular care, based on enhanced physiologic/diagnostic precision, may provide an opportunity to improve long-term outcomes in this patient population.8
Evidence to support individualized cardiovascular care of patients with NE/TH is extremely limited. Comprehensive physiological appraisal and multiple echocardiography evaluations during the stabilization phase may be required, particularly to develop a robust evidence base for a particular strategy. In North America this may not be possible within the framework of a busy pediatric cardiology program. Targeted neonatal echocardiography (TnECHO) is a tool that enables real-time determination of physiology at the bedside in a noninvasive, rapid manner that can be followed serially to evaluate changes due to clinical evolution and/or therapy.9,10 Neonatal intensivists are increasingly utilizing TnECHO to guide cardiovascular care in the neonatal intensive care unit (NICU), and a developing body of literature supports its use in various neonatal disease states.11,12,13 Although formal TnECHO programs have been developing across Canada since 201114 and are starting to emerge in the United States of America,15 the role that these programs play in the care of neonates with cardiovascular disease in the setting of NE/TH is unknown. In this study, we aim to evaluate the influence of access to TnECHO on the contemporary approach to cardiovascular assessment and therapeutics among neonates with NE/TH compared to programs without access to this resource. We hypothesize that centers with active TnECHO programs will place a greater emphasis on pathophysiology-driven therapeutic strategies based on their greater access to this real-time hemodynamic assessment and knowledge.
Methods
A REDCap questionnaire was designed to evaluate diagnostic criteria, monitoring tools and treatment of circulatory dysfunction. A preliminary draft of questions was developed (R.E.G.) and circulated for feedback to three neonatologists with expertise in neonatal hemodynamics (P.T.L., J.L.R., P.J.M.) and three neonatologists with established expertise in neonatal neurology (K.M., M.E.D., P.W.). Questions were modified/dropped/added if a majority from both groups of experts agreed. The survey was modified and recirculated until all authors agreed on the questions. After approval, the survey was piloted by two neonatologists uninvolved in its development. Further refinement of wording and question structure was made following this pilot testing to optimize clarity of intent. The final 77-item survey was agreed upon by all authors. A waiver of the requirement for institutional research ethics board approval was obtained from the University of Iowa (Iowa, USA) and convenience sample was used.
Target population surveyed
The survey was distributed to two types of tertiary or quaternary centers as defined by access to TnECHO services. TnECHO centers were defined as sites with active clinical hemodynamic consultation services. Essential components to qualify as a hemodynamic consultation service include: (i) involvement of one or more neonatologists with formal advanced TnECHO training,14 (ii) performance of comprehensive clinical assessment and quantitative TnECHO evaluation(s) in patients with critical illness, (iii) the provision of physiological information and management advice to peer neonatologists. Access of non-TnECHO centers to pediatric cardiology services was assessed. TnECHO sites (n = 19) were identified via their representatives to the PanAmerican Hemodynamics Collaborative, which is an international consortium of neonatologists with advanced training in neonatal hemodynamics and TnECHO and represents all known TnECHO programs in North America. A single representative hemodynamics expert was requested to respond from each TnECHO center. Non-TnECHO sites (n = 96) were selected by contacting the Division Directors of all Canadian and American academic neonatology programs. The Division Chiefs in the United States were contacted via the Division Directors listserv and those in Canada were emailed individually. The Division Directors were asked to choose the single respondent with the most appropriate working knowledge of the subject matter of cardiovascular care for neonates with NE from their practice group. Potential responders were sent one reminder email 2 weeks after the initial contact. Responses were collected anonymously.
Center characteristics
Demographic characteristics of each center that were collected included center type (TnECHO or not), perinatal/inborn or referral/outborn center, unit size by bed and faculty number, access to extracorporeal membrane oxygenation (ECMO), and geographic location within North America. In order to evaluate the equivalency of the centers in terms of exposure to the disease population of interest, the number of cases with NE/TH per year was also collected.
Assessment/monitoring for cardiovascular disease
Information was collected on blood pressure monitoring including preferred location (4 limb, right upper, umbilical artery, or peripheral artery) and type (invasive/noninvasive). Responders were asked to provide their institutional definition of hypotension as free text, due to potential for heterogeneity given lack of direction from the literature. Similarly, the definition of HRF and methods used to evaluate the adequacy of oxygenation was queried. The institutional approach to the measurement of troponin was requested and, if measured, responders were asked to describe how troponin was used as a contributor to clinical care. Responders were asked whether echocardiography of any type was performed as a standard screening test (“routine screening”) in all patients admitted with NE/TH, and if so, at what time-point following admission. In addition, responders were asked to provide circumstances in which an echocardiogram (of any type) was typically requested for diagnostic reasons. The phase of illness in which echocardiography was typically requested as a diagnostic tool for hypotension or HRF was specifically queried. Details of specific echocardiography measurements quantifying common pathology, and clinically relevant aspects of cardiovascular disease of patients with NE/TH, were requested. Specifically, responders were asked to document if quantitative measures of left ventricle (LV) and RV performance, systemic and pulmonary blood flow, pulmonary pressure, and shunt characteristics were provided.
Therapeutic strategies for hemodynamic instability
The approach to volume replacement, including how much was typically given before moving on to a vasoactive medication, was asked. Participants were then requested to report whether their therapeutic strategy differed between patients with “isolated hypotension” as compared to those with both “hypotension and HRF.”. Responders were given the choice of individual vasoactive agents, which were then grouped for the purposes of reporting the results into primary vasopressors (e.g., dopamine, vasopressin, norepinephrine), primary inotropes (e.g., dobutamine), those with mixed action (e.g., hydrocortisone, epinephrine), or primary vasodilators (e.g., milrinone). All agents were selectable therapeutic options for questions related to hypotension both with and without HRF. The typical first- and second-line agents most commonly used were requested. For those centers in which the strategy differed depending on the presenting phenotype, both strategies were solicited. Pulmonary vasodilator therapeutic strategy was queried, including the approach to sedation/analgesia, the use of nitric oxide, and the frequency of systemically delivered pulmonary vasodilators (e.g., milrinone, sildenafil, prostacyclin analogs, bosentan). Clinical practices regarding the approach to initiation, discontinuation, and modulation of temperature in the setting of HRF were requested.16 Participants were given options as to whether the presence of refractory HRF would prompt changes in target temperature by differing degrees (e.g., 0.5°, 1° increase in target) or not at all. Finally, ECMO practices were evaluated.
Statistical analysis
Intergroup comparison between TnECHO and non-TnECHO centers was performed using univariate analysis. Statistics were performed using SPSS statistical software version 22 (Armonk, NY, USA) and figures were generated using Microsoft Excel version 16 (Redmond, WA, USA).
Results
Of centers surveyed, response was obtained from 71 (62%) locations. The proportion of responders from TnECHO centers (12/19, 61%) and non-TnECHO centers (59/96, 62%) was similar. Baseline NICU characteristics and volume of HIE cases did not differ by center type (Table 1). A larger proportion of TnECHO centers were located in Canada (p < 0.001).
Assessment/monitoring of systemic and pulmonary hemodynamics
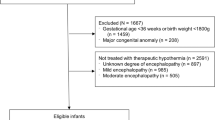
Most centers indicated a preference for invasive arterial blood pressure monitoring in these neonates. Most arterial catheters are placed in a post-ductal position via the umbilical artery (n = 54/57, 94%) route as opposed to a preductal peripheral artery. Intergroup differences were not present. Although more TnECHO centers utilized the individual components of systolic and diastolic to monitor blood pressure as compared to mean (p = 0.001), there was no consensus as to the definition of hypotension in this patient population. The most frequently cited definitions were mean arterial pressure less than gestation in weeks (n = 12, 17%), mean arterial pressure less than gestation with associated signs of low cardiac output (n = 11, 15%), and systolic/diastolic <3rd percentile (n = 9, 13%) (Fig. 1). Troponin was measured with equal frequency in both center types (Table 2). The most commonly reported indications for troponin measurement included screening for multiorgan injury (n = 24, 62%), or attempt to gauge myocardial ischemia among patients with clinical cardiovascular disease (n = 17, 38%). The latter rationale for measuring troponin was cited by 50% (3/6) of TnECHO and 42% (12/33) of non-TnECHO centers (p = NS). Choice of metrics of oxygenation efficacy among patients with HRF differed between the centers. Responders in non-TnECHO centers were more likely to use partial pressure of oxygen in arterial blood (PaO2) (n = 37, 63%) whereas TnECHO centers were more likely to use FiO2 requirement and SpO2 (n = 10, 83%; p = 0.009). The criteria used to define HRF could be grouped into three broad categories, which were evenly distributed across center type (Table 2).
Definitions of hypotension using a mean blood pressure threshold (a) or systolic blood pressure threshold (b). GA gestational age, LCOS low cardiac output state (e.g., low urine output, persistent lactic acidosis), NIRS cerebral near-infrared spectroscopy, MAP mean arterial pressure, SAP systolic arterial pressure, mmHg millimeters of mercury.
Echocardiography
All centers had access to echocardiography provided either by a TnECHO program, a pediatric cardiology program, or both. Routine pre-symptomatic screening echocardiography is performed in a minority of both TnECHO (n = 3, 25%) and non-TnECHO (n = 21, 36%) centers (p = NS). Among centers that routinely obtain echocardiography, most (n = 16, 70%) studies are obtained on the first postnatal day. Diagnostic echocardiography to evaluate hypotension was obtained earlier in the disease course by TnECHO centers (Table 2). Objective measurement of LV systolic function was commonly available at both center types; however, TnECHO centers were more likely to have access to quantitative measures of RV systolic function (p = 0.02), cardiac output (p = 0.05), ductal size (p = 0.04), atrial shunt size (0.02), and atrial shunt direction (p = 0.01) (Table 3).
Treatment strategies for impaired systemic blood flow/hypotension
More TnECHO centers indicated that the management for isolated hypotension and/or impaired cardiac output differed if concurrent HRF was also present (p = 0.01). Among TnECHO centers, it was more common to start a vasoactive medication without first giving a saline bolus (i = 0.01); however, when given as a first-line agent, the volume of saline did not differ between centers (Table 2). The first-line strategy for isolated hypotension in TnECHO centers was more likely to be a positive inotrope such as dobutamine or an agent with mixed inotrope and vasopressor action such as epinephrine, whereas physicians in non-TnECHO centers were more likely to choose a vasoconstricting agent, primarily dopamine, as first-line (p = 0.007). Early hydrocortisone use (1st or 2nd line) occurred in a minority of TnECHO (n = 3, 25%) and non-TnECHO (n = 11, 19%) centers (p = NS). Among patients with hypotension and HRF, more TnECHO centers use medications that are expected to lower the ratio of pulmonary vascular resistance (PVR) to systemic vascular resistance (SVR) such as vasopressin or norepinephrine as first-line therapies for hypotension (p = 0.01) (Table 2). In contrast, physicians at non-TnECHO centers used dopamine as a part of the management strategy in this patient population (p < 0.001).
Treatment strategies for impaired pulmonary blood flow/hypoxemia
Most centers, irrespective of group allocation, use inhaled nitric oxide as the first-line medication for HRF among the NE/TH population. There were no major differences in the use of sedation strategies between centers, although routine narcotic infusions were more frequently used in TnECHO centers (p = 0.05) (Table 4). The approach to cardiovascular support, however, differed between the groups. Milrinone was reported as a first- (n = 6, 10%) or second-line pulmonary vasodilator therapy (n = 50, 85%) at non-TnECHO centers. In contrast, none of the TnECHO centers reported use of milrinone as first line or second line in this population (p = 0.01). Sildenafil was used occasionally; however, neither bosentan nor prostacyclin analogs were frequently used irrespective of center type (Table 4). An additional strategy used to reverse refractory hypoxemia, primarily at TnECHO centers, was to modify target temperature (p = 0.002). Most responders at TnECHO centers (n = 7, 59%) reported increasing the target temperature by 0.5–1°, while 2 (16%) would make no temperature adjustment and 3 (25%) would discontinue TH. In contrast, most physicians at non-TnECHO centers (n = 42, 71%) reported they would make no temperature adjustment, while 7 (12%) would increase the target temperature by 0.5–1° and 10 (17%) would discontinue TH. Unlike TnECHO centers, non-TnECHO centers were more likely to administer ECMO for at least one patient with the concurrent diagnosis of NE/TH and HRF per year (p = 0.01) (Table 2). Regardless of center type, most responders will maintain TH while on ECMO [TnECHO centers 4/6 (67%) vs. non-TnECHO 42/47 (89%); NS].
Discussion
Precision medicine, with its emphasis on individualization, is an important focus for healthcare research in a variety of fields. Patients with NE who have an element of hypoxic–ischemic (HI) injury and are undergoing TH may have complex cardiopulmonary physiology, which makes this patient population well suited to study the value of tools that provide enhanced diagnostic accuracy and longitudinal monitoring on patient outcomes. In this survey, we demonstrate that the availability of cardiopulmonary physiologic information due to access to hemodynamic expertise and real-time evaluation of disease pathophysiology influences care practices of both hypoxemia and hypotension. It is important to recognize that, while these perspectives may have physiologic merit, clinical superiority should not be assumed. Rather, the clinical impact of each approach should be subjected to prospective evaluation.
The clinical phenotype of newborns with NE is complex. The neurological injury may be multifactorial, and among those with a significant component of HI, the cardiopulmonary phenotype may also be characterized by a variety of different contributors. Specifically, three mechanisms of cardiovascular dysfunction have been described in neonates following a perinatal hypoxic insult: (1) depressed LV function from the initial insult that is further exacerbated by reactive oxygen species (from the reperfusion injury) leading to reduced cardiac output and pulmonary venous hypertension, (2) hypoxic vasoconstriction of the pulmonary vascular bed leading to elevated PVR and aPH physiology; and (3) primary insult to RV performance with potential to lead to biventricular enlargement, dilated cardiomyopathy, and further impairment to systemic circulation and end-organ perfusion. These perturbations alone or in combination may result in failure to initiate normal transition through spontaneous breathing, such that neonates with HI are at risk of pathological persistence of elevated PVR, aPH, and RV and LV dysfunction.3 The biological nature of hypoxemia may be mistaken for lung parenchymal disease and the need for high ventilator pressures intended to “open the lung.” The consequences to patients with normal functional residual capacity may include over-distension-mediated impairment of pulmonary blood flow,17 reduced LV end-diastolic volume,18 LV stroke volume,18 and impaired systemic perfusion.19 Perinatal asphyxia also causes cardiac ischemia, to which the neonatal myocardium is uniquely vulnerable20,21 and ongoing postnatal hypoxia may upregulate a variety of molecular pathways that may further impair contractility.22 The RV may be particularly vulnerable due to higher metabolic requirements,23 more vulnerable coronary circulation,24 and greater afterload sensitivity.25,26 Comorbid infection or adrenal injury may further complicate the picture as does the introduction of TH. Reducing core body temperature increases both PVR27 and SVR, and worsens oxygenation failure.28
The value of clinical indices of cardiovascular well-being include blood pressure, end-organ function (e.g., urine output), and biochemical evidence of hypoperfusion (e.g., metabolic acidosis, lactate) is questionable as both the primary HI insult and altered core body temperature may impact their reliability. This confluence of factors make identification of contributors to cardiovascular dysfunction and determination of hemodynamic stability difficult.29 In addition, medications that are commonly utilized and biologically plausible among patients with aPH alone, may have unintended effects in this patient population. Milrinone, for example, has been associated with severe systemic hypotension, which may be related to impaired clearance in patients with NE/TH.30 Without access to real-time information regarding the ambient physiology, it is extremely difficult to unravel the natural evolution of the disease from other causes of deterioration. This is most important when considering the side effects of well-intended intensive care strategies, including not only cardiovascular-specific agents but also the introduction of alternative sedative agents (i.e., dexmedetomidine), which may also become protocolized. Limited access to echocardiography is a challenge in some centers and may have direct clinical implications secondary to diagnostic delay or lack of longitudinal appraisal of treatment response. The establishment of neonatal hemodynamic programs, where comprehensive TnECHO is performed by trained neonatology consultants, enables enhanced diagnostic precision and a more judicious approach to therapeutic intervention.31,32 Optimization of heart and lung function may enhance the recovery of organ function and positively modulate patient outcomes.
Scientific evidence to justify contemporary approaches to cardiovascular care in term neonates with NE/TH is limited. Neonatal practice has largely evolved from the approach to preterm infants, which focuses on the achievement of a mean arterial pressure target using a stepwise escalation of agents.33 The prevalence of dopamine as a first-line agent in this and other34 surveys of pulmonary hypertension management suggests that the primary goal of the therapy is to overcome the pulmonary pressure, thereby divert blood into the lungs either through the RV or left to right through the ductus arteriosus. This approach may have limitations, particularly among the sickest of patients; specifically, dopamine has been associated with an increase in the PVR:SVR ratio due to a greater degree of vasoconstriction in the more reactive pulmonary vascular bed.35,36,37 This may have negative consequences on RV performance and therefore, indirectly, cardiac output. High-dose catecholamine infusions may also be associated with tachycardia, which, when sustained, leads to a decrement in myocardial performance. This is related both to excessive metabolic demands and insufficient time for calcium to be cleared from the sarcolemma between beats.38 Patients with HI and concurrent acute PH may already have both disease-related tachycardia and pre-existing cardiac dysfunction. These patients may therefore be at greater risk of failed compensatory mechanisms and potentially a decline in cardiac efficacy under tachycardic conditions.39 There is emerging evidence that vasopressin, which is a systemic vasoconstrictor with favorable effects on the pulmonary vascular bed and minimal impact on heart rate, may be a more logical agent for hypotensive patients with aPH.40 Improved access to longitudinal TnECHO information may help clinicians justify both choice of therapy, characterize the efficacy of its intended role, and further customize therapy if the desired end-point is not reached. Repeated exposure to medications that perform more reliably, in addition to the aforementioned factors, may have contributed to a gradual change in practice at TnECHO sites. It is possible that this evolution of practice could contribute to a lower frequency of ECMO in this population in TnECHO centers; however, it is not possible to be conclusive based on this study methodology, particularly with geographic variation in site type.
Recent evidence suggests that hemodynamic instability and changes in cardiovascular health may contribute, at least in part, to brain injury; specifically, emerging data linking aPH and RV dysfunction to abnormal neurological outcomes suggests a role for the cardiovascular system in modulating postnatal risk of brain injury.6,7,41 The presence of aPH during TH has also been associated with increased risk of abnormal brain magnetic resonance imaging (MRI) and neurodevelopmental impairment.6,42 Similarly, both low tricuspid annulus plane systolic excursion (TAPSE, measure of RV longitudinal systolic function) and RV fractional area change (a surrogate for RV ejection fraction) have been independently associated with death or abnormal brain MRI in patients with NE/TH.7 Abnormal cerebral hemodynamics was identified in this and other studies.43,44,45,46 It is biologically plausible that prolonged derangement in the balance of supply and demand of substrate to the brain may aggravate injury and may therefore be an opportunity for targeted intervention. These data suggest that early inotropic support for RV dysfunction and a focus on ensuring vasoconstricting medications achieve a balance of adequate coronary and cerebral organ perfusion pressure without exacerbating the high PVR state, may be important modulators of brain injury. In order to pursue this hypothesis, the field will need to move beyond symptom-based management and evaluate alternative approaches to monitoring and intervention in well-controlled trials. Agreement on metrics, indicating stability whether this be a specific type, location, level of blood pressure, another clinical marker (or combination thereof), or an alternative marker of physiological health, is an essential prerequisite to large-scale research in this area. Training programs for neonatal hemodynamics specialists with the skills to perform and interpret early echocardiography may be one avenue to pursue. Real-time monitoring, however, should not be limited to the heart. The continued evolution and validation of end-organ monitoring tools (e.g., near-infrared spectroscopy) is needed to provide continuous organ-specific monitoring of this complex and frequently changing cardiopulmonary disease.
There are some potential limitations to our survey. First, this study was not designed to evaluate the direct impact of variance in approach to monitoring or treatment on patient stability or clinical outcomes; therefore, the findings should not be extrapolated to indicate that one specific diagnostic or therapeutic approach is necessarily superior. Second, although 38% of those surveyed did not respond, it is unlikely that those units are systematically different than responders. Although literature in this area is sparse, the perspectives of non-TnECHO centers are well aligned with prior publications, which evaluated cardiovascular care in this patient population.3,47 Third, we surveyed single representatives of each unit with a designation of a leadership position. While respondents were asked to provide information that reflected the perception of unit approach as a whole, personal biases may exist and there may be some variation at an individual level, which was not captured. Fourth, based on this study design, it is not possible to confirm that NE patients are of equivalent disease severity at all sites. The difference in geographic distribution of TnECHO vs. non-TnECHO centers could be a contributor to bias; however, there are no known systematic differences between Canadian and American NICU practices that are relevant to this patient population. Fifth, we specifically asked responders about their approach to HI-related encephalopathy; however, it is possible that responders were replying with respect to their approach to the broader NE population. Finally, although TnECHO may complement the clinical examination, the merits and thresholds to initiate treatment require investigation to determine the risk–benefit ratio.
Conclusion
The approach to cardiovascular care, in neonates with NE undergoing TH, differs between centers with and without access to TnECHO. Consensus regarding the definitions of hypotension and HRF are lacking. Use of dopamine remains commonplace despite biologically plausible drawbacks. The use of enhanced diagnostic or longitudinal monitoring tools to better appraise the relationship between hemodynamic instability or abnormal heart function, its management, and brain health may enable improved therapeutic precision and the discovery of novel interventions.
References
Liu, L. et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388, 3027–3035 (2016).
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. Cd003311 (2013).
Lakshminrusimha, S. et al. Pulmonary hypertension associated with hypoxic-ischemic encephalopathy-antecedent characteristics and comorbidities. J. Pediatr. 196, 45–51.e3 (2018).
Shankaran, S. et al. Outcomes of safety and effectiveness in a multicenter randomized, controlled trial of whole-body hypothermia for neonatal hypoxic-ischemic encephalopathy. Pediatrics 122, e791–e798 (2008).
Shah, P., Riphagen, S., Beyene, J. & Perlman, M. Multiorgan dysfunction in infants with post-asphyxial hypoxic-ischaemic encephalopathy. Arch. Dis. Child Fetal Neonatal Ed. 89, F152–F155 (2004).
More, K. S. et al. Cardiovascular associations with abnormal brain magnetic resonance imaging in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia and rewarming. Am. J. Perinatol. 35, 979–989. https://doi.org/10.1055/s-0038-1629900 (2018).
Giesinger, R. E. et al. Impaired right ventricular performance is associated with adverse outcome after hypoxic ischemic encephalopathy. Am. J. Respir. Crit. Care Med. 200, 1294–1305. https://doi.org/10.1164/rccm.201903-0583OC (2019).
Altit, G. & Levy, P. T. Cardiopulmonary impact of hypoxic ischemic encephalopathy in newborn infants. The emerging role of early hemodynamic assessment in determining adverse neurological outcomes. Am. J. Respir. Crit. Care Med. 200, 1206–1207 (2019).
Kluckow, M., Seri, I. & Evans, N. Echocardiography and the neonatologist. Pediatr. Cardiol. 29, 1043–1047 (2008).
Sehgal, A., Mehta, S., Evans, N. & McNamara, P. J. Cardiac sonography by the neonatologist: clinical usefulness and educational perspective. J. Ultrasound Med. 33, 1401–1406 (2014).
Amer, R., Kalash, R., Seshia, M. M. & Elsayed, Y. N. The impact of integrated evaluation of hemodynamics on management of preterm infants with late-onset compromised systemic circulation. Am. J. Perinatol. 34, 1011–1019 (2017).
Jain, A., McNamara, P. J., Ng, E. & El-Khuffash, A. The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am. J. Perinatol. 29, 101–106 (2012).
Jain, A. et al. Use of targeted neonatal echocardiography to prevent postoperative cardiorespiratory instability after patent ductus arteriosus ligation. J. Pediatr. 160, 584–9.e1 (2012).
Mertens, L. et al. Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J. Am. Soc. Echocardiogr. 24, 1057–1078 (2011).
Giesinger, R. E. et al. Targeted neonatal echocardiography in the United States of America: the contemporary perspective and challenges to implementation. Pediatr. Res. 85, 919–921 (2019).
Benumof, J. L. & Wahrenbrock, E. A. Dependency of hypoxic pulmonary vasoconstriction on temperature. J. Appl. Physiol. 42, 56–58 (1977).
Polglase, G. R. et al. Positive end-expiratory pressure differentially alters pulmonary hemodynamics and oxygenation in ventilated, very premature lambs. J. Appl Physiol. 99, 1453–1461 (2005).
Reller, M. D., Donovan, E. F. & Kotagal, U. R. Influence of airway pressure waveform on cardiac output during positive pressure ventilation of healthy newborn dogs. Pediatr. Res. 19, 337–341 (1985).
Tana, M. et al. Determination of lung volume and hemodynamic changes during high-frequency ventilation recruitment in preterm neonates with respiratory distress syndrome. Crit. Care Med. 43, 1685–1691 (2015).
Azzopardi, D. V. et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med. 361, 1349–1358 (2009).
Kanik, E. et al. Assessment of myocardial dysfunction in neonates with hypoxic-ischemic encephalopathy: is it a significant predictor of mortality? J. Matern. Fetal Neonatal Med. 22, 239–242 (2009).
Calbet, J. A., Robach, P. & Lundby, C. The exercising heart at altitude. Cell. Mol. Life Sci. 66, 3601–3613 (2009).
Smolich, J. J. Ultrastructural and functional features of the developing mammalian heart: a brief overview. Reprod. Fertil. Dev. 7, 451–461 (1995).
Ryan, J. J. et al. Right ventricular adaptation and failure in pulmonary arterial hypertension. Can. J. Cardiol. 31, 391–406 (2015).
Reller, M. D., Morton, M. J., Reid, D. L. & Thornburg, K. L. Fetal lamb ventricles respond differently to filling and arterial pressures and to in utero ventilation. Pediatr. Res. 22, 621–626 (1987).
Pinson, C. W., Morton, M. J. & Thornburg, K. L. An anatomic basis for fetal right ventricular dominance and arterial pressure sensitivity. J. Dev. Physiol. 9, 253–269 (1987).
Rubini, A. Effect of perfusate temperature on pulmonary vascular resistance and compliance by arterial and venous occlusion in the rat. Eur. J. Appl. Physiol. 93, 435–439 (2005).
Thoresen, M. & Whitelaw, A. Cardiovascular changes during mild therapeutic hypothermia and rewarming in infants with hypoxic-ischemic encephalopathy. Pediatrics 106(Part 1), 92–99 (2000).
Giesinger, R. E., Bailey, L. J., Deshpande, P. & McNamara, P. J. Hypoxic-ischemic encephalopathy and therapeutic hypothermia: the hemodynamic perspective. J. Pediatr. 180, 22–30.e2 (2017).
Bischoff, A. R., McNamara, P. J. & Giesinger, R. E. Hemodynamic response to milrinone for refractory hypoxemia during therapeutic hypothermia for neonatal hypoxic ischemic encephalopathy. J Perinatol. https://doi.org/10.1038/s41372-021-01049-y (2021). [Epub ahead of print].
Papadhima, I. et al. Targeted neonatal echocardiography (TNE) consult service in a large tertiary perinatal center in Canada. J. Perinatol. 38, 1039–1045. https://doi.org/10.1038/s41372-018-0130-y (2018).
El-Khuffash, A., Herbozo, C., Jain, A., Lapointe, A. & McNamara, P. J. Targeted neonatal echocardiography (TnECHO) service in a Canadian neonatal intensive care unit: a 4-year experience. J. Perinatol. 33, 687–690 (2013).
Dasgupta, S. J. & Gill, A. B. Hypotension in the very low birthweight infant: the old, the new, and the uncertain. Arch. Dis. Child Fetal Neonatal Ed. 88, F450–F454 (2003).
Nakwan, N. & Chaiwiriyawong, P. An international survey on persistent pulmonary hypertension of the newborn: a need for an evidence-based management. J. Neonatal Perinat. Med. 9, 243–250 (2016).
Barrington, K. J., Finer, N. N. & Chan, W. K. A blind, randomized comparison of the circulatory effects of dopamine and epinephrine infusions in the newborn piglet during normoxia and hypoxia. Crit. Care Med. 23, 740–748 (1995).
Cheung, P. Y. et al. Systemic, pulmonary and mesenteric perfusion and oxygenation effects of dopamine and epinephrine. Am. J. Respir. Crit. Care Med. 155, 32–37 (1997).
Moraes-Silva, M. A. et al. Effects of dopamine on the pulmonary circulation of the dog. Braz. J. Med. Biol. Res. 17, 75–82 (1984).
Wiegerinck, R. F. et al. Force frequency relationship of the human ventricle increases during early postnatal development. Pediatr. Res. 65, 414–419 (2009).
Schmidt, M. R. et al. The neonatal but not the mature heart adapts to acute tachycardia by beneficial modification of the force-frequency relationship. Pediatr. Cardiol. 32, 562–567 (2011).
Mohamed, A., Nasef, N., Shah, V. & McNamara, P. J. Vasopressin as a rescue therapy for refractory pulmonary hypertension in neonates: case series. Pediatr. Crit. Care Med. 15, 148–154 (2014).
Al Balushi, A. et al. Hypotension and brain injury in asphyxiated newborns treated with hypothermia. Am. J. Perinatol. 35, 31–38 (2018).
Mohammad, K. et al. Hemodynamic instability associated with increased risk of death or brain injury in neonates with hypoxic ischemic encephalopathy. J. Neonatal Perinat. Med. 10, 363–370 (2017).
Vesoulis, Z. A., Liao, S. M. & Mathur, A. M. Late failure of cerebral autoregulation in hypoxic-ischemic encephalopathy is associated with brain injury: a pilot study. Physiol. Meas. 39, 125004 (2018).
Variane, G. F. T., Chock, V. Y., Netto, A., Pietrobom, R. F. R. & Van Meurs, K. P. Simultaneous near-infrared spectroscopy (NIRS) and amplitude-integrated electroencephalography (aEEG): dual use of brain monitoring techniques improves our understanding of physiology. Front. Pediatr. 7, 560 (2019).
Wintermark, P. et al. Brain perfusion in asphyxiated newborns treated with therapeutic hypothermia. Am. J. Neuroradiol. 32, 2023–2029 (2011).
Wintermark, P., Hansen, A., Warfield, S. K., Dukhovny, D. & Soul, J. S. Near-infrared spectroscopy versus magnetic resonance imaging to study brain perfusion in newborns with hypoxic-ischemic encephalopathy treated with hypothermia. Neuroimage 85(Part 1), 287–293 (2014).
Nonomura, M. et al. Combination therapy with erythropoietin, magnesium sulfate and hypothermia for hypoxic-ischemic encephalopathy: an open-label pilot study to assess the safety and feasibility. BMC Pediatr. 19, 13 (2019).
Acknowledgements
This project utilized REDCap, and therefore the following grant support requires acknowledgment: UL1TR002537 Grant citation notice.
Author information
Authors and Affiliations
Contributions
R.E.G.: study design, data collection, analysis, first draft of the manuscript; P.T.L./J.L.R./M.E.D./K.M./P.J.M.N./P.W.: study design, review of manuscript; P.J.M.N.: study design, analysis, final review of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Study responders completed the survey following confirmation that they consent to have their responses used as a part of this scientific endeavor. No patient consent was required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Giesinger, R.E., Levy, P.T., Ruoss, J.L. et al. Cardiovascular management following hypoxic–ischemic encephalopathy in North America: need for physiologic consideration. Pediatr Res 90, 600–607 (2021). https://doi.org/10.1038/s41390-020-01205-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01205-8
This article is cited by
-
Arterial pressure is not reflective of right ventricular function in neonates with hypoxic ischemic encephalopathy treated with therapeutic hypothermia
Journal of Perinatology (2023)
-
Impact of persistent pulmonary hypertension and oxygenation on brain injury in neonates with neonatal encephalopathy treated with therapeutic hypothermia
Journal of Perinatology (2023)
-
Variations in care of neonates during therapeutic hypothermia: call for care practice bundle implementation
Pediatric Research (2023)
-
Comparative evaluation of approach to cardiovascular care in neonatal encephalopathy undergoing therapeutic hypothermia
Journal of Perinatology (2022)
-
Management of cardiovascular dysfunction in neonates with hypoxic ischaemic encephalopathy; a national survey of current practice in the UK
Journal of Perinatology (2022)