Abstract
Background
Maternal depression complicates a large proportion of pregnancies. Current evidence shows numerous harmful effects on the offspring. Reviews, which include depression, concluded that stress has harmful effects on the offspring’s outcomes neuro-cognitive development, temperament traits, and mental disorders.
Objective
This mini review of recent studies, sought to narrow the scope of exposure and identify studies specifically assessing prenatal depression and offspring neuropsychiatric outcomes.
Study eligibility criteria
The review included longitudinal, cohort, cross-sectional, clinical, quasi-experimental, epidemiological, or intervention study designs published in English from 2014 to 2018.
Participants
Study populations included mother-child dyads, mother-father-child triads, mother-alternative caregiver-child triads, and family studies utilizing sibling comparisons.
Methods
We searched PubMED and Web of Science. Study inclusion and data extraction were based on standardized templates. The quality of evidence was assessed using the Newcastle-Ottawa Scale (NOS).
Results
Thirteen studies examining neuropsychiatric outcomes were included. We judged the evidence to be moderate to high quality.
Conclusions
Our review supports that maternal prenatal depression is associated with neuropsychiatric adversities in children.
Implications
Future investigations should unravel the biological underpinnings and target timely interventions as early in pregnancy as possible to prevent offspring neuropsychiatric harms.
Similar content being viewed by others
Introduction
Early life environmental adversities may exert consequences upon developing cells, tissues, and organs, their structure and function. These biological alterations may result in phenotypic differences between individuals that persist throughout the lifespan—a developmental plasticity phenomenon called “prenatal programming”.1,2,3,4
Maternal depression complicates a large proportion of pregnancies with 7.4–20% of women experiencing major or minor depression, dysthymia, or clinically significant depressive symptomatology during pregnancy.5 Yet, a large proportion of pregnant women with depression remain undetected.6 This does not merely reflect a lack of systematic screening, but also an unwillingness of women to admit experiencing depressive symptoms.7 Nearly half of women reported feeling too embarrassed to confess to a health-care professional that they are not feeling well and almost one-third were afraid that if they divulged their feelings, their baby would be taken away.7 Many of the rest feared repercussions such as stigma.7
Due to the high prevalence, maternal depression is a major complication of pregnancy and childbirth. Strongly predicted by prenatal depression,8 maternal postpartum depression also carries adverse consequences for the offspring.9 One systematic review and meta-analysis of studies published between 2010 and 2015, concluded that offspring of women with untreated depression during pregnancy were 56% more likely to be born preterm (<37 gestational weeks) and 96% more likely to be born with a low birth weight (<2.5 kg).10 Another review of studies published up to 2015 focused on the effects of maternal untreated pregnancy depression on a series of offspring outcomes ranging from birth outcomes and physiological effects to cognitive and psychopathological effects.11 While the evidence of the reviewed studies showed a number of harmful effects on the offspring, yet the evidence was controversial, particularly regarding preterm birth and low birth weight.11 Pregnancy factors such as maternal age, gestation length, current maternal depressive status, pre-pregnancy obesity, gestational diabetes/hypertension, preeclampsia, and substance use during pregnancy, if not properly considered, may inflate the to the body of evidence. Yet, another recent review of studies published between 2010 and 2017 concluded that maternal stress in pregnancy, which included depression, has harmful effects on the offspring’s neuro-cognitive development, negative affectivity, difficult temperament, and mental health.2 As it is important to consider the alternative possibilities, numerous reviews explore the harmful effects of offspring exposure to pharmacologically treated (e.g. SSRIs) maternal prenatal depression.12,13,14,15
To the best of our knowledge, no reviews have focused specifically on the consequences of prenatal depression on offspring neuropsychiatric outcomes. Hence, the objective of this review was to assess all recent studies assessing prenatal depression and offspring neuropsychiatric outcomes. We evaluate the quality of the evidence of the reviewed studies using the Newcastle-Ottawa Scale (NOS) assessment. To deepen the discussion, we examine whether potential harmful effects of maternal depression on offspring neuropsychiatric outcomes are specific to the pregnancy period or explained by postnatal depression and whether a specific window of vulnerability exists when the effects of prenatal depression on offspring neuropsychiatric outcomes are most detrimental. Furthermore, we briefly explore the potential mechanisms through which prenatal depression may exert harmful consequences on offspring neuropsychiatric development. Lastly, we highlight treatment methods for prenatal depression, thereby possibly preventing offspring neurodevelopmental harm.
Methods
We searched Pubmed/MEDLINE and Web of Science databases for human longitudinal, cohort, and cross-sectional studies, published between January 2014 and February 2018 in English, with either clinical, quasi-experimental, epidemiological, or intervention study designs.
We included studies focusing on mother-child dyads, mother-father/alternate caregiver-child triads. Study criteria included maternal prenatal depression with any depressive disorder diagnosis identified via medical registries, psychiatric interview, or depressive symptoms measured with self-report questionnaires. We excluded studies that used antidepressant use as the sole exposure measure, reported only on lifetime history of depression, used retrospective self-reports or unclearly defined exposure. We excluded studies that used other forms of psychological stress or only a combined exposure measure, such as a depression and anxiety mean score. For offspring neuropsychiatric outcomes, we considered internalizing and externalizing problems, including anxiety, depression, attention, conduct problems, attention-deficit hyperactivity disorder (ADHD), autism spectrum disorders, and schizophrenia.
We utilized RevMan5 software to generate the PRISMA flow diagram16 that describes the study selection process (Fig. 1). The studies’ characteristics, participant demographics, and data were systematically collected from each study using a standardized template.
We assessed risk of bias and the methodological quality in non-randomized, non-intervention, observational studies using NOS, a recommended method from the Cochrane Handbook of Systematic reviews.17,18
Results
The sensitive search strategy applied produced 5712 articles (1083 = Pubmed, 4629 = Web of Science) for all studies up until February 2018. Refining the results to publications from 2014 to 2018, rendered 766 articles (PubMed, n = 135; Web of Science, n = 631) for title and abstract review. Further hand searching of reference lists and other sources augmented the search findings (n = 9). We included 13 empirical studies that examined prenatal depression and neuropsychiatric outcomes in offspring. See Fig. 1 for the PRISMA diagram of inclusion.
Summary of main findings
Refer to Table 1 for a complete list of included studies, study characteristics, and main findings, as well as each studies covariates.
A Finnish longitudinal cohort study by Korhonen et al.,20 among 192 mother-child dyads, found that prenatal depression was significantly associated with the 16-year-old child’s externalizing behavior problems. Notably, in this study population, maternal depression, when the child was 8–9 years old, was not significantly associated with the child’s behavior problems, but when measured at the child’s age of 16 years it was associated with the child’s externalizing behavior problems.20 The study reported that children of women who had a “high stable” trajectory of depressive symptoms from pregnancy to the child’s adolescence had the highest risk for externalizing problems, suggesting that both pre- and postnatal depression increase the child’s risk.20
The Finnish Prediction and Prevention of Preeclampsia and Intrauterine Growth Restriction (PREDO) study by Lahti et al.21 of 2296 mother-child dyads found that higher maternal prenatal depressive symptoms were associated with higher internalizing, externalizing, and total psychiatric problems of the child aged 1.9–5.9 years. These effects were independent of maternal depressive symptoms measured at the childhood follow-up, suggesting that the harmful effects on the child outcomes are specific to the prenatal period. The effects were gestation-week nonspecific, meaning that higher maternal depressive symptoms at the 14 bi-weekly measurements between 12 and 39 gestational weeks, were associated with more problems across a broad range of child behaviors.21 The study found that maternal depressive symptoms at the child follow-up partially mediated the prenatal depression effects. Additionally, the offspring of women who were consistently more depressed during pregnancy and at the childhood follow-up displayed the most problems,21 supporting the concept that both pre- and postnatal factors play a role.
In another study from the Finnish PREDO cohort by Wolford et al.,30 among 1779 mother-child dyads, higher maternal depressive symptoms during pregnancy were associated with significantly increased ADHD symptoms in children aged 3–6 years. These effects were independent of and partially mediated by maternal depressive symptoms measured in the childhood follow-up and were gestation-week nonspecific; children of mothers with consistently high depressive symptoms both during pregnancy and in early childhood had the most ADHD symptoms.30
The German Franconian Cognition and Emotion Study (FRANCES) study by Eicheler et al.,19 which assessed children of 61 depressed and 143 non-depressed mothers, found that at age 6–9 years, offspring of depressed mothers scored higher on anxiety, depression, and antisocial behavior. The associations with child depression and anxiety were independent of maternal depressive symptoms measured at the child follow-up, pointing to prenatal specificity of these effects.19 Yet, it remains unknown if the prenatal depression effects on child antisocial behavior would have been explained by maternal depressive symptoms during the child follow-up as the authors did not report these effects in the paper. This study also was unable to address if there would be a vulnerability window when maternal depressive symptoms would have had the most harmful offspring consequences, as the study measured depressive symptoms only once, during the third pregnancy trimester.19
In the Dutch Generation R study by El Marroun et al.,22 among 5596 mother-child dyads, 1.5- to 6-year-old children exposed to maternal depressive symptoms (without SSRIs) at 20 weeks of gestation showed more pervasive developmental problems than the control group. These associations remained significant after adjusting for maternal postnatal depression. Supplemental analysis indicated that prenatal depressive symptoms tended to be associated with autistic traits even after adjusted for maternal depression at the child’s age of 3 years.22 This study also measured affective problems and found an increased risk for affective problems in children who were exposed to prenatal maternal depression (without SSRIs).22 With only one measure of prenatal depression, this study, however, leaves the vulnerability window unclear.
In the UK Avon Longitudinal Study of Parents and Children (ALSPAC) by Capron et al. among 4303 mother-child dyads, higher maternal depressive symptoms at 18th gestational week were associated with and increased risk for anxiety disorder in the 18-year-old offspring.29
In another ALSPAC study by Leis et al. among 2891 mother-child dyads, higher maternal depressive symptoms at 18th and/or 32nd gestational weeks were associated with higher risk of hyperactivity, emotional symptoms, conduct problems, and total difficulties in the 11-year-old offspring.26 When the child problems were rated by the child’s teacher, maternal prenatal depressive symptoms remained a significant predictor of the child’s hyperactivity.26
In the third ALSPAC study by O’Donnell et al.24 among 7944 mother-child dyads, maternal depressive symptoms at 18 weeks’ gestation predicted consistently elevated levels of the child’s behavior problems through ages 4–14 years.
All the ALSPAC study findings were independent of maternal postnatal depressive symptoms measured at the childhood follow-ups. While the ALSPAC study has maternal depressive symptoms measurements at 18th and 32nd gestational weeks, these are not systematically reported in the studies, hence leaving open the question of a window of vulnerability.
In another UK study by Plant et al.,25 in the South London Child Development (SLCD) study of 103 mother-child dyads maternal depressive symptoms at 20 or 30 weeks of gestation were associated with an increased risk of depression in the 25-year-old offspring.25 In this study maternal prenatal depressive symptoms were correlated with maternal postnatal depressive symptoms measured up to 12 months after delivery. Yet, the postnatal depressive symptoms were not associated with the adult offspring depression. In contrast, children exposed to maternal depression in early childhood (1–6 years) were at an increased risk for adult depression.25 This study also revealed an additive effect where each additional exposure to maternal depression measured at different developmental stages increased the risk of depressive symptoms in the offspring in adulthood.25 This study concluded that childhood maltreatment mediated the effect of maternal prenatal depressive symptoms on the child’s adulthood depression.25
In another US longitudinal study of 196 young, low-income, African American mothers and their children, a path analysis indicated two indirect paths mediating the effects of maternal prenatal depression on toddler total behavior problems.28 One indirect path indicated a significant path of maternal prenatal depression on toddler total problems at 24 months via maternal sensitivity at 24 months.28 The other indirect path showed that maternal depressive symptoms at 24 months mediated the effect of maternal prenatal depression on toddler total behavior problems at 24 months.28 It is unclear from this study whether prenatal depressive symptoms had effects on toddler behavior problems that were independent of maternal sensitivity and concurrent depression. As this study measured maternal depressive symptoms only once during pregnancy, the study was not able to address the question of specific vulnerability window.28
In another US study by Johnson et al.,27 in a clinical subsample of 178 depressed mothers from the Emory Women’s Mental Health Program for perinatal mental illness, 2.5- to 5-year-old children exposed to maternal pregnancy depression (without SSRI) were less likely to score in the “at-risk range” for pervasive developmental disorder than those exposed to SSRI. The post hoc nested sibling analysis found that the decreased likelihood for pervasive developmental disorder in children with depressed mothers without SSRIs to compared to those with SSRIs remained significant.27
The US Californian registry study by Wieckowski et al., comprising nearly 9 million mother-child dyads, found that maternal major depressive disorder (MDD; recurrent and single episode), dysthymia, depressive disorder not otherwise specified, and bipolar disorder increased the 4- to 21-year-old offspring’s risk of autism spectrum disorder by 1.6- to 2.75-fold.32 While the timing of the maternal hospitalizations during pregnancy and at delivery were available, the study did not report the associations separately by trimesters or delivery; nor reported data on maternal hospitalizations during the child follow-up period. Hence, it remains unclear if the effects were specific to the prenatal period and if effects varied according to pregnancy trimester.
Quality of the evidence
We found the overall quality of the evidence as high to moderate based on the NOS Assessment, which judged cohort and case-control studies on three domains; (1) selection, (2) comparability, and (3) outcome (Tables 1 and 2).
The 13 prospective studies included in this review represent participants from six high-income countries, five of which are European. The ALSPAC (n = 3)24,26,29 and SLCD studies (n = 1)25 both drew their cohorts from the southern UK population at around the same time period. The PREDO (n = 2),21,30 MoBA (n = 1),31 and Korhonen et al. (n = 1)20 studies examined Nordic populations. The German FRANCES19 and the Dutch Generation R study22 both examined southern European populations with Generation R comprising a multi-ethnic European population. In the US studies (n = 3),27,28,32 however, the populations’ distinct geographic, socioeconomic and clinical characteristics, and ethnic variation separate these three studies from each other.
All of the studies used mother-child dyads (n = 14), however, some studies used an additional caregiver measure (i.e. teacher or father) (n = 3),22,26,29 or a sibling comparison model (n = 2).27,31 Non-exposed participants were all drawn from the same populations as the exposed participants.19,20,21,22,24,25,26,27,28,29,30,31,32 Notably, there was one clinical subsample study.27 Only two studies used an objective maternal depression exposure measure, i.e. medical record diagnosis32 and the Clinical Interview Schedule (CIS) structured interview.25 Nine of the other studies used validated maternal report measures such as the Center for Epidemiological Studies Depression Scale (CES-D)21,28,30 and Edinburgh Postnatal Depression Scale (EPDS)19,20 for measuring prenatal depressive symptoms. The bi-weekly CES-D measurements in the PREDO on maternal prenatal depression sets a gold standard for understanding the stability and trajectory of symptoms throughout gestation and allows for time point vulnerability exploration,21,30 a key tenant missing from the other studies in this review. The ALSPAC study also measured maternal depression at multiple prenatal and postnatal timepoints with the EPDS, however, only selective timepoints were used in each of the studies’ analyses.24,26,29 The clinical subsample from the Emory Women’s Mental Health Program measured exposure using self-reports of SRI use and the Beck Depression Inventory, Second Edition (BDI-II).27 Although the BDI-II is a commonly used measure for depression in the general population, findings suggest questionable validity in prenatal and postnatal samples, especially when compared to the EPDS.33,34 The Norwegian MoBa study31 used three selected items from the Symptoms Checklist (SCL) version 5 comprising an externally non-validated measure of maternal depressive symptoms.31 Internally, a Norwegian study reporting on the reliability and validity of the short form the psychometric measures used in the MoBA study, indicates a strong correlation between the five items in the SCL-8 short form and the three items in the SCL-5 with the original SCL-25 for depression.35 Authors, cited their previous work reporting a moderate level of agreement between the self-report and diagnostic interview measures, however using the five-item version of the SCL-5.36
For comparability, 10 studies controlled for the sex of the offspring as the most important confounder,19,21,22,24,25,26,27,28,30,31 while 3 studies20,29,32 did not control for sex, reducing comparability. All 13 studies controlled for at least one other important factor such as age, gestation length, current maternal depressive status, maternal pre-pregnancy obesity, gestational diabetes/hypertension, preeclampsia, and smoking and alcohol use during pregnancy all of which may significantly impact the findings (see Table 1 for all covariates used in each analysis). Although one study did not report any of the adjusted analysis in the paper, the author’s indicated that it had no effect on the results.19 Select studies accounted for novel confounders such as childhood maltreatment in path analysis, which significantly attenuated the results,25 paternal pre- and postnatal depression or sibling analysis,27,31 both of which account for genetic and environmental effects supporting the prenatal programming hypothesis. Yet, regarding the sibling analyses, maternal depressive symptoms show high continuity from pregnancy to postpartum,21,30 and the Gjerde MoBA study31 did not describe the level of differential exposure among siblings or the inter-correlations between antenatal and postpartum symptoms that would have been needed to assess whether multi-collinearity posed a concern for any analyses. Overall differences in adjustment for confounders decreased the comparability of the results across studies.19,20,21,22,24,25,26,27,28,29,30,31,32
Regarding outcomes, three studies used an objective neuropsychiatric outcome measure removing the subjectivity of parental report questionnaires via medical record diagnosis,32 the CSR-Revised29 validated in young adult populations for identifying anxiety and depression,37 and the Structured Clinical Interview.25 All other studies (n = 10) used mother-/father-/caregiver-rated questionnaires. Six studies used the Child Behavior Checklist (CBCL), which measures internalizing, externalizing, and total problems; emotionally reactive, anxious/depressed, somatic, withdrawn, sleep, attention, and aggressive behavior problems; and affective, anxiety, pervasive developmental, attention-deficit/hyperactivity, and oppositional defiant problems alone20,21,22,27,31 or in combination with the Youth Self Report,20 or the Social Responsiveness Scale.22 Other studies measured parental reported symptoms using the Conners’ Hyperactivity Index for ADHD,30 the Brief Infant-Toddler Social and Emotional Assessment (BITSEA), which assesses internalizing, externalizing, dysregulation, and competence,28,38 and the SDQ for assessing prosocial behavior, hyperactivity, emotional symptoms, conduct problems, peer problems, and total difficulties.24,26 The FRANCES study measured internalizing and externalizing behaviors using a psychologist administered set of mother-rated questionnaires from the International Classifications of diseases, version 10 (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders, Version 4 (DSM-IV), which are not well-known and are available only in the German language; hence it remains challenging to evaluate their reliability and validity.19
All 13 studies followed participants for a suitable length of time for the designated outcome of interest. Notably, however, the CBCL has only been validated for ages 1–5, and inclusion of some participants at age 6 could have impacted the results in the Generation R study (40% age 6).22 Nine studies retained adequate numbers for follow-up and clarified how the authors dealt with missing data.19,20,21,22,25,27,28,30,31 Originally a very large cohort, the long-term follow-up of the ALSPAC studies (n = 3)1,26,29 experienced a high attrition rate, especially by follow-up at 18 years.24,26,29 However, the long-term adulthood follow-up in the ALSPAC studies24,26,29 and the US register study32 is a valuable addition to the literature. Notably, although the majority of studies have sample sizes in the thousands,21,22,24,26,29,30,31 one even over 8 000 000,32 five studies in this review have relatively small sample sizes.19,20,25,27,28
Limitations for this review as a whole include the small number of studies that met the inclusion criteria and a high risk of publication bias across the included studies. Furthermore, our data extraction was performed by only one author. One question pinpointed at the beginning of this review, e.g. a specific gestational vulnerability time point, could not be fully elucidated based on the current body of evidence and the lack of replication multi-point measures across studies.
Discussion
This review of 13 studies supports the previous findings reviewed by Van den Bergh et al.2, suggesting that prenatal depression is associated with adverse neuropsychiatric consequences on the offspring. Ten studies20,21,22,24,25,26,27,28,29,30 favored the conclusion that the effects of maternal depression on offspring neuropsychiatric outcomes are specific to the maternal pregnancy period and are not accounted for by depression after pregnancy. Two studies,19,32 however, did not address the pre- vs postnatal specificity question, and another31 concluded that the offspring neuropsychiatric effects are not specific to the prenatal period, but are rather a consequence of maternal depression during the offspring postnatal development. As discussed previously, the one dissenting study used non-validated measures of maternal depression, which hampers its reliability.31 Importantly, maternal depression shows high continuity from pregnancy onwards, with study populations21,30 indicating that in over 50% of the women, clinically relevant depressive symptomatology during pregnancy persists after delivery. Therefore, the question of exposure timing during pregnancy or after delivery of the maternal effects may be difficult to disentangle because of statistical multi-collinearity problems. Only the PREDO cohort from this review, with 14 bi-weekly gestational measurements of maternal depressive symptoms was able to address the question of a specific vulnerability window, which showed that the effects on child problem behaviors were gestation-week nonspecific.21,30
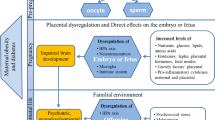
Pathways
Prenatal depressive symptoms may influence child neuropsychiatric outcomes via multiple psychological, health behavior, and biological pathways. An important component of understanding these pathways involves disentangling the effects of other pregnancy and perinatal complications, which may contribute to the severity, duration, and complexity of maternal prenatal depression. For instance, recent meta-analyses and systematic reviews show that maternal obesity in early pregnancy is associated with an increased risk of depression during pregnancy.39,40 Also in the PREDO cohort, from a study not in this review, women with early pregnancy overweight and obesity had consistently elevated depressive symptoms throughout pregnancy and after delivery.8 Evidence suggests that gestational diabetes and hypertension spectrum disorders may also be associated with prenatal depression,41 but these findings remain controversial.8
Maternal cardio-metabolic conditions might contribute as one of the pathways, as a meta-analysis found that maternal obesity predicted an increased risk of autism and ADHD, developmental delay, and emotional/behavioral problems in children.42 Also, we recently showed that maternal severe obesity in early pregnancy is associated with hyperactivity, sleep problems, conduct, externalizing and total problems, depressive symptoms, anxiety, and ADHD problems in children.43 Gestational diabetes has repeatedly been associated with an increased risk of neuropsychiatric disorders, particularly of autism and schizophrenia in the offspring.44,45,46,47 Yet, in the PREDO maternal obesity or gestational diabetes were not associated with mother-rated internalizing, externalizing, or total psychiatric problems in 1.9- to 5.9-year-old children,21 but were associated with child neurodevelopmental delay.48
Prenatal depression also increases risks of preterm birth and low birth weight.10,41 Also in the PREDO cohort, maternal depressive symptoms during pregnancy predicted shorter gestation length.49 Preterm birth and low birth weight have been consistently shown to be risk factors for neuropsychiatric disorders,50,51,52,53,54 and in sibling comparisons.51,52
Evidence from a meta-analysis and from large population-based studies suggests that depressed mothers are more likely to smoke throughout pregnancy,41,55 and prenatal smoking has been repeatedly associated with the risk of neuropsychiatric disorders in the offspring.21,56,57 Also in the PREDO, prenatal smoking was associated with increased internalizing, externalizing total psychiatric and ADHD problems in children.21,30
Biological mechanisms
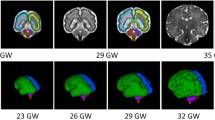
The biological mechanisms possibly linking maternal depression and psychological distress more generally with offspring neuropsychiatric outcomes were reviewed in Van den Bergh et al.2 According to this review, and studies published since, prenatal depression may be associated with child neurodevelopment via (1) alterations in hypothalamus-pituitary-adrenal (HPA)-axis functioning, (2) functional and structural changes of related brain areas, including amygdala and prefrontal cortex, (3) changes in autonomic nervous system, and (4) immune system functioning and in gut microbiota.2,58,59
At population level, one of the most consistent biological changes in depression is altered cortisol levels, indicating altered HPA-axis functioning.2,60,61 However, studies linking maternal depression specifically during pregnancy with maternal or infant cortisol levels have yielded inconsistent findings.2,60,61 Yet, maternal HPA-axis functioning during pregnancy has been linked with offspring neuropsychiatric problems.2 For instance, we recently showed that maternal licorice consumption during pregnancy predicted an over threefold risk of ADHD problems in the offspring62 due to glycyrrhizin, which inhibits the placental 11β-hydroxysteroid dehydrogenase type 2 (11βHSD2) enzyme. This enzyme protects the fetus from maternal glucocorticoids, hence leaving the fetus vulnerable to maternal glucocorticoid excess. Furthermore, structural and functional changes in the infant amygdala, which regulates HPA-axis functioning, have been repeatedly reported as a consequence of prenatal depression2,63,64,65 and are also associated with child psychopathology risk.66,67 Also, alterations in the functioning of the autonomic nervous system that also plays a key role in the stress response have been found in children exposed to prenatal depression.2
Changes in inflammatory pathways and gut microbiota, as a consequence of prenatal depression, offer another route through which prenatal depression may affect child neuropsychiatric problems. Maternal prenatal cytokine levels present questions for epigenetic programming as cytokines may pass through the placenta.68 Higher prenatal depression has also been directly associated with maternal inflammatory cytokine levels during pregnancy,69,70 but the findings are inconsistent. Correspondingly both anti-inflammatory drugs71 and probiotics72 have antidepressant effects. Prenatal levels of C-reactive protein (CRP), a key inflammatory marker, have been associated with offspring risk of different neuropsychiatric disorders,73,74,75,76 and prenatal depression is associated with offspring CRP levels.77 Evidence for the gut microbiota pathway predominately stems from animal studies but two recent studies have shown microbiota changes in offspring exposed to prenatal depression.78,79 Nonetheless, the biological mechanisms involved warrant further research.
Cellularly, depression-related changes in fetal biology studies have specifically focused on epigenetic modifications. There are several recent systematic reviews on the effects of maternal psychological distress during pregnancy and more specifically antenatal depression on placental and infant DNA methylation.2,80,81 Overall, these reviews state that the findings are inconsistent but many candidate gene studies have linked methylation of the NR3C1, the glucocorticoid-receptor gene, with maternal prenatal depression. Other potential, often examined, candidate genes include 11BHSD2, FKBP5, IGF2, SLC6A4, OXTR, CRH, and BDNF, genes that also play roles in HPA-axis regulation. Most studies have focused on either assessing placental DNA methylation or infant cord blood methylation levels. The studies have identified some significant effects, which still need validation. Future larger epigenome-wide-association studies harmonizing and pooling data into meta-analyses will overcome the current single-study limitations.
Recent findings from the PREDO suggest that changes in placental gene expression and infant DNA cord blood methylation as well as morphological changes in placental structure may be among the mediating biological pathways between antenatal depressive symptoms and child psychiatric problems. Among approximately 60 PREDO participants, prenatal depressive symptoms were associated with higher placental mRNA levels of glucocorticoid and mineralocorticoid receptor genes, findings that suggest higher placental glucocorticoid sensitivity.82,83 In a UK longitudinal study among 93 participants, we found that higher prenatal depressive symptoms were associated with reduced placental IGF2-2 mRNA levels and, particularly in the placentas of female fetuses, with altered mRNA levels of several genes regulating fetal glucocorticoid exposure.84 Furthermore, among PREDO participants, maternal prenatal depressive symptoms were associated with lower infant epigenetic gestational age at birth, a biomarker of the developmental maturation level of the fetus. This biomarker predicted increased total and internalizing psychiatric problems in boys, and partially mediated the effects of maternal prenatal depression on boys’ internalizing problems.85 Another PREDO study assessing placental morphology among 86 participants found less variation in placental villous barrier thickness of gamma-smooth muscle actin-negative villi in the placentas of antenatally depressed mothers, indicating reduced placental maturation, due to prenatal depression. This placental structural change predicted internalizing and total psychiatric problems in 60 toddlers86.
Treatments of prenatal depression
Predictors for full recovery from prenatal depression include the absence of maternal health concerns, low total parental stress status, and limited child behavior issues,87 while maternal sensitivity has been found to attenuate the effects of maternal prenatal depression on toddler total problems,28 all which underscore the need for a comprehensive treatment approach for prenatal depression. Antidepressant medication may offer an option as several reviews indicate the likelihood of serious harms is low.12,13,14,15 Although, investigations into specific medications and classes of antidepressants88,89,90 complicate the literature, suggesting serious harmful effects, leading many doctors not to prescribe and/or many women refuse/discontinue medication in pregnancy.5 Until the data on the safety and efficacy of antidepressant therapies are clearly defined, efforts should be concentrated to assess alternative therapies. Although they stray from antidepressants, pregnant women have reported an interest in cognitive behavioral therapy,5 which recent review evidence suggests has robust effects for the treatment of women with MDD.91 However, due to a lack of resources and limited access to standard therapies, nearly half of diagnosed women fail to receive timely evidence-based treatment.92 In lieu of standard delivery, online cognitive behavioral therapy interventions may serve as an effective measure for improving maternal perinatal mental health.93,94 Recent studies have considered the effectiveness of relaxation practices through musical therapy,95 fish oil supplementation,96 and dietary supplementation,97 and future studies could consider probiotic supplements.
Conclusions
Our review found a limited amount of high-to-moderate quality evidence supporting the association of prenatal depression and neuropsychiatric outcomes in children, published in 2014–2018. More carefully conducted cohort studies with multi-time point, validated exposure, and outcome measures investigating epigenetic and protective factors are needed to further corroborate the findings relating to a specific developmental vulnerability period. Further investigations into the implications of the timing and consistency of exposure, confounding by other perinatal conditions, and possible biological mechanisms would bolster the evidence. Future research needs continuous and prospective measures of maternal depressive symptoms throughout pregnancy and beyond, in order to better scope the prenatal and postnatal trajectories of depression, risk factors, and include follow-up of offspring into adulthood to assess long-term neuropsychiatric effects.
References
O’Donnell, K. J. & Meaney, M. J. Fetal origins of mental health: the developmental origins of health and disease hypothesis. Am. J. Psychiatry 174, 319–328 (2017).
Van den Bergh, B. R. H. et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 2017 Jul 28. pii: S0149-7634(16)30734-5. https://doi.org/10.1016/j.neubiorev.2017.07.003. [Epub ahead of print].
Gluckman, P. D. & Hanson, M. A. The developmental origins of health and disease: an overview. Dev. Orig. Health Dis. New York, USA:Cambridge University Press, 2006:1–5.
Barker, D. J. P. The origins of the developmental origins theory. J. Intern. Med. 261, 412–417 (2007).
Goodman, J. H. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth 36, 60–69 (2009).
Bauer, A., Parsonage, M., Knapp, M., Iemmi, V. & Adelaja, B. Costs of perinatal mental health problems.London, England:Centre For Mental Health, 2014 [Internet]. [cited 2018 May 7].
Russell, S., Lang, B., Clinton, J., Adams, C. J. L. Perinatal Mental Health: Mental Health Experiences of Women and Health, 2013. (https://www.tommys.org/sites/default/files/Perinatal_Mental_Health_Experiences%20of%20women.pdf).
Kumpulainen, S. M. et al. Maternal early pregnancy obesity and depressive symptoms during and after pregnancy. Psychol. Med. 48(14):2353-2363.(2018) e-pub ahead of print, 17 January 2018.
Girchenko, P. et al. Cohort profile: prediction and prevention of preeclampsia and intrauterine growth restriction (PREDO) study. Int. J. Epidemiol. 46, 1380–1381g (2017).
Jarde, A. et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: A systematic review and meta-analysis. JAMA Psychiatry 73, 826–837 (2016).
Gentile, S. Untreated depression during pregnancy: short- and long-term effects in offspring. A systematic review. Neuroscience 342, 154–166 (2017).
Andalib, S. et al. Maternal SSRI exposure increases the risk of autistic offspring: a meta-analysis and systematic review. Eur. Psychiatry 45, 161–166 (2017).
Gentile, S. & Fusco, M. L. Placental and fetal effects of antenatal exposure to antidepressants or untreated maternal depression. J. Matern. Fetal Neonatal Med. 30, 1189–1199 (2017).
Ornoy, A., Weinstein-Fudim, L. & Ergaz, Z. Antidepressants, antipsychotics, and mood stabilizers in pregnancy: what do we know and how should we treat pregnant women with depression. Birth Defects Res. 109, 933–956 (2017).
Mezzacappa, A. et al. Risk for autism spectrum disorders according to period of prenatal antidepressant exposure: a systematic review and meta-analysis. JAMA Pediatr. 171, 555–563 (2017).
Moher, D., Liberati, A. & Tetzlaff, J. A. D. PRISMA 2009 Flow Diagram. Prism. Statement 6, 1000097 (2009).
Wells, G. A. et al. Ottawa Hosp. Res. Inst. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses, 2013. (http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf).
Higgins J., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions [Internet]. Version 5. The Cochrane Collaboration; 2011.
Eichler, A. et al. Children of prenatally depressed mothers: externalizing and internalizing symptoms are accompanied by reductions in specific social-emotional competencies. J. Child Fam. Stud. 26, 3135–3144 (2017).
Korhonen, M., Luoma, I., Salmelin, R. & Tamminen, T. Maternal depressive symptoms: associations with adolescents’ internalizing and externalizing problems and social competence. Nord. J. Psychiatry 68, 323–332 (2014).
Lahti, M. et al. Maternal depressive symptoms during and after pregnancy and psychiatric problems in children. J. Am. Acad. Child Adolesc. Psychiatry 56, 30–39 (2017). e7.
El Marroun, H. et al. Prenatal exposure to selective serotonin reuptake inhibitors and social responsiveness symptoms of autism: population-based study of young children. Br. J. Psychiatry 205, 95–102 (2014).
Hermansen, T. K., Røysamb, E., Augusti, E.-M. & Melinder, A. Behavior and inhibitory control in children with prenatal exposure to antidepressants and medically untreated depression. Psychopharmacology (Berl), 233, 1523–35 (2016).
O’Donnell, K. J., Glover, V., Barker, E. D. & O’Connor, T. G. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev. Psychopathol. 26, 393–403 (2014).
Plant, D. T., Pariante, C. M., Sharp, D. & Pawlby, S. Prenatal depression and offspring depression in adulthood: role of child maltreatment. Br. J. Psychiatry 207, 213–220 (2015).
Leis, J. A., Heron, J., Stuart, E. A. & Mendelson, T. Associations between maternal mental health and child emotional and behavioral problems: does prenatal mental health matter? J Abnorm Child Psychol. 42, 161–71 (2014).
Johnson, K. C., Smith, A. K., Stowe, Z. N., Newport, D. J. & Brennan, P. A. Preschool outcomes following prenatal serotonin reuptake inhibitor exposure: differences in language and behavior, but not cognitive function. J. Clin. Psychiatry 77, E176–E182 (2016).
Edwards, R. C. & Hans, S. L. Prenatal depressive symptoms and toddler behavior problems: the role of maternal sensitivity and child sex. Child Psychiatry Hum. Dev. 47, 696–707 (2016).
Capron, L. E. et al. Associations of maternal and paternal antenatal mood with offspring anxiety disorder at age 18 years. J. Affect Disord. 187, 20–26 (2015).
Wolford, E. et al. Maternal depressive symptoms during and after pregnancy are associated with attention-deficit/hyperactivity disorder symptoms in their 3-to 6-year-old children. PLoS ONE 12, 1–13 (2017).
Gjerde, L. C. et al. Maternal perinatal and concurrent depressive symptoms and child behavior problems: a sibling comparison study. J. Child Psychol. Psychiatry 58, 779–786 (2017).
Wieckowski, B. M., Mukhtar, Y., Lee, J. J., Xing, G. & Walker, C. K. Higher autism in children of women with psychiatric diagnoses. Res. Autism Spectr. Disord. 33, 10–20 (2017).
Su, K.-P. et al. Different cutoff points for different trimesters? The use of Edinburgh Postnatal Depression Scale and Beck Depression Inventory to screen for depression in pregnant Taiwanese women. Gen. Hosp. Psychiatry 29, 436–441 (2007).
Harris, B., Huckle, P., Thomas, R., Johns, S. & Fung, H. The use of rating scales to identify post-natal depression. Br. J. Psychiatry 154, 813–817 (1989).
Tambs, K. & Røysamb, E. Selection of questions to short-form versions of original psychometric instruments in MoBa. Nor. Epidemiol. 24, 195–201 (2014).
Gjerde, L. C. et al. Strong genetic correlation between interview-assessed internalizing disorders and a brief self-report symptom scale. Twin Res. Hum. Genet. 14, 64–72 (2011).
McBride, O., Bebbington, P. & Cooper, C. Could the lower prevalence of affective disorder in older people be due to measurement error? Reliability of the Revised Clinical Interview Schedule in younger and older adults. J. Affect. Disord. 148, 310–315 (2013).
Briggs-Gowan, M. J., Carter, A. S., Irwin, J. R., Wachtel, K. & Cicchetti, D. V. The Brief Infant-Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. Journal of Pediatric Psychology 29, 143–155 (2004).
Molyneaux, E., Poston, L., Ashurst-williams, S. & Howard, L. M. Obesity and mental disorders during pregnancy and postpartum: a systematic review and meta-analysis. Obstet. Gynecol. 123, 857–867 (2014).
Steinig, J., Nagl, M., Linde, K., Zietlow, G. & Kersting, A. Antenatal and postnatal depression in women with obesity: a systematic review. Arch. Womens Ment. Health 20, 569–585 (2017).
Räisänen, S. et al. Risk factors for and perinatal outcomes of major depression during pregnancy: population-based analysis during 2002-2010 in Finland. BMJ Open 4 (2014).
Sanchez, C. E. et al. Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: a meta-analysis. Obes. Rev. 19, 464–484 (2018).
Mina, T. H. et al. Prenatal exposure to very severe maternal obesity is associated with adverse neuropsychiatric outcomes in children. Psychol. Med. 47, 353–362 (2017).
Nahum Sacks, K. et al. Prenatal exposure to gestational diabetes mellitus as an independent risk factor for long-term neuropsychiatric morbidity of the offspring. Am. J. Obstet. Gynecol. 215, 380 (2016). e1-380.e7.
Wan, H., Zhang, C., Li, H., Luan, S. & Liu, C. Association of maternal diabetes with autism spectrum disorders in offspring: a systemic review and meta-analysis. Medicine (Baltimore) 97, e9438 (2018).
Van Lieshout, R. J. & Voruganti, L. P. Diabetes mellitus during pregnancy and increased risk of schizophrenia in offspring: a review of the evidence and putative mechanisms. J. Psychiatry Neurosci. 33, 395–404 (2008).
Xiang, A. H. et al. Association of maternal diabetes with autism in offspring. JAMA 313, 1425–1434 (2015).
Girchenko, P. et al. Maternal early pregnancy obesity and related pregnancy and pre-pregnancy disorders: associations with child developmental milestones in the prospective PREDO Study. Int. J. Obes. (2018).
Pesonen, A. K. et al. Maternal prenatal positive affect, depressive and anxiety symptoms and birth outcomes: the PREDO study. PLoS ONE 11, 1–13 (2016).
Pyhälä, R. et al. Self-reported mental health problems among adults born preterm: a meta-analysis. Pediatrics 139, e20162690 (2017).
D’Onofrio, B. M. et al. Preterm birth and mortality and morbidity: a population-based quasi-experimental study. JAMA Psychiatry 70, 1231–1240 (2013).
Class, Q. A., Rickert, M. E., Larsson, H., Lichtenstein, P. & D’Onofrio, B. M. Fetal growth and psychiatric and socioeconomic problems: population-based sibling comparison. Br. J. Psychiatry 205, 355–361 (2014).
Räikkönen, K. et al. Depression in young adults with very low birth weight: the Helsinki study of very low-birth-weight adults. Arch. Gen. Psychiatry 65, 290–296 (2008).
Heinonen, K. et al. Common mental disorders in young adults born late-preterm. Psychol. Med. 46, 2227–2238 (2016).
Riaz, M., Lewis, S., Naughton, F. & Ussher, M. Predictors of smoking cessation during pregnancy: a systematic review and meta-analysis. Addiction 113, 610–622 (2018). (e-pub ahead of print 30 Jan 2018).
Ekblad, M., Lehtonen, L., Korkeila, J. & Gissler, M. Maternal smoking during pregnancy and the risk of psychiatric morbidity in singleton sibling pairs. Nicotine Tob. Res. 1, 597–604 (2017).
Quinn, P. D. et al. Association between maternal smoking during pregnancy and severe mental illness in offspring. JAMA Psychiatry 74, 589 (2017).
Stetler, C. & Miller, G. E. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom. Med. 73, 114–126 (2011).
Zorn, J. V. et al. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology 77, 25–36 (2017).
Bleker, L. S., Roseboom, T. J., Vrijkotte, T. G., Reynolds, R. M. & de Rooij, S. R. Determinants of cortisol during pregnancy—the ABCD cohort. Psychoneuroendocrinology 83, 172–181 (2017).
Thomas, J. C., Letourneau, N., Bryce, C. I., Campbell, T. S. & Giesbrecht, G. F. Biological embedding of perinatal social relationships in infant stress reactivity. Dev. Psychobiol. 59, 425–435 (2017).
Räikkönen, K. et al. Maternal licorice consumption during pregnancy and pubertal, cognitive, and psychiatric outcomes in children. Am. J. Epidemiol. 185, 317–328 (2017).
van der Knaap, N. J. F. et al. Maternal depressive symptoms during pregnancy are associated with amygdala hyperresponsivity in children. Eur. Child Adolesc. Psychiatry 27, 57–64 (2018).
Soe, N. N. et al. Perinatal maternal depressive symptoms alter amygdala functional connectivity in girls. Hum. Brain Mapp. 39, 680–690 (2018). e-pub 2 November 2017.
Wen, D. J. et al. Influences of prenatal and postnatal maternal depression on amygdala volume and microstructure in young children. Transl. Psychiatry 7, e1103 (2017).
Buss, C. et al. Maternal cortisol over the course of pregnancy and subsequent child amygdala and hippocampus volumes and affective problems. Proc. Natl Acad. Sci. USA 109, E1312–E1319 (2012).
Rogers, C. E. et al. Neonatal amygdala functional connectivity at rest in healthy and preterm infants and early internalizing symptoms. J. Am. Acad. Child Adolesc. Psychiatry 56, 157–166 (2017).
Zaretsky, M. V., Alexander, J. M., Byrd, W. & Bawdon, R. E. Transfer of inflammatory cytokines across the placenta. Obstet. Gynecol. 103, 546–550 (2004).
Shelton, M. M., Schminkey, D. L. & Groer, M. W. Relationships among prenatal depression, plasma cortisol, and inflammatory cytokines. Biol. Res. Nurs. 17, 295–302 (2015).
Karlsson, L. et al. Cytokine profile and maternal depression and anxiety symptoms in mid-pregnancy-the FinnBrain Birth Cohort Study. Arch. Womens Ment. Health 20, 39–48 (2017).
Köhler, O. et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects. JAMA Psychiatry 71, 1381 (2014).
Huang, R., Wang, K. & Hu, J. Effect of probiotics on depression: a systematic review and meta-analysis of randomized controlled trials. Nutrients 8, 483 (2016). [cited 2018 Apr 26].
Canetta, S. et al. Elevated maternal C-reactive protein and increased risk of schizophrenia in a national birth cohort. Am. J. Psychiatry 171, 960–968 (2014).
Brown, A. S. et al. Elevated maternal C-reactive protein and autism in a national birth cohort. Mol. Psychiatry 19, 259–264 (2014).
Zerbo, O. et al. Maternal mid-pregnancy C-reactive protein and risk of autism spectrum disorders: the early markers for autism study. Transl. Psychiatry 6, e783 (2016).
Gilman, S. E. et al. Prenatal immune programming of the sex-dependent risk for major depression. Transl. Psychiatry 6, e822–e822 (2016).
Plant, D. T., Pawlby, S., Sharp, D., Zunszain, P. A. & Pariante, C. M. Prenatal maternal depression is associated with offspring inflammation at 25 years: a prospective longitudinal cohort study. Transl. Psychiatry 6, e936 (2016).
Kang, L. J. et al. Maternal depressive symptoms linked to reduced fecal Immunoglobulin A concentrations in infants. Brain Behav. Immun. 68, 123–131 (2018).
Krause, L., Einsle, F., Petzoldt, J., Wittchen, H. U. & Martini, J. The role of maternal anxiety and depressive disorders prior to and during pregnancy and perinatal psychopathological symptoms for early infant diseases and drug administration. Early Hum. Dev. 109, 7–14 (2017).
Ryan, J., Mansell, T., Fransquet, P. & Saffery, R. Does maternal mental well-being in pregnancy impact the early human epigenome? Epigenomics 9, 313–332 (e-pub ahead of print 3 January 2017).
Palma-Gudiel, H., Córdova-Palomera, A., Eixarch, E., Deuschle, M. & Fañanás, L. Maternal psychosocial stress during pregnancy alters the epigenetic signature of the glucocorticoid receptor gene promoter in their offspring: a meta-analysis. Epigenetics 10, 893–902 (2015).
Räikkönen, K. et al. Maternal depressive symptoms during pregnancy, placental expression of genes regulating glucocorticoid and serotonin function and infant regulatory behaviors. Psychol. Med. 45, 3217–3226 (2015).
Reynolds, R. M. et al. Maternal depressive symptoms throughout pregnancy are associated with increased placental glucocorticoid sensitivity. Psychol. Med. 45, 2023–30 (2015). (e-pub ahead of print 28 January 2015).
Mina, T. H., Räikkönen, K., Riley, S. C., Norman, J. E. & Reynolds, R. M. Maternal distress associates with placental genes regulating fetal glucocorticoid exposure and IGF2: role of obesity and sex. Psychoneuroendocrinology 59, 112–122 (e-pub 2015).
Suarez, A. et al. The epigenetic clock at birth: associations with maternal antenatal depression and child psychiatric problems. J. Am. Acad. Child Adolesc. Psychiatry 2018; 57(5),321–328.
Lahti-Pulkkinen, M. et al. Placental morphology is associated with maternal depressive symptoms during pregnancy and toddler psychiatric problems. Sci. Rep. 8, 1–12 (2018) (Article 791).
Shankar, R., Badker, R., Brain, U., Oberlander, T. F. & Misri, S. Predictors of recovery from depression and anxiety in women: a longitudinal study from childbirth to 6 years. Can. J. Psychiatry 62, 318–326 (2017).
Kong, L. L., Zhou, T. T., Wang, B. L., Gao, Z. B. & Wang, C. X. The risks associated with the use of lamotrigine during pregnancy. Int J. Psychiatry Clin. Pract. 22, 2–5 (2018).
Paulzen, M. et al. Pregnancy exposure to citalopram—therapeutic drug monitoring in maternal blood, amniotic fluid and cord blood. Prog. Neuropsychopharmacol. Biol. Psychiatry 79, 213–219 (2017).
Siu, A. L. et al. Screening for depression in adults. JAMA 315, 380 (2016).
van Ravesteyn, L. M., Lambregtse-van den Berg, M. P., Hoogendijk, W. J. G. & Kamperman, A. M. Interventions to treat mental disorders during pregnancy: a systematic review and multiple treatment meta-analysis. PLoS ONE 12, e0173397 (2017) (e collection 2017).
Knight, M., Nair, M., Derek Tuffnell, J. S. & Sara Kenyon, J. J. K. (eds). National Perinatal Epidemiology Unit. Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2013–15, 2014. (https://www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/Saving%20Lives%20Improving%20Mothers%20Care%20report%202014%20Full.pdf).
Ashford, M. T., Ayers, S. & Olander, E. K. Supporting women with postpartum anxiety: exploring views and experiences of specialist community public health nurses in the UK. Health Soc. Care Community 25, 1257–1264 (2017).
Lee, E. W., Denison, F. C., Hor, K. & Reynolds, R. M. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth 16, 38 (2016).
Nwebube, C., Glover, V. & Stewart, L. Prenatal listening to songs composed for pregnancy and symptoms of anxiety and depression: a pilot study. BMC Complement. Altern. Med. 17, 256 (2017).
Farshbaf-Khalili, A., Mohammad-Alizadeh, S., Farshbaf-Khalili, A., Mohammadi, F. & Ostadrahimi, A. Fish-oil supplementation and maternal mental health: a triple-blind, randomized controlled trial. Iran Red Crescent Med. J. 19, e36237 (2017) (e-pub a head of print 4 October 2016).
Sparling, T. M., Henschke, N., Nesbitt, R. C. & Gabrysch, S. The role of diet and nutritional supplementation in perinatal depression: a systematic review. Matern. Child Nutr. 13, (2017) (e-pub ahead of print 3 February 2016).
Acknowledgements
Funding for this review comes from an Academy of Finland Program Grant, European Commission Horizon 2020 Award SC1-2016-RTD-733280 for RECAP, European Commission Dynamics of Inequality Across the Life-course: structures and processes (DIAL) No. 724363 for PremLife, and the Signe and Ane Gyllenberg Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Robinson, R., Lahti-Pulkkinen, M., Heinonen, K. et al. Fetal programming of neuropsychiatric disorders by maternal pregnancy depression: a systematic mini review. Pediatr Res 85, 134–145 (2019). https://doi.org/10.1038/s41390-018-0173-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0173-y
This article is cited by
-
Participation in club sport in childhood is associated with mental health in preterm and term born adolescents
European Child & Adolescent Psychiatry (2024)
-
Die Eltern-Kind-Beziehung im Kontext elterlicher psychischer Erkrankung – Möglichkeiten zur Intervention
Der Nervenarzt (2023)
-
Prenatal risk factors and neonatal DNA methylation in very preterm infants
Clinical Epigenetics (2021)
-
Maternal stress or sleep during pregnancy are not reflected on telomere length of newborns
Scientific Reports (2020)
-
Silencing of maternal hepatic glucocorticoid receptor is essential for normal fetal development in mice
Communications Biology (2019)