Abstract
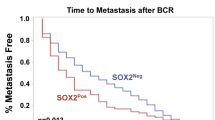
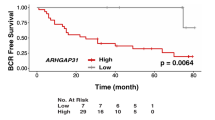
Prostate cancer (PCa) metastases are highly enriched with genomic alterations including a gain at the 16p13.3 locus, recently shown to be associated with disease progression and poor clinical outcome. ECI1, residing at the 16p13.3 gain region, encodes Δ3, Δ2-Enoyl-CoA Delta Isomerase 1 (ECI1), a key mitochondrial fatty acid β-oxidation enzyme. Although deregulated mitochondrial fatty acid β-oxidation is known to drive PCa pathogenesis, the role of ECI1 in PCa is still unknown. We investigated the impacts of ECI1 on PCa phenotype in vitro and in vivo by modulating its expression in cell lines and assessed the clinical implications of its expression in human prostate tissue samples. In vitro, ECI1 overexpression increased PCa cell growth while ECI1 deficiency reduced its growth. ECI1 also enhanced colony formation, cell motility, and maximal mitochondrial respiratory capacity. In vivo, PCa cells stably overexpressing ECI1 injected orthotopically in nude mice formed larger prostate tumors with higher number of metastases. Immunohistochemistry analysis of the human tissue microarray representing 332 radical prostatectomy cases revealed a stronger ECI1 staining in prostate tumors compared to corresponding benign tissues. ECI1 expression varied amongst tumors and was higher in cases with 16p13.3 gain, high Gleason grade, and advanced tumor stage. ECI1 overexpression was a strong independent predictor of biochemical recurrence after adjusting for known clinicopathologic parameters (hazard ratio: 3.65, P < 0.001) or the established CAPRA-S score (hazard ratio: 3.95, P < 0.001). ECI1 overexpression was also associated with significant increased risk of distant metastasis and reduced overall survival. Overall, this study demonstrates the functional capacity of ECI1 in PCa progression and highlights the clinical implication of ECI1 as a potential target for the management of PCa.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA: a cancer journal for clinicians. 2020;70:7–30.
Yuan X, Balk SP. Mechanisms mediating androgen receptor reactivation after castration. Urologic Oncol. 2009;27:36–41.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011;144:646–74.
Jones RG, Thompson CB. Tumor suppressors and cell metabolism: a recipe for cancer growth. Genes Dev. 2009;23:537–48.
Liu Y. Fatty acid oxidation is a dominant bioenergetic pathway in prostate cancer. Prostate Cancer Prostatic Dis. 2006;9:230–4.
Warburg O. On respiratory impairment in cancer cells. Science 1956;124:269–70.
Carracedo A, Cantley LC, Pandolfi PP. Cancer metabolism: fatty acid oxidation in the limelight. Nat Rev Cancer 2013;13:227–32.
Deep G, Schlaepfer IR. Aberrant lipid metabolism promotes prostate cancer: role in cell survival under hypoxia and extracellular vesicles biogenesis. Int J Mol Sci. 2016;17:1061
Zadra G, Photopoulos C, Loda M. The fat side of prostate cancer. Biochim et Biophys Acta 2013;1831:1518–32.
De Schrijver E, Brusselmans K, Heyns W, Verhoeven G, Swinnen JV. RNA interference-mediated silencing of the fatty acid synthase gene attenuates growth and induces morphological changes and apoptosis of LNCaP prostate cancer cells. Cancer Res. 2003;63:3799–804.
Zadra G, Ribeiro CF, Chetta P, Ho Y, Cacciatore S, Gao X, et al. Inhibition of de novo lipogenesis targets androgen receptor signaling in castration-resistant prostate cancer. Proc Natl Acad Sci USA 2019;116:631–40.
Houten SM, Wanders RJ. A general introduction to the biochemistry of mitochondrial fatty acid beta-oxidation. J Inherit Metab Dis. 2010;33:469–77.
Itkonen HM, Brown M, Urbanucci A, Tredwell G, Ho Lau C, Barfeld S, et al. Lipid degradation promotes prostate cancer cell survival. Oncotarget 2017;8:38264–75.
Schlaepfer IR, Rider L, Rodrigues LU, Gijon MA, Pac CT, Romero L, et al. Lipid catabolism via CPT1 as a therapeutic target for prostate cancer. Mol Cancer Ther. 2014;13:2361–71.
Gurvitz A, Wabnegger L, Yagi AI, Binder M, Hartig A, Ruis H, et al. Function of human mitochondrial 2,4-dienoyl-CoA reductase and rat monofunctional Delta3-Delta2-enoyl-CoA isomerase in beta-oxidation of unsaturated fatty acids. Biochem J. 1999;344:903–14.
Lee SH, Lee SK, Paik D, Min KJ. Overexpression of fatty-acid-beta-oxidation-related genes extends the lifespan of Drosophila melanogaster. Oxid Med Cell Longev. 2012;2012:854502.
Rasmussen AL, Diamond DL, McDermott JE, Gao X, Metz TO, Matzke MM, et al. Systems virology identifies a mitochondrial fatty acid oxidation enzyme, dodecenoyl coenzyme A delta isomerase, required for hepatitis C virus replication and likely pathogenesis. J Virol. 2011;85:11646–54.
Janssen U, Stoffel W. Disruption of mitochondrial beta -oxidation of unsaturated fatty acids in the 3,2-trans-enoyl-CoA isomerase-deficient mouse. J Biol Chem. 2002;277:19579–84.
Lapointe J, Li C, Giacomini CP, Salari K, Huang S, Wang P, et al. Genomic profiling reveals alternative genetic pathways of prostate tumorigenesis. Cancer Res. 2007;67:8504–10.
Choucair KA, Guerard KP, Ejdelman J, Chevalier S, Yoshimoto M, Scarlata E, et al. The 16p13.3 (PDPK1) Genomic Gain in Prostate Cancer: A Potential Role in Disease Progression. Transl Oncol. 2012;5:453–60.
Bramhecha YM, Guerard KP, Rouzbeh S, Scarlata E, Brimo F, Chevalier S, et al. Genomic Gain of 16p13.3 in Prostate Cancer Predicts Poor Clinical Outcome after Surgical Intervention. Mol Cancer Res. 2018;16:115–23.
Lapointe J, Li C, Higgins JP, Van De Rijn M, Bair E, Montgomery K, et al. Gene expression profiling identifies clinically relevant subtypes of prostate cancer. Proc Natl Acad Sci USA. 2004;101:811–6.
Poluri RTK, Beauparlant CJ, Droit A, Audet-Walsh E. RNA sequencing data of human prostate cancer cells treated with androgens. Data Brief. 2019;25:104372.
Poluri RTK, Paquette V, Allain EP, Lafront C, Joly-Beauparlant C, Weidmann C, et al. KLF5 and NFYA factors as novel regulators of prostate cancer cell metabolism. Endocr-Relat Cancer. 2021;28:257–71.
Cai QY, Yu P, Besch-Williford C, Smith CJ, Sieckman GL, Hoffman TJ, et al. Near-infrared fluorescence imaging of gastrin releasing peptide receptor targeting in prostate cancer lymph node metastases. Prostate 2013;73:842–54.
Tuomela JM, Valta MP, Vaananen K, Harkonen PL. Alendronate decreases orthotopic PC-3 prostate tumor growth and metastasis to prostate-draining lymph nodes in nude mice. BMC Cancer 2008;8:81.
Aasmundstad TA, Haugen OA, Johannesen E, Hoe AL, Kvinnsland S. Oestrogen receptor analysis: correlation between enzyme immunoassay and immunohistochemical methods. J Clin Pathol. 1992;45:125–9.
Wang S, Shi X, Wei S, Ma D, Oyinlade O, Lv SQ, et al. Kruppel-like factor 4 (KLF4) induces mitochondrial fusion and increases spare respiratory capacity of human glioblastoma cells. J Biol Chem. 2018;293:6544–55.
Pfleger J, He M, Abdellatif M. Mitochondrial complex II is a source of the reserve respiratory capacity that is regulated by metabolic sensors and promotes cell survival. Cell Death Dis. 2015;6:e1835.
Teh JT, Zhu WL, Newgard CB, Casey PJ, Wang M. Respiratory Capacity and Reserve Predict Cell Sensitivity to Mitochondria Inhibitors: Mechanism-Based Markers to Identify Metformin-Responsive Cancers. Mol Cancer Ther. 2019;18:693–705.
Oliva CR, Nozell SE, Diers A, McClugage SG 3rd, Sarkaria JN, Markert JM, et al. Acquisition of temozolomide chemoresistance in gliomas leads to remodeling of mitochondrial electron transport chain. J Biol Chem. 2010;285:39759–67.
Audet-Walsh E, Dufour CR, Yee T, Zouanat FZ, Yan M, Kalloghlian G. et al. Nuclear mTOR acts as a transcriptional integrator of the androgen signaling pathway in prostate cancer. Genes Dev.2017;31:1228–42.
Pougovkina O, te Brinke H, Ofman R, van Cruchten AG, Kulik W, Wanders RJ, et al. Mitochondrial protein acetylation is driven by acetyl-CoA from fatty acid oxidation. Hum Mol Genet. 2014;23:3513–22.
Wong BW, Wang X, Zecchin A, Thienpont B, Cornelissen I, Kalucka J, et al. The role of fatty acid beta-oxidation in lymphangiogenesis. Nature 2017;542:49–54.
McDonnell E, Crown SB, Fox DB, Kitir B, Ilkayeva OR, Olsen CA, et al. Lipids Reprogram Metabolism to Become a Major Carbon Source for Histone Acetylation. Cell Rep. 2016;17:1463–72.
Park JH, Vithayathil S, Kumar S, Sung PL, Dobrolecki LE, Putluri V, et al. Fatty Acid Oxidation-Driven Src Links Mitochondrial Energy Reprogramming and Oncogenic Properties in Triple-Negative Breast Cancer. Cell Rep. 2016;14:2154–65.
Joshi M, Stoykova GE, Salzmann-Sullivan M, Dzieciatkowska M, Liebman LN, Deep G, et al. CPT1A Supports Castration-Resistant Prostate Cancer in Androgen-Deprived Conditions. Cells. 2019;8.
Lapointe J, Malhotra S, Higgins JP, Bair E, Thompson M, Salari K, et al. hCAP-D3 Expression Marks a Prostate Cancer Subtype With Favorable Clinical Behavior and Androgen Signaling Signature. Am J Surg Pathol. 2008;32:205–9.
Audet-Walsh E, Yee T, McGuirk S, Vernier M, Ouellet C, St-Pierre J, et al. Androgen-Dependent Repression of ERRgamma Reprograms Metabolism in Prostate Cancer. Cancer Res. 2017;77:378–89.
van Weeghel M, te Brinke H, van Lenthe H, Kulik W, Minkler PE, Stoll MS, et al. Functional redundancy of mitochondrial enoyl-CoA isomerases in the oxidation of unsaturated fatty acids. Faseb J. 2012;26:4316–26.
Zhang D, Yu W, Geisbrecht BV, Gould SJ, Sprecher H, Schulz H. Functional characterization of Delta3,Delta2-enoyl-CoA isomerases from rat liver. J Biol Chem. 2002;277:9127–32.
Higgins LH, Withers HG, Garbens A, Love HD, Magnoni L, Hayward SW, et al. Hypoxia and the metabolic phenotype of prostate cancer cells. Biochim et Biophys Acta. 2009;1787:1433–43.
Dueregger A, Schopf B, Eder T, Hofer J, Gnaiger E, Aufinger A, et al. Differential Utilization of Dietary Fatty Acids in Benign and Malignant Cells of the Prostate. PLoS ONE 2015;10:e0135704.
Flaig TW, Salzmann-Sullivan M, Su LJ, Zhang Z, Joshi M, Gijon MA, et al. Lipid catabolism inhibition sensitizes prostate cancer cells to antiandrogen blockade. Oncotarget 2017;8:56051–65.
Qu Q, Zeng F, Liu X, Wang Q, Deng F. Fatty acid oxidation and carnitine palmitoyltransferase I: emerging therapeutic targets in cancer. Cell Death Dis. 2017;7:e2226.
Mertins P, Mani DR, Ruggles KV, Gillette MA, Clauser KR, Wang P, et al. Proteogenomics connects somatic mutations to signalling in breast cancer. Nature 2016;534:55–62.
Qian J, Hassanein M, Hoeksema MD, Harris BK, Zou Y, Chen H, et al. The RNA binding protein FXR1 is a new driver in the 3q26-29 amplicon and predicts poor prognosis in human cancers. Proc Natl Acad Sci USA. 2015;112:3469–74.
Pfaffl MW, Horgan GW, Dempfle L. Relative expression software tool (REST) for group-wise comparison and statistical analysis of relative expression results in real-time PCR. Nucleic Acids Res. 2002;30:e36.
Rogers GW, Nadanaciva S, Swiss R, Divakaruni AS, Will Y. Assessment of fatty acid beta oxidation in cells and isolated mitochondria. Curr Protoc Toxicol. 2014;60:25 3 1–19.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. REporting recommendations for tumor MARKer prognostic studies (REMARK). Nat Clin Pract Urol. 2005;2:416–22.
Bramhecha YM, Rouzbeh S, Guerard KP, Scarlata E, Brimo F, Chevalier S, et al. The combination of PTEN deletion and 16p13.3 gain in prostate cancer provides additional prognostic information in patients treated with radical prostatectomy. Mod Pathol. 2019;32:128–38.
Punnen S, Freedland SJ, Presti JC, Aronson WJ, Terris MK, Kane CJ, et al. Multi-institutional validation of the CAPRA-S score to predict disease recurrence and mortality after radical prostatectomy. Eur Urol. 2014;65:1171–7.
Choucair K, Ejdelman J, Brimo F, Aprikian A, Chevalier S, Lapointe J. PTEN genomic deletion predicts prostate cancer recurrence and is associated with low AR expression and transcriptional activity. BMC Cancer. 2012;12:543.
Budczies J, Klauschen F, Sinn BV, Gyorffy B, Schmitt WD, Darb-Esfahani S, et al. Cutoff Finder: a comprehensive and straightforward Web application enabling rapid biomarker cutoff optimization. PLoS ONE 2012;7:e51862.
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87.
Acknowledgements
Funding for this research was provided by the US Department of Defense (DoD, W81XWH-11-1-0638), Prostate Cancer Canada (D2019-2192), and the Fonds de Recherche du Québec-Santé (FRQS, Chercheur boursier) to JL. The Canadian Institutes of Health Research (CIHR) Foundation Grant to VG, CIHR System Biology and McGill Division of Urology studentships to YB, and 100 Days Across Canada Urology Studentship Program on Prostate Cancer to OK also supported the study. We are grateful to Mathieu Simard from the Small Animal Imaging Labs (SAIL) and the personnel of the Animal Resources Division of Research Institute of the McGill University Health Centre for their precious help.
Funding
US Department of Defense (DoD, W81XWH-11-1-0638), Prostate Cancer Canada (D2019-2192), the Fonds de Recherche du Québec-Santé (FRQS, Chercheur boursier) to JL. Canadian Institutes of Health Research (CIHR) Foundation Grant to VG, CIHR System Biology and McGill Division of Urology studentships to YB, and 100 Days Across Canada Urology Studentship Program on Prostate Cancer to OK.
Author information
Authors and Affiliations
Contributions
Conception and design: YB, KPG, EAW, JL Development of methodology: YB, KPG, EAW, JL Acquisition of data: YB, KPG, EAW, OK, EP, ES, LH, FB, MD, AA, SC, VG, JL. Analysis and interpretation of data: YB, KPG, EAW, SR, OK, FB, SC, VG, JL. Writing, review, and/or revision of the paper: YB, KPG, EAW, ES, FB, MD, AA, SC, VG, JL. Administrative, technical, or material support: ES, LH, AA Study supervision: JL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bramhecha, Y.M., Guérard, KP., Audet-Walsh, É. et al. Fatty acid oxidation enzyme Δ3, Δ2-enoyl-CoA isomerase 1 (ECI1) drives aggressive tumor phenotype and predicts poor clinical outcome in prostate cancer patients. Oncogene 41, 2798–2810 (2022). https://doi.org/10.1038/s41388-022-02276-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-022-02276-z
This article is cited by
-
Ferroptosis landscape in prostate cancer from molecular and metabolic perspective
Cell Death Discovery (2023)