Abstract
Peptide-based T cell vaccines targeting the conserved epitopes of influenza virus can provide cross-protection against distantly related strains, but they are generally not immunogenic. Foreign antigen-specific regulatory T (Treg) cells are induced under subimmunogenic conditions peripherally, although their development and role in vaccine-mediated antiviral immunity is unclear. Here, we demonstrated primary vaccination with peptides alone significantly induced antigen-specific Foxp3+ Treg cells, which were further expanded by repeated vaccination with unadjuvanted peptides. Certain adjuvants, including CpG, suppressed the induction and expansion of antigen-specific Treg cells by peptide vaccination. Interestingly, secondary influenza virus infection significantly increased the frequency of preexisting antigen-specific Treg cells, although primary infection barely induced them. Importantly, specific depletion of vaccine-induced antigen-specific Treg cells promoted influenza viral clearance, indicating their inhibitory role in vivo. Immunization with CpG-adjuvanted peptides by the subcutaneous prime–intranasal-boost strategy restricted the recruitment and accumulation of antigen-specific Treg cells in lung, and stimulated robust T cell immunity. Finally, subcutaneous prime–intranasal-boost immunization with CpG-adjuvanted peptides or whole-inactivated influenza vaccines protected mice from heterosubtypic influenza virus infection. In conclusion, antigen-specific Treg cells induced by peptide vaccines attenuate the antiviral immunity against influenza virus infection. CpG-adjuvanted peptide vaccines provide heterosubtypic influenza protection probably by inhibiting Treg development and enhancing T cell immunity.
Similar content being viewed by others
Introduction
Vaccination is the most cost-effective strategy to prevent influenza viral infections. Current inactivated influenza vaccines inducing neutralizing antibodies are effective against strain-matched circulating influenza virus, but fail to prevent antigenically distinct viral strains generated by antigenic drift and shift.1 Influenza vaccines thus require annual reformulation to keep pace with viral mutations. T cell immunity has been suggested to provide cross-protection against influenza viruses of different strains and subtypes, because T cells can recognize epitopes across the entire virus proteome, particularly the epitopes derived from the conserved internal influenza viral proteins.2,3 Two recent studies have demonstrated that preexisting T cell responses were well correlated with reduced severity of influenza disease in humans.4,5 However, T cell immunity induced by natural influenza virus infection may not be durable and wane in efficacy to minimal levels within years.6
Peptide-based vaccines targeting conserved epitopes of internal influenza viral proteins can activate specific antiviral T cell immunity, and hold the promise to provide protection against a broad spectrum of influenza viruses, both seasonal and pandemic.7,8 Nevertheless, development of an efficacious peptide-based T cell vaccine against viral infection has been challenging.3,9 The immunogenicity of peptide vaccines is far from optimal, and needs to overcome several regulatory mechanisms, including regulatory T (Treg) cells.
Treg cells play a major role in regulating exuberant immune responses and are suggested to dampen the protective immunity induced by infection and vaccination. CD4+Foxp3+ Treg cells are so far best characterized.10,11 In addition to the thymus-derived Treg cells that target self-antigens, Treg cells are also differentiated from naïve CD4+ T cells encountering foreign antigens under a tolerizing or subimmunogenic condition in the peripheral tissues, termed peripherally- induced Treg cells.12 Recently, the role of pathogen-specific Treg cells in regulating antiviral immune responses has emerged. Previous studies demonstrated that pathogen-specific Treg cells are activated and expanded upon acute viral infections, and form a pool of memory Treg cells after the resolution of infections.13 Furthermore, it has been claimed that acute influenza viral infection stimulated viral antigen-specific Treg cells, which contributed to the attenuation of antiviral T cell immunity and suppression of excessive immunopathological conditions.14,15 However, previous studies investigated this issue by non-specific depletion of polyclonal Treg cells rather than specific depletion of pathogen-specific Treg cells, and thus failed to convincingly clarify the role of the pathogen-specific Treg cells in vivo.15,16 Moreover, whether and how vaccine-induced viral antigen-specific Treg cells respond to acute influenza virus infection and affect the antiviral immunity remains unclear.
Adjuvants can enhance the immunogenicity of T cell vaccines through different mechanisms, including restricting the development of Treg cells, and promoting the T cell immunity.17,18 Current clinically licensed adjuvants, like aluminum salts, can enhance antibody responses, but plays a limited role in promoting T cell immunity.19 Toll-like receptor (TLR) agonists, such as lipopolysaccharide (LPS) (TLR-4), R848 (TLR-7/8), and CpG ODN 1826 (CpG) (TLR-9), have been reported to prevent the expansion of Treg cells.20 Suppression of Treg cells by adjuvants may constitute an ideal vaccination strategy for generation of protective antiviral T cell immunity.
The priming and boosting strategy is demonstrated to be required to establish optimal T cell immunity.21 However, current human inactivated influenza vaccines are given through intradermal or intramuscular injection, and thus fail to generate robust anti-influenza T cell immunity in the lung. It has been shown that the local boosting strategy can help establish robust memory T cells in peripheral tissues.21,22,23 In addition, robust resident T cell immunity in lung is critical to protect from acute influenza viral infection.24,25,26 Nevertheless, little is known about the effects of pulmonary boosting vaccines with adjuvants on local development of antigen-specific Treg cells in lung.
In this study, we utilized an influenza virus infection mouse model with the adoptive transfer of T cells bearing the transgenic TCR (OT-II T cells), which allows for convenient monitor and manipulation of vaccine-induced antigen-specific Treg cells in vivo. Using this model, we clearly demonstrated that unadjuvanted peptide vaccines induced a significant portion of antigen-specific Treg cells, which were indeed functionally suppressive and could be further expanded upon secondary vaccination and acute influenza viral infection. Specific depletion of antigen-specific Treg cells or inhibition of their induction by the vaccine adjuvant CpG promoted viral clearance in acute influenza virus infection, suggesting their role in antagonizing antiviral immunity.
Results
Unadjuvanted peptide vaccines induce antigen-specific Treg cells in a dose-dependent manner
To investigate the role of antigen-specific Treg cells induced by vaccination, we established an influenza vaccination and infection mouse model that allows for tracking of vaccine-induced antigen-specific Treg cells in vivo. We utilized TCR-transgenic OT-II mice whose CD4+OT-II T cells specifically recognize ovalbumin (OVA) OT-II peptide (OVA323–339) presented by H-2IAb. CD45.1+CD25− OT-II T cells isolated from naïve CD45.1+ OT-II transgenic mice were adoptively transferred into wild-type (WT) CD45.2+ C57BL/6 (B6) mice, which were then subcutaneously primed with different doses of OVA OT-II (OVA323–339) peptide (Fig. 1a). We found that vaccination with the OVA OT-II peptide alone induced a significant proportion of Foxp3+ Treg cells among the adoptively transferred OT-II T cells, up to 32% in spleens and 45% in inguinal lymph nodes (LNs), by the increase of the peptide vaccine dose up to 10 and 50 μg, respectively (Fig. 1b, c). However, further increase of the peptide dose to 100 μg reduced the level of vaccine-induced OT-II Treg cells to 14.4% and 24.0% in spleens and inguinal LNs, respectively (Fig. 1b, c). The number of OT-II Treg cells in spleens of mice immunized by 100 μg OT-II peptide was significantly lower than that in mice immunized by 10 μg OT-II peptide (Fig. 1d). In contrast, immunization with phosphate-buffered saline (PBS) or an irrelevant peptide NP366–374 derived from PR8 NP protein barely induced OT-II Treg cells in a dose up to 50 μg, suggesting this Treg induction was antigen-specific. Because the number of adoptively transferred OT-II T cells was unphysiologically high (3–4 × 106 cells), we also adoptively transferred 10-fold fewer (3 × 105) CD45.1+CD25− OT-II T cells to repeat this experiment. Similarly, 10 μg OT-II peptide induced the highest number and percentage of Treg cells in spleens and LNs, but higher doses of OT-II peptide (50 and 100 μg) reduced Treg induction (Supplementary Figure 1). Taken together, these results indicate that peptide vaccines induce antigen-specific Treg cells in a dose-dependent manner, but a high dose of peptide vaccine overcomes its tolerizing effect.
The dose effect of peptide vaccination on induction of antigen-specific Treg cells. a Schematic representation of the experimental protocol used for immunization of mice. C57BL/6 (CD45.2) mice were adoptively transferred with 3–4 × 106 CD45.1+CD25−OT-II T cells isolated from CD45.1 × OT-II mice one day before vaccination with OVA OT-II (OVAII) peptide. At day 0, mice were s.c. immunized with PBS control, indicated doses of OVA OT-II peptide, or the control NP366–374 peptide. At day 13 post immunization, mice were sacrificed for analysis of the antigen-specific Treg cells in spleens and inguinal LNs. b–d The CD45.1+CD4+Foxp3+ OT-II T cells in spleens and inguinal LNs of the immunized mice. CD45.1+CD4+ donor cells were gated to analyze the percentage of CD45.1+Foxp3+ OT-II T cells. Cells in CD45.1+Foxp3+ regions are considered antigen-specific Treg cells. b Representative flow cytometric plots displaying CD45.1+CD4+Foxp3+ OT-II antigen-specific Treg cells. c Individual percentages of CD45.1+CD4+Foxp3+ OT-II T cells with mean ± SE (error bars) (n ≧ 4 mice per group compiled from two independent experiments). d The total number of CD45.1+CD4+Foxp3+ OT-II T cells with mean ± SE. e Summary results of the suppressive assay for vaccine-induced antigen-specific T cells. AT adoptive transfer, OVAII OVA OT-II peptide, 1° imm primary immunization, d.p.i. days post immunization. *P < 0.05; **P < 0.005; ***P < 0.001 (Student’s t test)
To examine whether these vaccine-induced antigen-specific Foxp3+ Treg cells were suppressive, we isolated CD4+CD25-GFP− OT-II T cells from naïve Thy1.1/Thy1.2 × Foxp3gfp × OT-II mice and adoptively transferred them to WT B6 mice receiving OT-II peptide immunization. We demonstrated that CD4+CD25+GFP+ OT-II Treg cells (vaccine-induced Treg) isolated from these OT-II peptide-immunized mice could suppress T cell proliferation in vitro (Fig. 1e and Supplemental Figure 2).
Adjuvants antagonize the induction of antigen-specific Treg cells by peptide vaccine priming
We further determined the effects of adjuvants on the induction of Treg cells by peptide vaccines. CD45.1+CD4+CD25− OT-II T cells were adoptively transferred into WT CD45.2+ B6 mice, which were then subcutaneously (s.c.) immunized with 10 μg OVA OT-II peptide combined with different adjuvants (Fig. 2a), including CpG, complete Freud’s adjuvant (CFA), alum, R848, and LPS (Fig. 2b, c). Compared with the control group immunized with OVA OT-II peptide alone, the mice immunized with all the adjuvants used here except alum had significantly reduced the percentage of vaccine-induced OT-II Treg cells (p < 0.001). Notably, in the group treated by OVA OT-II peptide plus CpG, the percentage of vaccine-induced OT-II Treg cells was significantly suppressed to <2% (Fig. 2b, c). Interestingly, alum adjuvant did not suppress the induction of Treg cells by peptide vaccination. We also examined whether T cell proliferation affects Treg induction. Thy1.1/1.2CD4+CD25- OT-II T cells were stained with violet proliferation dye 450 and adoptively transferred into WT Thy1.2+ B6 mice, which were then immunized with 10 μg OVA OT-II peptide with adjuvants. OT-II peptide alone induced a larger number and a higher proportion of OT-II Treg cells than OT-II peptides adjuvanted with CpG, R848, and LPS (Fig. 2d, f). More extensive proliferation of OT-II non-Treg cells was also observed in mice immunized by OT-II peptide adjuvanted with CpG, CFA, R848, and LPS (Fig. 2d, f). In addition, the non-Treg OT-II CD4+ T cells in the mice immunized by CFA-adjuvanted OT-II peptide expressed significantly higher levels of interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α) than those in the unadjuvanted controls (Fig. 2e, g). Collectively, primary peptide vaccines combined with certain adjuvants, particularly with CpG, but not alum, significantly suppress the induction of vaccine-induced antigen-specific Treg cells.
Effects of adjuvants on the development of antigen-specific Treg cells in primary and secondary vaccination. a Schematic representation of the experimental protocol used for primary immunization by OVA OT-II (OVAII) peptide combined with different adjuvants. C57BL/6 mice with adoptive transfer of CD45.1+CD25−OT-II T cells received primary s.c. immunization by OVA OT-II peptide (10 μg) alone or combined with indicated adjuvants CpG, CFA, alum, R848, or LPS. b, c CD45.1+CD4+Foxp3+ OT-II T cells in the spleens and inguinal LNs of the immunized mice. b Representative flow cytometric plots displaying CD45.1+CD4+Foxp3+ OT-II antigen-specific Treg cells. c Individual percentages of CD45.1+CD4+Foxp3+ OT-II T cells with mean ± SE (n ≧ 7 mice per group compiled from three independent experiments). d–g Thy1.1/1.2CD4+CD25- OT-II T cells were stained with violet proliferation dye 450 (VPD450) and adoptively transferred into WT Thy1.2+ B6 mice, which were then immunized with 10 μg OVA OT-II peptide alone or with indicated adjuvants. Representative flow cytometric plots displaying (d) proliferation (CFSE dilution) and (e) IFN-γ and TNF-α production of transferred Thy1.1+ OT-II T cells were shown. f Individual percentages and total numbers of Thy1.1+CD4+GFP+ OT-II Treg cells with mean ± SE and total numbers of Thy1.1+CD4+GFP− OT-II non-Treg cells with mean ± SE. g Individual percentages of Thy1.1+CD4+ IFN-γ+ and TNF-α+ OT-II T cells with mean ± SE (n ≧ 7 mice per group compiled from three independent experiments). h Schematic representation of the experimental protocol used for secondary vaccination by OVA OT-II (OVAII) peptide alone or combined with different adjuvants. Mice were primarily s.c. immunized with OVA OT-II peptide (10 μg), and secondary s.c. immunized by either OVA OT-II peptide (10 μg) alone, adjuvants (CpG or alum) alone, or OVA OT-II peptide plus adjuvants (CpG or alum). The antigen-specific Treg cells in the spleens and inguinal LNs were analyzed. i, j CD45.1+CD4+Foxp3+ OT-II T cells in the spleens and inguinal LNs of the immunized mice. i Data are representative flow cytometric plots. j Individual percentages of CD45.1+CD4+Foxp3+ OT-II T cells with mean ± SE (n ≧ 7 mice per group compiled from three independent experiments). *P < 0.05; ***P < 0.001 (Student’s t test). NS not significant
Adjuvants restrict the expansion of preexisting vaccine-induced Treg cells
Next, we investigated the effects of adjuvants on the preexisting vaccine-induced antigen-specific Treg cells after secondary immunization. Again, WT B6 mice with adoptive transfer of CD45.1+CD25− OT-II T cells were immunized subcutaneously with OVA OT-II peptide alone, and, subsequently, were either injected with PBS or immunized subcutaneously with OVA OT-II peptide alone or in combination with CpG or alum (Fig. 2h). The percentage of OT-II Treg cells in the PBS control mice was 24.9% in spleens and 32.8% in inguinal LNs, similar to that in mice with primary vaccination by unadjuvanted OVA OT-II peptides (Fig. 2j, lane 1 vs. Fig. 2c, lane 2). Interestingly, secondary vaccination with OVA OT-II peptide alone further increased the percentage of OT-II Treg cells to 55.5% in spleens and 55.4% in inguinal LNs, approximately twofold over that of the PBS control. In contrast, the CpG-adjuvanted OT-II peptide vaccine did not increase the percentage of OT-II Treg cells and even reduced it in inguinal LNs (Fig. 2i, j). Moreover, the percentage of vaccine-induced Treg cells of mice receiving OVA OT-II peptide plus alum was similar in spleens, but significantly higher in inguinal LNs, compared to those receiving the OVA OT-II peptide with CpG (Fig. 2j). In addition, following primary immunization by unadjuvanted OT-II peptide, the mice secondarily immunized by OT-II peptide had significantly more OT-II Treg cells in the spleen than those receiving PBS, CpG-adjuvanted OT-II peptide or alum-adjuvanted OT-II peptide (Supplementary Fig. 3). Collectively, these results indicate that vaccine-induced antigen-specific Treg cells remain relatively stable for at least 1 month, and repeated vaccination expands the preexisting antigen-specific Treg cells. Compared with alum, the CpG adjuvant has greater ability to restrict the expansion of preexisting antigen-specific Treg cells.
Influenza virus infection promotes the expansion of preexisting vaccine-induced antigen-specific Treg cells
We next asked how these vaccine-induced antigen-specific Treg cells respond during the acute influenza virus infection. We generated the genetically modified PR8-NA-OVAII. We showed that PR8-NA-OVAII infection, but not PR8, specifically drove the proliferation of OT-II T cells, indicating proper presentation of the epitope OVA323–339 in PR8-NA-OVAII-infected mice (Supplementary Fig. 4). To determine the effect of influenza virus infection on vaccine-induced antigen-specific Treg cells, WT CD45.2+ B6 mice were adoptively transferred with CD45.1+CD25− OT-II T cells, and immunized subcutaneously with OVA OT-II peptide or treated with PBS as the unimmunized control. Mice were then infected with low and high doses of PR8-NA-OVAII virus (5 plaque-forming unit (PFU) and 80 PFU) (Fig. 3a). In the unvaccinated control mice, low percentage of antigen-specific OT-II Treg cells were detected (Fig. 3b, c), indicating that primary influenza virus infection did not simulate significant expansion of viral antigen-specific Treg cells. Surprisingly, in mice primarily vaccinated by OVA OT-II peptide, the proportion of OT-II Treg cells were significantly increased upon subsequent influenza viral infection (Fig. 3b, c). The percentage of OT-II Treg cells in draining lymph nodes (dLNs) of the low-dose (5 PFU) group was significantly higher than that in mice with primary vaccination by OT-II peptide alone (Fig. 3c, dLN lane 2 vs. Fig. 2c, LN lane 2, 41.2 vs. 31.6%, P < 0.05). The expansion of vaccine-induced preexisting antigen-specific Treg cells in the high-dose (80 PFU) group was even greater than that in the low-dose group (5 PFU) (Fig. 3b, c). In addition, the number of OT-II Treg cells in the spleens of high-dose group was also significantly higher than that in spleens of the OT-II peptide/PBS immunization group indicated in Fig. 2j (data now shown), suggesting that influenza virus infection drives the expansion of OT-II Treg cells.
The response of preexisting vaccine-induced antigen-specific Treg cells to acute influenza virus infection. a Schematic representation of the experimental protocol. C57BL/6 mice with adoptive transfer of CD45.1+CD25− OT-II T cells were primarily s.c. immunized by OVA OT-II peptide (10 μg) alone or PBS and subsequently i.n. infected by 5 PFU or 80 PFU of PR8-NA-OVAII virus (PR8-OVAII). b, c The CD45.1+CD4+Foxp3+ OT-II T cells in spleens, dLNs, and lungs of the immunized mice. b Representative flow cytometric plots displaying CD45.1+CD4+Foxp3+ OT-II antigen-specific Treg cells. c Graphs for spleens and dLNs show individual percentages of CD45.1+CD4+Foxp3+ OT-II T cells with mean ± SE (n ≧ 6 mice per group complied from three independent experiments). The graph for lung shows the representative of three independent experiments, in which each sample represented a pool of cells from three vaccinated mice. d, e C57BL/6 mice with adoptive transfer of CD45.1+CD25− OT-II T cells were primarily s.c. immunized by OVA OT-II peptide (10 μg) with or without CpG, and subsequently infected by 80 PFU of PR8-OVAII. d Representative flow cytometric plots displaying CD45.1+CD4+Foxp3+ OT-II antigen-specific Treg cells. e Graphs for spleens and dLNs show individual percentages (upper panel) and numbers (lower panel) of CD45.1+CD4+Foxp3+ OT-II T cells with mean ± SE (n ≧ 4 mice per group complied from two independent experiments). For the graph of lung, data are representative of three independent experiments, in which each sample represented a pool of cells from three vaccinated mice. *P < 0.05; **P < 0.005; ***P < 0.001 (Student’s t test)
We further asked whether primary immunization response affected the subsequent expansion of antigen-specific Treg cells following secondary influenza virus infections. WT CD45.2+ B6 mice with adoptive transfer of CD45.1+CD25− OT-II T cells were primarily s.c. immunized with OVA OT-II peptide alone or adjuvanted with CpG, and subsequently infected with 80 PFU of PR8-NA-OVAII virus. Interestingly, we found that primary vaccination by OVA OT-II peptide with CpG adjuvant inhibited the induction of OT-II Treg cells and significantly reduced the percentage and number of the vaccine-induced antigen-specific Treg cells upon subsequent influenza virus infection (Fig. 3d, e). Although acute influenza virus infection only induces minimal level of antigen-specific Treg cells, it significantly drives the expansion of preexisting antigen-specific Treg cells in a dose-dependent manner. However, suppression of vaccine-induced Treg cells by CpG adjuvant in primary vaccination can significantly reduce further expansion of these Treg cells by subsequent influenza virus infection.
Depletion of vaccine-induced antigen-specific Treg cells enhances antiviral immunity against influenza virus infection
As we have shown previously, vaccine-induced antigen-specific Treg cells exhibited suppressive activity in vitro (Fig. 1e). We further investigated whether vaccine-induced antigen-specific Treg cells can suppress antiviral immunity in vivo. Previous studies have demonstrated that depletion of all polyclonal Foxp3+ Treg cells can enhance antiviral immunity.16 However, such approach fails to determine the role of antigen-specific Treg cells in acute viral infections. To investigate whether vaccine-induced antigen-specific Treg cells can affect antiviral immunity against influenza viral infection in vivo, we took advantage of DEREG mice, in which fully functional Foxp3+ Treg cells express diphtheria toxin receptor (DTR)-enhanced green fluorescent protein (eGFP) transgene, which can be specifically depleted by administration of diphtheria toxin (DT).27 We first generated OT-II × DEREG mice by cross-breeding OT-II mice with DEREG mice. CD45.1+ mice were adoptively transferred with CD45.2+CD25−Foxp3-GFP−OT-II T cells isolated from OT-II × DEREG mice, and were then immunized with two doses of 10 μg OVA OT-II peptide at days 0 and 21 (Fig. 4a). We showed that vaccine-induced OT-II-DTR-GFP+ Treg cells could be specifically and efficiently eliminated (>95%) by treatment with a low dose (0.5 μg) of DT (Fig. 4b).
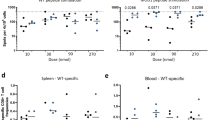
The effects of depletion of antigen-specific Treg cells on the antiviral immunity against acute influenza virus infection. a Schematic representation of the experimental protocol. CD45.1 mice with adoptive transfer of CD45.2+CD25−Foxp3-GFP− OT-II T cells received primary and secondary s.c. immunization with OVA OT-II peptide (10 μg). Mice were then treated with PBS control or with DT (0.5 μg) to deplete OVA OT-II-specific Treg cells, and subsequently infected by PR8-OVAII virus (80 PFU/mouse). b At day 7 post infection, mice were sacrificed for analysis of the antigen-specific Treg cells in the dLNs. c The proportional body weight change of the recipient CD45.1 mice with indicated treatments were recorded at the indicated days post infection. d Viral titer in lungs (n ≧ 8 mice per group compiled from three independent experiments) and e virus-specific IFN-γ-producing T cells of spleens, dLNs, and lungs in the OVA OT-II peptide-immunized mice with or without DT treatment at 7 days post infection. Data are individual percentages of virus-specific IFN-γ-producing T cells for spleens, dLNs (n ≧ 8 mice per group compiled from three independent experiments), and lung (n ≧ 3 mice per group compiled from two independent experiments) with mean ± SE. *P < 0.05; **P < 0.005; ***P < 0.001 (Student’s t test)
In mice receiving OVA OT-II peptide vaccination and subsequent PR8-NA-OVAII infection, those with DT treatment exhibited significantly higher body weight and lower viral titer in lungs than PBS-treated control ones (no depletion of antigen-specific Treg cells) (Fig. 4c, d). We also found that depletion of OT-II-DTR Treg cells by DT treatment only slightly, although significantly, increased virus-specific IFN-γ-producing CD8 T cells in spleens and CD4 T cells in dLNs (Fig. 4e). Of note, the body weight and lung viral load of mice receiving DT treatment without prior OVA OT-II peptide vaccination did not differ significantly from those of PBS control mice, excluding the possibility that non-specific inflammation caused by DT treatment might have contributed to viral clearance. Taken together, specific depletion of the vaccine-induced antigen-specific Treg cells promotes viral clearance during acute influenza virus infection, suggesting their role in suppressing the antiviral immunity.
Vaccination with the CpG adjuvant suppresses recruitment of Treg cells to the lung and provides protective antiviral T cell immunity against acute influenza virus infection
To establish T cell memory in the lung, we utilized a peripheral prime–local-boost strategy in which mice were s.c. primed and intranasally (i.n.) boosted.23 We first evaluated the effect of the CpG adjuvant with this strategy on the local recruitment and accumulation of vaccine-induced antigen-specific Treg cells in the lung. WT B6 mice receiving adoptive transfer of Thy1.1/1.2Foxp3-GFP− OT-II T cells were primarily immunized by 10 μg OVA OT-II peptide alone or combined with CpG via the s.c. route at day 0, and then i.n. boosted at day 21 (Fig. 5a). Compared with mice primed and boosted by the OVA OT-II peptide alone, mice primed and boosted by the OVA OT-II peptide with CpG adjuvant had significantly lower percentage of OT-II Treg cells (37.4 vs. 2.3% in lung, 61.3 vs. 0.7% in dLN, and 46.5 vs. 0.8% in spleen) and higher percentage of non-Treg cells in lungs, dLNs, and spleens (Fig. 5b, c). Furthermore, we counted the absolute number of OT-II Treg and total OT-II T cells in the lung, and found that mice immunized by OVA OT-II peptide plus CpG recruited significantly more total Thy1.1+ OT-II T cells to the lung than those immunized by OVA OT-II peptide alone (Fig. 5d). In addition, the absolute number of OT-II Treg cells in the lung was also higher in mice immunized by OVA OT-II peptide plus CpG when compared to those immunized by OVA OT-II peptide alone, although this did not reach statistical significance.
The effect of CpG adjuvant on the recruitment and accumulation of vaccine-induced Treg cells in lung in mice receiving the peripheral prime–local-boost immunization. a Schematic representation of the experimental protocol. WT Thy1.2+/+ B6 mice with adoptively transfer of Thy1.1/1.2CD4+Foxp3-GFP− OT-II T cells received primary s.c. immunization by PBS or OVA OT-II peptide with/without CpG and secondary i.n. immunization by OVA OT-II peptide with/without CpG. b, c, and e Thy1.1+CD4+Foxp3-GFP+ OT-II Treg cells in the spleens, dLNs, and lungs of the immunized mice were analyzed at day 7 post secondary immunization. b Representative flow cytometric plots displaying Thy1.1+CD4+Foxp3-GFP+ OT-II antigen-specific Treg cells. c Individual percentages of Thy1.1+CD4+Foxp3-GFP+ OT-II T cells in spleens (n ≧ 6 mice per group complied from three independent experiments). For dLNs and lungs, data with mean ± SE are representative of four independent experiments, in which each sample represented a pool of cells from two to three vaccinated mice. d Individual total numbers of Thy1.1+CD4+Foxp3-GFP+ OT-II donor cells (left panel) and Thy1.1+CD4+ OT-II cells (right panel) in lung (three independent experiments) are shown with mean ± SE. *P < 0.05; **P < 0.05; ***P < 0.001 (Student’s t test)
We further examined whether the T cell immunity induced by CpG-adjuvanted vaccines with the peripheral prime–local-boost strategy could protect mice from acute influenza viral infection. To focus on the T cell immunity, we immunized mice with the peptides OVA257–264 (OVA OT-I) and OVA OT-II, and subsequently infected them with HKx31-HA-OVAI/II. We demonstrated that HKx31-HA-OVAI/II infection specifically stimulated the proliferation of OT-I and OT-II cells in mice (Supplemental Fig. 5). Mice were s.c. primed and then i.n. boosted by OVA OT-I/OT-II peptides alone or in combination with CpG at days 0 and 21 (Fig. 6a). PBS alone (unimmunized), s.c./i.n. CpG alone, and s.c./s.c. CpG-adjuvanted OT-I/OT-II peptides also served as controls (Fig. 6a). Subsequently, mice were challenged with a lethal dose of HKx31-HA-OVAI/II. The survival rate (87.5%) of mice immunized by s.c./i.n. OT-I/OT-II peptide adjuvanted with CpG was significantly higher than the mice from remaining groups, except for CpG-only group and the group of s.c./s.c. OT-I/OT-II peptides with CpG (Fig. 6b). Moreover, compared with all the controls, except for s.c./s.c. CpG-adjuvanted OT-I/OT-II peptides, s.c./i.n. CpG-adjuvanted OVA OT-I/OT-II peptides significantly reduced the lung viral load at 7 days post immunization (Fig. 6c). In addition, mice receiving s.c./i.n. CpG-adjuvanted peptide vaccines had significantly higher proportion of IFN-γ-producing OT-I CD8 T and OT-II CD4 T cells (Fig. 6d–g).
CpG-adjuvanted OVA OT-I/OT-II peptide vaccines protected mice from HKx31-HA-OVAI/II influenza virus infection. a Schematic representation of the experimental protocol. C57BL/6 mice received primary s.c. and secondary s.c. or i.n. immunization with OVA OT-I/OT-II peptides (10 μg/10 μg) alone or with CpG. Immunized mice were then infected with HKx31-HA-OVAI/II (5 × 105 PFU/mouse). b The survival rates of HKx31-HA-OVAI/II-infected mice immunized by PBS (circle), OVA OT-I/OT-II peptides alone (triangle), or OVA OT-I/OT-II peptides with CpG adjuvant (square). c Lung viral loads were analyzed at day 7 post HKx31-HA-OVAI/II infection. Data are individual viral loads with mean ± SE (n ≧ 4 mice per group compiled from three independent experiments). d–g OVA OT-I/OT-II antigen-specific CD8 and CD4 T cell immunity of spleens, dLNs, and lungs were analyzed at day 7 post HKx31-HA-OVAI/II infection. d Representative flow cytometric plots of virus-specific IFN-γ-producing T cells for spleens and dLNs. e Individual percentages of virus-specific IFN-γ-producing T cells for spleens and dLN with mean ± SE (n ≧ 7 mice per group complied from three independent experiments). f Representative flow cytometric plots of virus-specific IFN-γ-producing T cells for lungs. g Individual percentages of virus-specific IFN-γ-producing T cells for lungs with mean ± SE (n ≧ 4 mice per group). OVAI/II OVA OT-I/OT-II peptides. *P < 0.05; **P < 0.005 (Fisher’s exact test for the survival rate). NS not significant
We also examined the protective effect of the CpG-adjuvanted vaccines with this peripheral prime–local-boost strategy using more relevant viral peptides that are derived from the PR8 nucleoprotein: major histocompatibility complex (MHC) class I-restricted NP366–374 (NPI) and MHC class II-restricted NP311–325 (NPII). Compared to mice immunized with NPI and NPII (NP I/II) peptides alone, those immunized with NPI/II plus CpG had a higher survival rate following PR8 infection (Fig. 7a), although the survival rates among the three groups (PBS, NPI/II alone, and NPI/II + CpG) was not significantly different. Additionally, the body weight of mice immunized with NPI/II plus CpG was significantly higher than that of unimmunized mice (PBS control) or mice immunized by NPI/II alone only from day 10 post infection onwards (Fig. 7b). More importantly, mice immunized with NPI/II plus CpG had significantly lower lung viral load than the other two groups (Fig. 7c). We also found that mice immunized by NPI/II plus CpG had significantly more NPII-specific IFN-γ-producing CD4 T cells in the lung, although they seemed to have lower NPI-specific CD8 T cells than unimmunized mice (PBS/PBS controls) (Fig. 7d–g). Finally, we demonstrated that WT B6 Mice immunized by CpG-adjuvanted whole-inactivated virus (WIV) derived from HKx31 (H3N2) through s.c. priming and i.n. boosting were significantly more resistant to PR8 challenge than those receiving unadjuvanted WIV (Supplemental Fig. 6). It is known that neutralizing antibodies against HKx31 and PR8 only provide negligible cross-protection, so this system can be utilized to examine the protective effect of antiviral T cell immunity.28,29 We also found that HKx31 WIV did not induce detectable levels of hemagglutination-inhibiting titer against PR8 (data not shown), although it remains possible that there may be some non-neutralizing cross-reactive antibodies contributing to cross-protection against heterosubtypic influenza virus infection. Collectively, our data show that through the peripheral (s.c.) priming and local (i.n.) boosting strategy, vaccination with the CpG adjuvant not only reduces the accumulation of vaccine-induced Treg cells in the lung, but also enhances the antiviral T cell immunity, conferring protective immunity against heterosubtypic influenza viral infections.
CpG-adjuvanted NPI/NPII peptide vaccines protected mice from PR8 influenza virus infection. C57BL/6 mice received primary s.c. and secondary i.n. immunization with NPI/NPII peptides (10 μg/10 μg) alone or with CpG. Immunized mice were then infected with PR8 (110 PFU/mouse). a The survival rates and b body weight of PR8-infected mice immunized by PBS (circle), NPI/NPII peptides alone (triangle), or NPI/NPII peptides with CpG adjuvant (square). c Lung viral load was analyzed at day 7 post PR8 infection. Data are individual viral load with mean ± SE (n ≧ 7 mice per group compiled from two independent experiments). d–g NPI -specific CD8 and NPII-specific CD4 T cell immunity of spleens, dLNs, and lungs were analyzed at day 7 post PR8 infection. d, e Representative flow cytometric plots of NPI-specific IFN-γ-producing CD8 T cells (d) and NPII-specific IFN-γ-producing CD4 T cells (e) for spleens, dLNs, and lungs. Individual cell numbers (f) and percentages (g) of NPI-specific IFN-γ-producing CD8 T cells and NPII-specific IFN-γ-producing CD4 T cells for spleens (n ≧ 7 mice per group complied from three independent experiments), dLNs (n ≧ 7 mice per group complied from three independent experiments), and lungs with mean ± SE (n ≧ 7 mice per group complied from two independent experiments). *P < 0.05; **P < 0.005; ***P < 0.001 (Fisher’s exact test for survival rate). *P < 0.05; ***P < 0.001
Discussion
It has been difficult to track and study antigen-specific Treg cells in vivo because they are extremely rare under physiological conditions. Our TCR-transgenic OT-II T cell adoptive transfer model and genetic modified influenza virus incorporating the OT-II peptide provide a convenient and robust system to investigate the role of vaccine-induced antigen-specific Treg cells during acute influenza viral infection. Using this model, we demonstrated that unadjuvanted peptide vaccines induce a significant portion of antigen-specific Treg cells in a dose-dependent manner. These vaccine-induced Treg cells are functionally suppressive in vitro and in vivo and attenuate the antiviral immunity against influenza virus infection. Consistently, previous studies reported that subimmunogenic immunization promotes the development of antigen-specific Treg cells.30 In addition, the high ratio of Foxp3+ Treg cells among T cells possessing the same antigen specificity has been shown to attenuate anti-tumor T cell immunity.31 Actually, we found that the ratios of vaccine-induced antigen-specific Treg cells in mice receiving unadjuvanted OVA OT-II peptides are quite similar between 2 and 4 weeks following primary immunization. This indicates that the ratio of vaccine-induced antigen-specific Treg cells remains stable from 2 weeks after primary immunization.
Our results further showed that several adjuvants, including TLR agonists and CFA, when coadministered with peptide vaccines, dramatically reduced the ratio of antigen-specific Treg cells, whereas the clinically licensed alum adjuvant failed to suppress the induction of Treg cells. In addition, the CpG adjuvant prevented the increase in the ratio of antigen-specific Treg cells upon secondary immunization in mice primed by peptide alone, but did not suppress antigen-specific Treg cells to a level as low as that induced by CpG priming. Consistent with our observation, Timothy et al. 32 also found that prior vaccination in lung mucosa with unadjuvanted influenza antigen alone induces Treg cells that significantly reduce the immune response to subsequent pulmonary-delivered influenza ISCOMATRIXTM-adjuvanted vaccine. Taken together, our data suggest that antigen-specific Tregs induced by an initial suboptimal vaccination strategy have detrimental effect on the immune response induced by effective adjuvanted vaccines. Although our results reveal the Treg-suppression function of adjuvants, several adjuvants are also found to induce antigen-specific Treg cells, which can be utilized for treatment of chronic inflammatory disease, like autoimmune disease.33 However, the antigen dose, formulation, and vaccination route may also affect the immunomodulatory effect of adjuvants and need to be further studied.
A previous study has reported that peripheral Treg conversion is established by inhibition of dendritic cell activation, which reduces T cell proliferation and enhances the conversion rate.30 It is likely that TLR agonists suppress the induction of antigen-specific Treg cells by activation of dendritic cells, although the detailed molecular mechanisms remain to be explored. Interestingly, we found that the alum adjuvant failed to reduce the frequency of antigen-specific Treg cells in primary immunization, but was able to restrict the expansion of Tregs in spleens upon secondary immunization. Alum has been demonstrated to activate the inflammasome NLRP3 pathway, although the underlying pathways involved in the alum-mediated adjuvant activity remains unclear.34 Whether the TLR and NLRP3 pathways differentially affect the development of antigen-specific Treg cells in vivo requires further investigation.
Previous studies have shown that acute influenza virus infection induces antigen-specific Foxp3+ Treg cells, and promotes expansion of memory Treg cells upon secondary influenza infection.13,14,15 By adoptive transfer of HA-specific Treg and non-Treg cells into Balb/c mice, Sanchez et al. 13 demonstrated that the expansion of Treg is less robust than non-Treg cells (50-fold vs. 290-fold expansion) at 7 days post influenza virus infection. However, we found that acute influenza virus infection significantly increased the percentage of preexisting vaccine-induced antigen-specific Treg cells at 7 days post infection. The study of Sanchez et al. 13 is different from ours in that they adoptively transferred pure antigen-specific Treg or non-Treg cells to recipient mice separately and infected them by virus. However, in our system, Treg and non-Treg cells bearing the same antigen specificity co-existed in vivo, and might compete with each other for antigen stimulation and proliferation. Our results suggest the increased ratio of antigen-specific Treg cells is likely to be caused by faster proliferation of Treg than non-Treg cells during acute influenza virus infection. Alternatively, antigen-specific Treg cells might be further converted from non-Treg cells. However, primary acute influenza infection barely induced antigen-specific Treg cells. Therefore, it seems unlikely that conversion of non-Treg cells to Treg cells played a major role during secondary influenza virus challenge. Rather, it is more likely that faster proliferation of antigen-specific Treg cells than non-Treg cells resulted in the increase of the Treg ratio. In support of this view, using peptide-MHC class II tetramers, Brincks et al. 15 showed that viral antigen-specific Treg cells reach an earlier peak than non-Treg cells upon the secondary influenza infection, indicating that Treg cells undergo faster expansion than non-Treg cells by the stimulation of the same antigen.15 The expansion of antigen-specific Treg cells is also consistent with the previous report that antigen-specific Treg cells induced in subimmunogenic conditions can be further expanded by immunogenic stimulation.30 Intriguingly, our results showed that primary immunization with CpG-adjuvanted peptides significantly reduced the magnitude of subsequent expansion of antigen-specific Treg cells driven by the secondary influenza virus infection. This suggests that an initial optimal vaccination strategy is critical for preventing the development of vaccine-induced viral antigen-specific Treg cells during acute influenza viral infection. This finding has important implication for future vaccination strategy.
The role of vaccine-induced pathogen-specific Treg cells in antiviral immunity has not been convincingly addressed in vivo. Previous studies usually used the strategy of non-specific depletion of all polyclonal Foxp3+ Treg cells. For example, depletion of polyclonal Treg cells by anti-CD25 antibody in WT mice or by DT in DEREG mice was shown to enhance antiviral T cell immunity.15,16 However, this approach failed to determine the effect of antigen-specific Treg cells in vivo during acute viral infection. Using OT-II × DEREG mice, we clearly demonstrated that depletion of vaccine-induced pathogen-specific Treg cells enhanced viral control, strongly supporting their role in suppression of antiviral immunity in vivo. However, we did not observe significantly enhanced IFN-γ-producing T cells after depletion of pathogen-specific Treg cells. Although the underlying mechanisms remain unknown, one plausible explanation is that pathogen-specific Treg cells might affect the other functions of antiviral T cell immune responses besides IFN-γ production in our infection condition. Alternatively, pathogen-specific Treg cells may inhibit antiviral immunity through T cell-independent mechanisms.
T cell immunity in the local infection site, termed resident T cell memory, has been shown to be of critical importance for the control of infections by providing the first-line defense against invading pathogens, including heterosubtypic influenza viral infection.24,26,35 Therefore, to establish protective resident T cell immunity, we utilized the peripheral priming/local boosting strategy, which has been shown to promote greater accumulation and recruitment of antigen-specific CD4+ T cells in the lung.23 Using this strategy, we showed that the CpG adjuvant could promote the immunogenicity of peptide vaccines and conferred the protective immunity against heterosubtypic influenza virus infections by reducing the ratio of antigen-specific Treg cells and increasing effector T cells that accumulated in the lung. Interestingly, we found that the total number of pathogen-specific Treg cells in the lung of the mice immunized by CpG-adjuvanted peptides were not fewer than those of mice immunized by unadjuvanted peptides. This suggests that the ratio of antigen-specific Treg to non-Treg cells is more important than the absolute number of Treg cells in modulating antiviral T cell immunity. This is in agreement with a previous study, which also reported that CpG adjuvant can improve the ratio of antigen-specific effector to Treg cells, and enhance the anti-tumor T cell immunity.31
Our system certainly bears some intrinsic limitations. The major drawback is the use of non-physiologically high frequency of adoptively transferred clonal TCR-transgenic T cells.36 In this situation, the balance between antigen dose and the availability of TCR-transgenic T cells may be disturbed. In addition, model antigen may not be representative of natural antigens of influenza virus. To overcome this issue, we also adoptively transferred fewer OT-II T cells, and observed similar results regarding the induction of antigen-specific Treg cells. Future studies using a more physiological system are required to validate our findings.
In summary, we clearly demonstrated the suppressive effect of vaccine-induced antigen-specific Treg cells on the antiviral immunity against influenza virus infection. The CpG-adjuvanted peptide vaccines exhibit enhanced antiviral immunity probably by both antagonizing vaccine-induced antigen-specific Treg cells and promoting antiviral T cell immunity. Because the ratio of vaccine-induced antigen-specific Treg cells can be further expanded by acute influenza viral infection and repeated vaccination, our data suggest that the initial priming strategy is critical to prevent the future development of viral antigen-specific Treg cells and establishment of long-term effective antiviral immunity. Given the frequent occurrence of influenza viral infections and vaccinations in the entire lifespan of an individual, design of optimal vaccination strategies, particularly in the early years of life, should be important for the success of influenza T cell vaccines.
Methods
Mice
All mouse experiment protocols were approved by the Laboratory Animal Committee of National Taiwan University College of Medicine (NTUCOM). C57BL/6 (B6) WT mice (CD45.2 and Thy1.2) came from the National Laboratory Animal Center in Taiwan. All the following special mouse strains are on the B6 background. The breeder pairs of DEREG were a gift from Dr. Tim Sparwasser (Munich, Germany).27 The breeder pairs of Foxp3gfp, which encodes a chimeric GFP-Foxp3 fusion protein by insertion of eGFP in the N terminal of Foxp3 (GFP-knock-in), was a gift from Dr. Alexander Rudensky (New York, USA). B6 mice with specific T cell lineage markers (Thy1.1 and CD45.1), TCR-transgenic OT-II mice, and DEREG mice were maintained in the Laboratory Animal Center of National Taiwan University College of Medicine. CD45.1 × OT-II, Thy1.1/Thy1.2 × Foxp3gfp× × OT-II, and OT-II × DEREG mice were generated by cross-breeding the indicated mouse lines on a B6 background by ourselves, and were maintained in the Animal Center of National Taiwan University College of Medicine.
Viruses, infection, and virus quantification
The plasmids hemagglutinin (HA) and neuraminidase (NA) of HKx31 cloned in pHW2000 were a gift from Dr. Paul Thomas (Memphis, USA). PR8-NA-OVAII were generated by replacing NA43–58 with OVA323–339 (ISQAVHAAHAEINEAGR) as previously described.37 The HKx31-HA-OVAI/II was generated using a strategy described previously.38 The OVA OT-I/OT-II peptide (OVA257–264/OVA323–339) was modified by adding SR (XbaI site), GT (KpnI site), and GGGGS linker to generate SR-SIINFEKL/ISQAVHAAHAEINEAGR-GT-GGGS, which was then inserted into HKx31-HA after the glycine at residue 17. All viruses, including PR8, HKx31, PR8-NA-OVAII, and HKx31-HA-OVAI/II, were produced by the 8-plasmid reverse genetics system and propagated in Madin–Darby Canine Kidney (MDCK) cell monolayers, and were titrated by the plaque assay. Six-week to eight-week-old mice were fully anesthetized by intraperitoneal injection of Rompun (xylazine) and Zoletil (tiletamine hypochloride and zolazepam hypochloride) and then infected with 20 µl of viral suspension with indicated doses of viruses via the i.n. route. To determine the lung viral titer of infected mice, lungs were isolated and homogenized in 1 ml infection medium consisting of Dulbecco's modified Eagle's medium with non-essential amino acid, sodium pyruvate, and bovine serum albumin. Lung viral loads were determined by inoculation of MDCK cells in six-well plates with serial tenfold dilutions of the lung suspension using the plaque assay.
Adoptive transfer of naïve CD4+ T cells
Splenocytes from indicated donor mice were prepared as a single-cell suspension and FACS (fluorescence-activated cell sorting) sorted for CD4+OT-II+CD25−GFP− cells, which were adjusted to an appropriate final volume with sterile serum-free RPMI-1640 (Gibco). Each mouse received 0.3 ml of cell suspension with the cell number of 3 × 106 to 4 × 106 cells. Donor cells were transferred into recipient mice by intravenous (i.v.) injection through the tail veins.
WIV preparation
HKx31 viruses were amplified in MDCK cells. Sucrose (Sigma) was dissolved in PBS, and prepared as 60%, 30%, and 20% (w/v) sucrose solution. The viral culture supernatant was layered on top of 20% sucrose solution in a centrifuge tube, which was then ultracentrifuged at 100,000 x g overnight at 4 °C. The next day, the virus pellet in the bottom of tubes was resuspended in 5 ml of PBS. The sucrose gradient tubes were made by layering successively from pipetting 5 ml each of 60, 30, and 20% (w/v) sucrose, and followed by the virus soup. The tube was then ultracentrifuged at 100,000 x g at 4°C for 1.5 h. Purified virus stayed between 30 and 60% sucrose gradients. Viruses were inactivated in the formaldehyde solution, which was adjusted to the final concentration of 0.01% and was incubated at 37 °C for overnight. The next day, inactivated virus was dialyzed with PBS through Dialysis cassette G2 (Thermo Scientific) and stored at −80 °C.
Immunization of mice
Mice were immunized through either s.c. injection with 100 μl of vaccines or the intranasal route with 20 μl of vaccines. All vaccine liquids were freshly prepared and diluted with PBS. Vaccines used for the subcutaneous injection contained immunogens, OVA257–264 (OT-I)/OVA323–339 (OT-II) peptides, NP366–374/NP311–325 peptides or WIV, alone or combined with different adjuvants, including CpG ODN 1,826 (CpG) (TLR-9 agonist) (50 μg) (InvivoGen), Alum (2 mg) (Thermo), R848 (TLR-7/8 agonist) (50 μg) (InvivoGen), or CFA (50 μg) (Sigma). Vaccines used for the i.n. route contained immunogens alone or with CpG (20 μg). The peptide sequences are listed below: OVA257–264 (OT-I peptide) (SIINFEKL), OVA323–339 (OT-II peptide)(ISQAVHAAHAEINEAGR), NP366–374 (ASNENMETM), and NP311–325 (QVYSLIRPNENPAHK).
The in vitro suppression assay for vaccine-induced Treg cells
WT B6 mice received FACS-sorted CD4+OT-II+CD25−GFP− cells with the cell number of 3 × 106 to 4 × 106 by i.v. injection, and immunized with 10 μg of OVA OT-II peptide at day 0, 21, and 35 post immunization. At day 42 post immunization, 5 or 6 OVA OT-II peptide-immunized WT mice were sacrificed, and cells pooled from all the spleens and inguinal LNs were sorted for CD4+OT-II+CD25+GFP+ Treg cells. For the suppression assay, 2.5 × 104 naïve CD4+CD25−GFP− conventional T cells sorted from the splenocytes of Thy1.1 × Foxp3gfp OT-II mice were stained with violet proliferation dye 450 (BD Biosciences), and co-cultured with different ratios of vaccine-induced Treg cells and 1.5 × 103 bone marrow-derived dendritic cells (BMDCs) per well in a 96-well V-bottom plate. CD4+CD25+GFP+ naïve Treg cells sorted from the splenocytes of Thy1.1 × Foxp3gfp OT-II mice were used as a control. Further, anti-CD3 antibody (BD Biosciences) was added to the culture medium in a final concentration of 1 μg/ml. After 3 days, cells were collected and subjected to the flow cytometry analysis for cell proliferation. Proliferating cells were measured based on the dilution of violet proliferation dye 450. Percent suppression = 100 – (percentage of proliferating cells with Treg present/percentage of proliferating cells without Treg present) × 100.39
Reagents, cell staining, and flow cytometry analysis
Cells were washed twice with staining buffer (PBS containing 2% fetal bovine serum (FBS)), and stained with fluorescence-conjugated antibodies against surface markers wherever appropriate, including anti-CD45.1 PE (eBioscience), anti-Thy1.1 APC (eBioscience), anti-CD3 FITC (eBioscience), anti-CD4 PerCP-Cy5.5 (eBioscience), and anti-CD8 PE (eBioscience) for 30 min. For intracellular IFN-γ staining, cells were fixed and permeabilized (Cytofix/Cytoperm, BD Biosciences) after surface staining, and then stained intracellularly with anti-IFN-γ-APC (BD Biosciences). For intracellular Foxp3 staining, cells were fixed and permeabilized (Foxp3/Transcription Factor Fixation/Permeabilization Concentrate and Diluent, eBioscience) after surface staining, and then stained intracellularly with anti-Foxp3-PE-Cy7 (eBioscience). Samples were measured by FACS Verse and the flow cytometry analysis was done by FlowJo®.
Measurement of virus-specific T cells
A total of 2 × 105 BMDCs were infected with PR8-NA-OVAII at a multiplicity of infection of 2 for 5 h in the 50 μl infection medium in a 96-V-bottom plate. After 5 h post infection, the BMDCs were washed with T cell culture medium (RPMI-1640 containing 10% low endotoxin FBS, 1% glutamine, penicillin, streptomycin, and 2-mercaptoethanol). At the same time, primary cells from the spleens, LNs, and lungs were resuspended in the T cell culture medium. A total of 6 × 105 primary cells/100 μl were co-cultured with influenza vrius-infected BMDCs in 100 μl of T cell culture medium containing mouse recombinant interleukin-2 (2 ng/ml). After 4 h post co-culture, cells were treated with Golgi Plug (BD Biosciences) for 11 h, and analyzed by intracellular IFN-γ staining. To measure the OVA257–264-specific and OVA323–339-specific T cells, 1 × 106 of primary cells from the spleens and LNs were stimulated with OVA OT-I peptide (10 μg/ml) and OVA OT-II peptide (40 μg/ml) for 6 h in the 200 μl of T cell culture medium plus Golgi Plug (BD Biosciences) in 96-U-bottom plate, and analyzed by intracellular IFN-γ staining.
Statistical analyses
Data are expressed as mean ± standard error (SE) values. The 14-day survival rates were analyzed by the Fisher’s exact test. Continuous variables, including lung viral titers and percentage of antigen-specific Treg and effector T cells were analyzed by the Student’s t test. A P value of <0.05 was considered statistically significant.
References
Houser, K. & Subbarao, K. Influenza vaccines: challenges and solutions. Cell Host Microbe 17, 295–300, (2015).
Thomas, P. G., Keating, R., Hulse-Post, D. J. & Doherty, P. C. Cell-mediated protection in influenza infection. Emerg. Infect. Dis. 12, 48–54 (2006).
Sridhar, S. Heterosubtypic T-cell immunity to influenza in humans: challenges for universal T-cell influenza vaccines. Front. Immunol. 7, 195, (2016).
Sridhar, S. et al. Cellular immune correlates of protection against symptomatic pandemic influenza. Nat. Med. 19, 1305–1312, (2013).
Wilkinson, T. M. et al. Preexisting influenza-specific CD4+ T cells correlate with disease protection against influenza challenge in humans. Nat. Med. 18, 274–280, (2012).
McMichael, A. J., Gotch, F. M., Dongworth, D. W., Clark, A. & Potter, C. W. Declining T-cell immunity to influenza, 1977–82. Lancet 2, 762–764 (1983).
Pleguezuelos, O. et al. A synthetic influenza virus vaccine induces a cellular immune response that correlates with reduction in symptomatology and virus shedding in a randomized phase Ib live-virus challenge in humans. Clin. Vaccin. Immunol. 22, 828–835, (2015).
Atsmon, J. et al. Safety and immunogenicity of multimeric-001—a novel universal influenza vaccine. J. Clin. Immunol. 32, 595–603, (2012).
Rosendahl Huber, S., van Beek, J., de Jonge, J., Luytjes, W. & van Baarle, D. T cell responses to viral infection—opportunities for Peptide vaccination. Front. Immunol. 5, 171, (2014).
Sakaguchi, S., Yamaguchi, T., Nomura, T. & Ono, M. Regulatory T cells and immune tolerance. Cell 133, 775–787, (2008).
Josefowicz, S. Z., Lu, L. F. & Rudensky, A. Y. Regulatory T cells: mechanisms of differentiation and function. Annu. Rev. Immunol. 30, 531–564, (2012).
Abbas, A. K. et al. Regulatory T cells: recommendations to simplify the nomenclature. Nat. Immunol. 14, 307–308, (2013).
Sanchez, A. M., Zhu, J., Huang, X. & Yang, Y. The development and function of memory regulatory T cells after acute viral infections. J. Immunol. 189, 2805–2814, (2012).
Betts, R. J. et al. Influenza A virus infection results in a robust, antigen-responsive, and widely disseminated Foxp3+ regulatory T cell response. J. Virol. 86, 2817–2825, (2012).
Brincks, E. L. et al. Antigen-specific memory regulatory CD4+Foxp3+ T cells control memory responses to influenza virus infection. J. Immunol. 190, 3438–3446, (2013).
Suvas, S., Kumaraguru, U., Pack, C. D., Lee, S. & Rouse, B. T. CD4+CD25+ T cells regulate virus-specific primary and memory CD8+ T cell responses. J. Exp. Med. 198, 889–901, (2003).
Bayry, J. Regulatory T cells as adjuvant target for enhancing the viral disease vaccine efficacy. Virus Dis. 25, 18–25, (2014).
Coffman, R. L., Sher, A. & Seder, R. A. Vaccine adjuvants: putting innate immunity to work. Immunity 33, 492–503, (2010).
Marrack, P., M., A. & Munks, M. W. Towards an understanding of the adjuvant action of aluminium. Nat. Rev. Immunol. 9, 287–293 (2009).
Peng, G. et al. Toll-like receptor 8-mediated reversal of CD4+ regulatory T cell function. Science 309, 1380–1384 (2005).
Fiorino, F., Pettini, E., Pozzi, G., Medaglini, D. & Ciabattini, A. Prime-boost strategies in mucosal immunization affect local IgA production and the type of th response. Front. Immunol. 4, 128, (2013).
Uddback, I. E. et al. Combined local and systemic immunization is essential for durable T-cell mediated heterosubtypic immunity against influenza A virus. Sci. Rep. 6, 20137, (2016).
Ciabattini, A. et al. Characterization of the antigen-specific CD4(+) T cell response induced by prime-boost strategies with CAF01 and CpG adjuvants administered by the intranasal and subcutaneous routes. Front. Immunol. 6, 430, (2015).
Teijaro, J. R. et al. Cutting edge: tissue-retentive lung memory CD4 T cells mediate optimal protection to respiratory virus infection. J. Immunol. 187, 5510–5514, (2011).
Laidlaw, B. J. et al. CD4+ T cell help guides formation of CD103+ lung-resident memory CD8+ T cells during influenza viral infection. Immunity 41, 633–645, (2014).
Wu, T. et al. Lung-resident memory CD8 T cells (TRM) are indispensable for optimal cross-protection against pulmonary virus infection. J. Leukoc. Biol. 95, 215–224, (2014).
Lahl, K. et al. Selective depletion of Foxp3+ regulatory T cells induces a scurfy-like disease. J. Exp. Med. 204, 57–63, (2007).
Flynn, K. J. et al. Virus-specific CD8 1 T cells in primary and secondary influenza pneumonia. Immunity 8, 683–691 (1998).
Topham D. J. & Doherty P. C. Clearance of an influenza A virus by CD4 7T cells is inefficient in the absence of B cells. J. Virol. 72, 882–885, (1998).
Kretschmer, K. et al. Inducing and expanding regulatory T cell populations by foreign antigen. Nat. Immunol. 6, 1219–1227, (2005).
Perret, R. et al. Adjuvants that improve the ratio of antigen-specific effector to regulatory T cells enhance tumor immunity. Cancer Res. 73, 6597–6608, (2013).
Timothy, A. A. et al. ISCOMATRIX adjuvant reduces mucosal tolerance for effective pulmonary vaccination against influenza. Hum. Vaccin Immunother. 11, 377–385, (2015).
Keijzer, C., van der Zee, R., van Eden, W. & Broere, F. Treg inducing adjuvants for therapeutic vaccination against chronic inflammatory diseases. Front. Immunol. 4, 245, (2013).
Franchi, L. & Nunez, G. The Nlrp3 inflammasome is critical for aluminium hydroxide-mediated IL-1beta secretion but dispensable for adjuvant activity. Eur. J. Immunol. 38, 2085–2089, (2008).
Schenkel, J. M. et al. T cell memory. Resident memory CD8 T cells trigger protective innate and adaptive immune responses. Science 346, 98–101, (2014).
Zinkernagel, R. M. & Hengartner, H. Regulation of the immune response by antigen. Science 293, 251–253, (2001).
Chapman, T. J., Castrucci, M. R., Padrick, R. C., Bradley, L. M. & Topham, D. J. Antigen-specific and non-specific CD4+ T cell recruitment and proliferation during influenza infection. Virology 340, 296–306, (2005).
Garulli, B., Di Mario, G., Sciaraffia, E., Kawaoka, Y. & Castrucci, M. R. Immunogenicity of a recombinant influenza virus bearing both the CD4+ and CD8+ T cell epitopes of ovalbumin. J. Biomed. Biotechnol. 2011, 497364, (2011).
Fazekas de St Groth, B., Zhu, E., Asad, S. & Lee, L. Flow cytometric detection of human regulatory T cells. Methods Mol. Biol. 707, 263–279, (2011).
Acknowledgements
We thank Dr. Mi-Hua Tao and Dr. Ching-Hwa Tsai for their critical review and constructive comments on this manuscript. We also would like to acknowledge the service provided by the Flow Cytometric Analyzing and Sorting Core of the First Core Laboratory and the Third Core Laboratory, National Taiwan University College of Medicine. This work was supported by grants from the National Taiwan University Hospital (grant number UN106-057), and the Ministry of Science and Technology (grant number MOST105-2628-B-002-027-MY3), Executive Yuan, Taiwan.
Author information
Authors and Affiliations
Contributions
P.-H.L. P.-J.C., and H.-C.Y. formed the original concepts and designs of the experiments. P.-H.L., W.-I.W., Y.-L.W., M.-P.H., C.-W.L., C.-Y.L., and S.-H.J. performed the experiments; P.-H.L. acquired and interpreted data; P.-J.C and H.-C.Y. reviewed and helped interpret the data; P.-H.L. and H.-C.Y. drafted and finalized the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Lin, PH., Wong, WI., Wang, YL. et al. Vaccine-induced antigen-specific regulatory T cells attenuate the antiviral immunity against acute influenza virus infection. Mucosal Immunol 11, 1239–1253 (2018). https://doi.org/10.1038/s41385-018-0004-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41385-018-0004-9
This article is cited by
-
Immunomodulatory drugs have divergent effects on humoral and cellular immune responses to SARS-CoV-2 vaccination in people living with rheumatoid arthritis
Scientific Reports (2023)
-
Mucosal immunity to poliovirus
Mucosal Immunology (2022)
-
Seasonal and pandemic influenza: 100 years of progress, still much to learn
Mucosal Immunology (2020)
-
Effect of regulatory T cells on the efficacy of the fatty acid-binding protein vaccine against Schistosoma japonicum
Parasitology Research (2019)
-
Effect of homeostatic T-cell proliferation in the vaccine responsiveness against influenza in elderly people
Immunity & Ageing (2019)