Abstract
Background
Painful physical symptoms (PPS) are highly prevalent in patients with major depressive disorder (MDD). Presence of PPS in depressed patients are potentially associated with poorer antidepressant treatment outcome. We aimed to evaluate the association of baseline pain levels and antidepressant treatment outcomes.
Methods
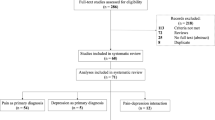
We searched PubMed, Embase and Cochrane Library databases from inception through February 2023 based on a pre-registered protocol (PROSPERO: CRD42022381349). We included original studies that reported pretreatment pain measures in antidepressant treatment responder/remitter and non-responder/non-remitter among patients with MDD. Data extraction and quality assessment were performed following the Preferred Reporting Items for Systematic Reviews and Meta-analyses by two reviewers independently. The primary outcome was the difference of the pretreatment pain levels between antidepressant treatment responder/remitter and non-responder/non-remitter. Random-effects meta-analysis was used to calculate effect sizes (Hedge’s g) and subgroup and meta-regression analyses were used to explore sources of heterogeneity.
Results
A total of 20 studies were included. Six studies reported significantly higher baseline pain severity levels in MDD treatment non-responders (Hedge’s g = 0.32; 95% CI, 0.13–0.51; P = 0.0008). Six studies reported the presence of PPS (measured using a pain severity scale) was significantly associated with poor treatment response (OR = 1.46; 95% CI, 1.04-2.04; P = 0.028). Five studies reported significant higher baseline pain interference levels in non-responders (Hedge’s g = 0.46; 95% CI, 0.32–0.61; P < 0.0001). Four studies found significantly higher baseline pain severity levels in non-remitters (Hedge’s g = 0.27; 95% CI, 0.14–0.40; P < 0.0001). Eight studies reported the presence of PPS significantly associated with treatment non-remission (OR = 1.70; 95% CI, 1.24–2.32; P = 0.0009).
Conclusions
This study suggests that PPS are negatively associated with the antidepressant treatment outcome in patients with MDD. It is possible that better management in pain conditions when treating depression can benefit the therapeutic effects of antidepressant medication in depressed patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Study data are available on request to the corresponding author at yabin.wei@bjmu.edu.cn.
References
Depression and Other Common Mental Disorders: Global Health Estimates. https://apps.who.int/iris/handle/10665/254610 (2017). Accessed 2017.
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association Publishing: Washington, 2013.
Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N. Engl J Med. 1999;341:1329–35.
Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry. 2003;60:39–47.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–45.
Munoz RA, McBride ME, Brnabic AJ, Lopez CJ, Hetem LA, Secin R, et al. Major depressive disorder in Latin America: the relationship between depression severity, painful somatic symptoms, and quality of life. J Affect Disord. 2005;86:93–8.
Lee P, Zhang M, Hong JP, Chua HC, Chen KP, Tang SW, et al. Frequency of painful physical symptoms with major depressive disorder in asia: relationship with disease severity and quality of life. J Clin Psychiatry. 2009;70:83–91.
Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66:17–22.
Wise TN, Meyers AL, Desaiah D, Mallinckrodt CH, Robinson MJ, Kajdasz DK. The significance of treating somatic symptoms on functional outcome improvement in patients with major depressive disorder: a post hoc analysis of 2 trials. Prim Care Companion J Clin Psychiatry. 2008;10:270–5.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40.
Fava M, Mallinckrodt CH, Detke MJ, Watkin JG, Wohlreich MM. The effect of duloxetine on painful physical symptoms in depressed patients: do improvements in these symptoms result in higher remission rates? J Clin Psychiatry. 2004;65:521–30.
Karp JF, Scott J, Houck P, Reynolds CF 3rd, Kupfer DJ, Frank E. Pain predicts longer time to remission during treatment of recurrent depression. J Clin Psychiatry. 2005;66:591–7.
Harada E, Satoi Y, Kikuchi T, Watanabe K, Alev L, Mimura M. Residual symptoms in patients with partial versus complete remission of a major depressive disorder episode: patterns of painful physical symptoms in depression. Neuropsychiatr Dis Treat. 2016;12:1599–607.
Stahl SM. The psychopharmacology of painful physical symptoms in depression. J Clin Psychiatry. 2002;63:382–3.
Meerwijk EL, Ford JM, Weiss SJ. Brain regions associated with psychological pain: implications for a neural network and its relationship to physical pain. Brain Imaging Behav. 2013;7:1–14.
Stubbs B, Vancampfort D, Veronese N, Thompson T, Fornaro M, Schofield P, et al. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychol Med. 2017;47:2906–17.
IsHak WW, Wen RY, Naghdechi L, Vanle B, Dang J, Knosp M, et al. Pain and depression: a systematic review. Harv Rev Psychiatry. 2018;26:352–63.
Gureje O, Von Korff M, Kola L, Demyttenaere K, He Y, Posada-Villa J, et al. The relation between multiple pains and mental disorders: results from the World Mental Health Surveys. Pain. 2008;135:82–91.
Zheng CJ, Van Drunen S, Egorova-Brumley N. Neural correlates of co-occurring pain and depression: an activation-likelihood estimation (ALE) meta-analysis and systematic review. Transl Psychiatry. 2022;12:196.
Engauge Digitizer Software. https://markummitchell.github.io/engauge-digitizer/ (2018). Accessed 2018.
Hasselblad V, Hedges LV. Meta-analysis of screening and diagnostic tests. Psychol Bull. 1995;117:167–78.
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139–45.
Brannick MT, Potter SM, Benitez B, Morris SB. Bias and precision of alternate estimators in meta-analysis: Benefits of blending Schmidt–Hunter and Hedges approaches. Organ Res Methods. 2019;22:490–514.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
Karp JF, Weiner D, Seligman K, Butters M, Miller M, Frank E, et al. Body pain and treatment response in late-life depression. Am J Geriatr Psychiatry. 2005;13:188–94.
Lin CH, Lane HY, Chen CC, Juo SH, Yen CF. Pain has a strong negative impact on the fluoxetine response in hospitalized patients with major depressive disorder. Clin J Pain. 2011;27:805–10.
Sagman D, McIntosh D, Lee MS, Li H, Ruschel S, Hussain N, et al. Attributes of response in depressed patients switched to treatment with duloxetine. Int J Clin Pract. 2011;65:73–81.
Huang X, Li C, Luo YL, Wang B, Ji JL. Efficacy of venlafaxine extended-release monotherapy for first-episode depression with painful physical symptoms. Neuroreport. 2013;24:364–9.
Stahl ST, Jung C, Weiner DK, Pecina M, Karp JF. Opioid exposure negatively affects antidepressant response to venlafaxine in older adults with chronic low back pain and depression. Pain Med. 2020;21:1538–45.
Diep C, Rosenek N, Khoo Y, Gandhi W, van Reekum CM, Ravindran AV, et al. Pain severity and pain interference during major depressive episodes treated with escitalopram and aripiprazole adjunctive therapy: a CAN-BIND-1 report. Psychiatry Res. 2022;312:114557.
Duenas HJ, Dwight T, McBride ME, Brnabic AJ, Semper LA, Holmgren D, et al. Effectiveness of antidepressants in the treatment of major depressive disorder in Latin America. Int J Psychiatry Clin Pract. 2007;11:129–39.
Leuchter AF, Husain MM, Cook IA, Trivedi MH, Wisniewski SR, Gilmer WS, et al. Painful physical symptoms and treatment outcome in major depressive disorder: a STAR*D (Sequenced Treatment Alternatives to Relieve Depression) report. Psychol Med. 2010;40:239–51.
DeVeaugh-Geiss AM, West SL, Miller WC, Sleath B, Gaynes BN, Kroenke K. The adverse effects of comorbid pain on depression outcomes in primary care patients: results from the ARTIST trial. Pain Med. 2010;11:732–41.
Chen KP, Chiu NY, Shen YC, Hou YM, Yeh CB, Ouyang WC, et al. Association between painful physical symptoms and clinical outcomes in Taiwanese patients with major depressive disorder: a three-month observational study. Asia-Pac Psychiatry. 2010;2:136–45.
Novick D, Montgomery W, Bertsch J, Peng X, Brugnoli R, Haro JM. Impact of painful physical symptoms on depression outcomes in elderly Asian patients. Int Psychogeriatr. 2014;2:305–12.
Hong J, Novick D, Montgomery W, Moneta MV, Duenas H, Peng X, et al. Real-world outcomes in patients with depression treated with duloxetine or a selective serotonin reuptake inhibitor in East Asia. Asia Pac Psychiatry. 2016;8:51–9.
Kroenke K, Shen J, Oxman TE, Williams JW Jr, Dietrich AJ. Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain. 2008;134:209–15.
Thielke SM, Fan MY, Sullivan M, Unutzer J. Pain limits the effectiveness of collaborative care for depression. Am J Geriatr Psychiatry. 2007;15:699–707.
Romera I, Perez V, Quail D, Berggren L, Lenox-Smith A, Gilaberte I. Individual residual symptoms and functional impairment in patients with depression. Psychiatry Res. 2014;220:258–62.
Jaracz J, Gattner K, Moczko J, Hauser J. Comparison of the effects of escitalopram and nortriptyline on painful symptoms in patients with major depression. Gen Hosp Psychiatry. 2015;37:36–9.
Sekine A, Hozumi S, Shimizu T. Influence of painful physical symptoms in the treatment of Japanese patients with melancholic major depressive disorder: a prospective cohort study. Psychiatry Res. 2016;242:240–4.
Arnold LM, Meyers AL, Sunderajan P, Montano CB, Kass E, Trivedi M, et al. The effect of pain on outcomes in a trial of duloxetine treatment of major depressive disorder. Ann Clin Psychiatry. 2008;20:187–93.
Collaborators GBDMD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50.
Fishbain DA, Cole B, Lewis JE, Gao J. Does pain interfere with antidepressant depression treatment response and remission in patients with depression and pain? An evidence-based structured review. Pain Med. 2014;15:1522–39.
Gameroff MJ, Olfson M. Major depressive disorder, somatic pain, and health care costs in an urban primary care practice. J Clin Psychiatry. 2006;67:1232–9.
Novick JS, Stewart JW, Wisniewski SR, Cook IA, Manev R, Nierenberg AA, et al. Clinical and demographic features of atypical depression in outpatients with major depressive disorder: preliminary findings from STAR*D. J Clin Psychiatry. 2005;66:1002–11.
Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165:342–51.
Lin EH, Tang L, Katon W, Hegel MT, Sullivan MD, Unutzer J. Arthritis pain and disability: response to collaborative depression care. Gen Hosp Psychiatry. 2006;28:482–6.
Jann MW, Slade JH. Antidepressant agents for the treatment of chronic pain and depression. Pharmacotherapy. 2007;27:1571–87.
Julius D, Basbaum AI. Molecular mechanisms of nociception. Nature. 2001;413:203–10.
Pancrazio JJ, Kamatchi GL, Roscoe AK, Lynch C 3rd. Inhibition of neuronal Na+ channels by antidepressant drugs. J Pharm Exp Ther. 1998;284:208–14.
Hooten WM, Townsend CO, Sletten CD. The triallelic serotonin transporter gene polymorphism is associated with depressive symptoms in adults with chronic pain. J Pain Res. 2017;10:1071–8.
Kunz M, Hennig J, Karmann AJ, Lautenbacher S. Relationship of 5-HTTLPR polymorphism with various factors of pain processing: subjective experience, motor responsiveness and catastrophizing. PLoS One. 2016;11:e0153089.
Sachau J, Bruckmueller H, Gierthmuhlen J, Magerl W, May D, Binder A, et al. The serotonin receptor 2A (HTR2A) rs6313 variant is associated with higher ongoing pain and signs of central sensitization in neuropathic pain patients. Eur J Pain. 2021;25:595–611.
Linnstaedt SD, Riker KD, Rueckeis CA, Kutchko KM, Lackey L, McCarthy KR, et al. A functional riboSNitch in the 3′ untranslated region of FKBP5 Alters MicroRNA-320a binding efficiency and mediates vulnerability to chronic post-traumatic pain. J Neurosci. 2018;38:8407–20.
Sutherland HG, Maher BH, Rodriguez-Acevedo AJ, Haupt LM, Griffiths LR. Investigation of brain-derived neurotrophic factor (BDNF) gene variants in migraine. Headache. 2014;54:1184–93.
Azoulay D, Abed S, Sfadi A, Sheleg O, Shaoul E, Shehadeh M, et al. Low brain-derived neurotrophic factor protein levels and single-nucleotide polymorphism Val66Met are associated with peripheral neuropathy in type II diabetic patients. Acta Diabetol. 2020;57:891–8.
Hooten WM, Hu D, Cunningham JM. Effects of the ABCB1 c.3435C>T (rs1045642) polymorphism on heat pain perception in opioid-free adults with chronic pain. Anesth Analg. 2021;133:1028–35.
Reyes-Gibby CC, Wang J, Yeung SJ, Chaftari P, Yu RK, Hanna EY, et al. Genome-wide association study identifies genes associated with neuropathy in patients with head and neck cancer. Sci Rep. 2018;8:8789.
Tsai CK, Liang CS, Lin GY, Tsai CL, Lee JT, Sung YF, et al. Identifying genetic variants for age of migraine onset in a Han Chinese population in Taiwan. J Headache Pain. 2021;22:89.
Fabbri C, Crisafulli C, Calabro M, Spina E, Serretti A. Progress and prospects in pharmacogenetics of antidepressant drugs. Expert Opin Drug Metab Toxicol. 2016;12:1157–68.
Liu JJ, Wei YB, Strawbridge R, Bao Y, Chang S, Shi L, et al. Peripheral cytokine levels and response to antidepressant treatment in depression: a systematic review and meta-analysis. Mol Psychiatry. 2020;25:339–50.
Elman I, Zubieta JK, Borsook D. The missing p in psychiatric training: why it is important to teach pain to psychiatrists. Arch Gen Psychiatry. 2011;68:12–20.
Schneider E, Linden M, Weigmann H, Wagner T, Quail D, Hundemer HP, et al. Early reduction in painful physical symptoms is associated with improvements in long-term depression outcomes in patients treated with duloxetine. BMC Psychiatry. 2011;11:150.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14:162–73.
McQuay HJ, Tramer M, Nye BA, Carroll D, Wiffen PJ, Moore RA. A systematic review of antidepressants in neuropathic pain. Pain. 1996;68:217–27.
Arnold LM, Lu Y, Crofford LJ, Wohlreich M, Detke MJ, Iyengar S, et al. A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum. 2004;50:2974–84.
Brannan SK, Mallinckrodt CH, Brown EB, Wohlreich MM, Watkin JG, Schatzberg AF. Duloxetine 60 mg once-daily in the treatment of painful physical symptoms in patients with major depressive disorder. J Psychiatr Res. 2005;39:43–53.
Rowbotham MC, Goli V, Kunz NR, Lei D. Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain. 2004;110:697–706.
Ozyalcin SN, Talu GK, Kiziltan E, Yucel B, Ertas M, Disci R. The efficacy and safety of venlafaxine in the prophylaxis of migraine. Headache. 2005;45:144–52.
Gaynor PJ, Gopal M, Zheng W, Martinez JM, Robinson MJ, Marangell LB. A randomized placebo-controlled trial of duloxetine in patients with major depressive disorder and associated painful physical symptoms. Curr Med Res Opin. 2011;27:1849–58.
Brecht S, Courtecuisse C, Debieuvre C, Croenlein J, Desaiah D, Raskin J, et al. Efficacy and safety of duloxetine 60 mg once daily in the treatment of pain in patients with major depressive disorder and at least moderate pain of unknown etiology: a randomized controlled trial. J Clin Psychiatry. 2007;68:1707–16.
Gaynor PJ, Gopal M, Zheng W, Martinez JM, Robinson MJ, Hann D, et al. Duloxetine versus placebo in the treatment of major depressive disorder and associated painful physical symptoms: a replication study. Curr Med Res Opin. 2011;27:1859–67.
Acknowledgements
JJL and YBW are supported by National Natural Science Foundation of China (JJL, 82171530; YBW, 82001430). PD is supported by the Ministry of Science and Technology of China (STI2030-Major Projects 2021ZD0202105).
Funding
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
JJL, YBW, PD and JS conceptualized and initiated the study. JJL, XH and YPB screened the text. JJL and XH analyzed the data. JJL and YBW created the forest plots. JJL, LL, and XH wrote the first draft of the manuscript with input from YBW and JS. YBW and YPB proofread the manuscript. JJL, YBW, PD, OMW and JRK revised the manuscript. All authors contributed to the design of the study and the final manuscript. The corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, J.J., Huang, X., Bao, YP. et al. Painful physical symptoms and antidepressant treatment outcome in depression: a systematic review and meta-analysis. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02496-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02496-7