Abstract
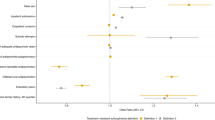
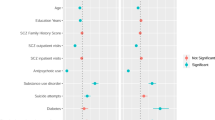
Using Swedish registers, we examine whether the prescription of and the response to antidepressants (AD), mood stabilizers (MS), and antipsychotics (AP) in the treatment of, respectively, major depression (MD), bipolar disorder (BD), and schizophrenia (SZ), are influenced by familial-genetic risk. We examined individuals born in Sweden 1960–1995 with a first diagnosis of MD (n = 257,177), BD (n = 23,032), and SZ (n = 4248) from 2006 to 2018. Drug classes and Defined Daily Dose (DDD) were obtained from the Pharmacy register using the Anatomical Therapeutic Chemical system. We utilized the Familial Genetic Risk Scores (FGRS) calculated from morbidity risks in first- through fifth degree relatives. Treatment with antidepressants (AD) in MD, mood-stabilizers (MS) in BD, and antipsychotics (AP) in SZ were associated with significantly higher disorder-specific familial-genetic risks. Using dosage trajectory analysis of AD, MS, and AP treatment for MD, BD, and SZ, respectively, familial-genetic risk was positively associated with higher and/or increasing drug dosages over time. For MD and BD, examining cases started on the most common pharmacologic treatment class (SSRIs for MD and “other anti-epileptics” for BD), familial-genetic risks were significantly lower in those who did not versus did later receive treatment from other AD and MS classes, respectively. Higher familial-genetic risk for BD predicted switching AD medication in cases of MD. Among pharmacologically treated cases of BD, familial-genetic risk was significantly higher for those treated with lithium. In a large population-based patient cohort, we found evidence of a wide-spread association between higher familial-genetic risk and i) increased likelihood of receiving pharmacologic treatment but 2) responding more poorly to it—as indicated by a switching of medications -- and/or requiring higher doses. Further investigations into the clinical utility of genetic risk scores in the clinical managements of MD, BD, and SZ are warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Jan Sundquist MD, Ph.D. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Grof P, Duffy A, Cavazzoni P, Grof E, Garnham J, MacDougall M, et al. Is response to prophylactic lithium a familial trait? J Clin Psychiatry. 2002;63:942–7.
Uher R. Genes, environment, and individual differences in responding to treatment for depression. Harv Rev Psychiatry. 2011;19:109–24.
Franchini L, Serretti A, Gasperini M, Smeraldi E. Familial concordance of fluvoxamine response as a tool for differentiating mood disorder pedigrees. J Psychiatr Res. 1998;32:255–9.
Malhotra AK, Murphy GM Jr, Kennedy JL. Pharmacogenetics of psychotropic drug response. Am J Psychiatry. 2004;161:780–96.
Johnson D, Wilke MA, Lyle SM, Kowalec K, Jorgensen A, Wright GE, et al. A systematic review and analysis of the use of polygenic scores in pharmacogenomics. Clin Pharmacol Ther. 2022;111:919–30.
Meerman JJ, Ter Hark SE, Janzing JG, Coenen MJ. The potential of polygenic risk scores to predict antidepressant treatment response in major depression: a systematic review. J Affect Disord. 2022;304:1–11.
Fabbri C, Serretti A. Genetics of treatment outcomes in major depressive disorder: present and future. Clin Psychopharmacol Neurosci. 2020;18:1–9.
Pain O, Hodgson K, Trubetskoy V, Ripke S, Marshe VS, Adams MJ, et al. Identifying the common genetic basis of antidepressant response. Biol Psychiatry Glob Open Sci. 2022;2:115–26.
Nøhr AK, Forsingdal A, Moltke I, Howes OD, Vitezic M, Albrechtsen A, et al. Polygenic heterogeneity in antidepressant treatment and placebo response. Transl Psychiatry. 2022;12:456.
Wimberley T, Gasse C, Meier SM, Agerbo E, MacCabe JH, Horsdal HT. Polygenic risk score for schizophrenia and treatment-resistant schizophrenia. Schizophr Bull. 2017;43:1064–9.
Werner MCF, Wirgenes KV, Haram M, Bettella F, Lunding SH, Rødevand L, et al. Indicated association between polygenic risk score and treatment-resistance in a naturalistic sample of patients with schizophrenia spectrum disorders. Schizophr Res. 2020;218:55–62.
Kowalec K, Lu Y, Sariaslan A, Song J, Ploner A, Dalman C, et al. Increased schizophrenia family history burden and reduced premorbid IQ in treatment-resistant schizophrenia: a Swedish National Register and Genomic Study. Mol Psychiatry. 2021;26:4487–95.
Zhang J-P, Robinson D, Yu J, Gallego J, Fleischhacker WW, Kahn RS, et al. Schizophrenia polygenic risk score as a predictor of antipsychotic efficacy in first-episode psychosis. Am J Psychiatry. 2019;176:21–8.
Gasse C, Wimberley T, Wang Y, Mors O, Børglum A, Als TD, et al. Schizophrenia polygenic risk scores, urbanicity and treatment-resistant schizophrenia. Schizophr Res. 2019;212:79–85.
Fusar-Poli L, Rutten BP, van Os J, Aguglia E, Guloksuz S. Polygenic risk scores for predicting outcomes and treatment response in psychiatry: hope or hype? Int Rev Psychiatry. 2022;34:663–75.
Kendler KS, Ohlsson H, Sundquist J, Sundquist K. Family genetic risk scores and the genetic architecture of major affective and psychotic disorders in a Swedish national sample. JAMA Psychiatry. 2021;78:735–43.
Kendler KS, Ohlsson H, Sundquist J, Sundquist K. The patterns of family genetic risk scores for eleven major psychiatric and substance use disorders in a Swedish national sample. Transl Psychiatry. 2021;11:1–8.
Kendler K, Ohlsson H, Sundquist J, Sundquist K. The impact of sex, age at onset, recurrence, mode of ascertainment and medical complications on the family genetic risk score profiles for alcohol use disorder. Psychol Med. 2023;53:1732–40.
Kendler KS, Ohlsson H, Mościcki EK, Sundquist J, Edwards AC, Sundquist K. Genetic liability to suicide attempt, suicide death and psychiatric and substance use disorders on the risk for suicide attempt and suicide death: a Swedish national study. Psychol Med. 2023;53:1639–48.
Kendler KS, Ohlsson H, Bacanu S, Sundquist J, Sundquist K. Differences in genetic risk score profiles for drug use disorder, major depression and ADHD as a function of sex, age at onset, recurrence, mode of ascertainment and treatment. Psychol Med. 2023;53:3448–60.
Kendler KS, Ohlsson H, Sundquist J, Sundquist K. The moderation of the genetic risk for alcohol and drug use disorders in a swedish national sample by the genetic aptitude for educational attainment. Psychol Med. 2023;53:3077–84.
Kendler KS, Rosmalen JGM, Ohlsson H, Sundquist J, Sundquist K. A distinctive profile of family genetic risk scores in a Swedish national sample of cases of fibromyalgia, irritable bowel syndrome, and chronic fatigue syndrome compared to rheumatoid arthritis and major depression. Psychol Med. 2023;53:3879–86.
Fanelli G, Benedetti F, Kasper S, Zohar J, Souery D, Montgomery S, et al. Higher polygenic risk scores for schizophrenia may be suggestive of treatment non-response in major depressive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;108:110170.
Amare AT, Schubert KO, Hou L, Clark SR, Papiol S, Heilbronner U, et al. Association of polygenic score for schizophrenia and HLA antigen and inflammation genes with response to lithium in bipolar affective disorder: a genome-wide association study. JAMA Psychiatry. 2018;75:65–74.
Lin BD, Pinzón-Espinosa J, Blouzard E, Van Der Horst MZ, Okhuijsen-Pfeifer C, Van Eijk KR, et al. Associations between polygenic risk score loading, psychosis liability, and clozapine use among individuals with schizophrenia. JAMA Psychiatry. 2023;80:181–5.
WHO Collaborating Centre for Drug Statistics Methodology. Definition and general consideration 2023 [Available from: http://www.whocc.no/ddd/definition_and_general_considera/.
FASS [Available from: https://www.fass.se/LIF/startpage?userType=0.
Grunze H, Schlösser S, Amann B, Walden J. Anticonvulsant drugs in bipolar disorder. Dialog Clin Neurosci. 1999;1:24–40.
Kato T. Current understanding of bipolar disorder: toward integration of biological basis and treatment strategies. Psychiatry Clin Neurosci. 2019;73:526–40.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38.
Vrieze SI. Model selection and psychological theory: a discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol Methods. 2012;17:228–43.
Côté S, Tremblay RE, Nagin D, Zoccolillo M, Vitaro F. The development of impulsivity, fearfulness, and helpfulness during childhood: Patterns of consistency and change in the trajectories of boys and girls. J Child Psychol Psychiatry. 2002;43:609–18.
Rahman S, Wiberg M, Alexanderson K, Jokinen J, Tanskanen A, Mittendorfer-Rutz E. Trajectories of antidepressant medication use in individuals before and after being granted disability pension due to common mental disorders-a nationwide register-based study. BMC Psychiatry. 2018;18:1–10.
SAS Institute I. SAS/STAT® online documentation, version 9.4. Cary, N.C.: SAS Institute, Inc; 2012.
Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry. 2003;60:1187–92.
McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497–502.
Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157:1552–62.
Facal F, Costas J. Polygenic risk scores for schizophrenia and treatment resistance: new data, systematic review and meta-analysis. Schizophr Res. 2023;252:189–97.
Lichtenstein P, Bjork C, Hultman CM, Scolnick E, Sklar P, Sullivan PF. Recurrence risks for schizophrenia in a Swedish national cohort. Psychol Med. 2006;36:1417–25.
Sellgren C, Landen M, Lichtenstein P, Hultman CM, Langstrom N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124:447–53.
Ekholm B, Ekholm A, Adolfsson R, Vares M, Osby U, Sedvall GC, et al. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nord J Psychiatry. 2005;59:457–64.
Kendler KS, Ohlsson H, Lichtenstein P, Sundquist J, Sundquist K. The genetic epidemiology of treated major depression in Sweden. Am J Psychiatry. 2018;175:1137–44.
Sundquist J, Ohlsson H, Sundquist K, Kendler KS. Common adult psychiatric disorders in Swedish primary care (where most mental health patients are treated). BMC Psychiatry. 2017;17:235.
Bech P. Diagnostic and classification tradition of mental disorders in the 20th century in Scandinavia. In: Satorius N, editor. Sources and traditions of classification in psychiatry. Toronto: Hogrefe & Huber; 1990. p. 153–70.
Langfeldt G. Diagnosis and prognosis of schizophrenia. Proc R Soc Med. 1960;53:1047–52.
Fors BM, Isacson D, Bingefors K, Widerlöv B. Mortality among persons with schizophrenia in Sweden: an epidemiological study. Nord J Psychiatry. 2007;61:252–9.
Hujoel ML, Gazal S, Loh P-R, Patterson N, Price AL. Liability threshold modeling of case–control status and family history of disease increases association power. Nat Genet. 2020;52:541–7.
Krebs MB Appadurai V, Hellberg KLJ, Ohlsson H, Steinbach J, Pedersen EM, et al. The relationship between genotype- and phenotype-based estimates of genetic liability to human psychiatric disorders, in practice and in theory. medRxiv. 2023:epub.
Acknowledgements
Location of where work was done: Lund University, Virginia Commonwealth University.
Funding
This project was supported by grants from the Swedish Research Council (2020-01175).
Author information
Authors and Affiliations
Contributions
KSK developed the hypothesis and HO performed the statistical analyses. KSK drafted the manuscript with input from JS, KS, and HO, who all reviewed the MS. JS and KS oversaw and kept updated the registry resources needed for these analyses.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kendler, K.S., Ohlsson, H., Sundquist, J. et al. The relationship between familial-genetic risk and pharmacological treatment in a Swedish national sample of patients with major depression, bipolar disorder, and schizophrenia. Mol Psychiatry (2023). https://doi.org/10.1038/s41380-023-02365-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-023-02365-9