Abstract
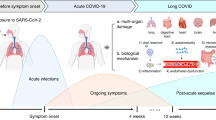
The increasing number of coronavirus disease 2019 (COVID-19) infections have highlighted the long-term consequences of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection called long COVID. Although the concept and definition of long COVID are described differently across countries and institutions, there is general agreement that it affects multiple systems, including the immune, respiratory, cardiovascular, gastrointestinal, neuropsychological, musculoskeletal, and other systems. This review aims to provide a synthesis of published epidemiology, symptoms, and risk factors of long COVID. We also summarize potential pathophysiological mechanisms and biomarkers for precise prevention, early diagnosis, and accurate treatment of long COVID. Furthermore, we suggest evidence-based guidelines for the comprehensive evaluation and management of long COVID, involving treatment, health systems, health finance, public attitudes, and international cooperation, which is proposed to improve the treatment strategies, preventive measures, and public health policy making of long COVID.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl J Med. 2020;382:727–33.
WHO. WHO coronavirus (COVID-19) dashboard. 2023. https://covid19.who.int/ (Accessed 1 May 2023).
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–93.
Cevik M, Kuppalli K, Kindrachuk J, Peiris M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ. 2020;371:m3862.
Kondratiuk AL, Pillay TD, Kon OM, Lalvani A. A conceptual framework to accelerate the clinical impact of evolving research into long COVID. Lancet Infect Dis. 2021;21:756–7.
Wulf Hanson S, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, Ballouz T, et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328:1604–15.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–15.
Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. BMJ. 2021;374:n1648.
Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22:e102–e107.
Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026.
Datta SD, Talwar A, Lee JT. A proposed framework and timeline of the spectrum of disease due to SARS-CoV-2 infection: illness beyond acute infection and public health implications. JAMA. 2020;324:2251–2.
Shah W, Hillman T, Playford ED, Hishmeh L. Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 2021;372:n136.
WHO. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1.
Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med. 2022;10:863–76.
Pazukhina E, Andreeva M, Spiridonova E, Bobkova P, Shikhaleva A, El-Taravi Y, et al. Prevalence and risk factors of post-COVID-19 condition in adults and children at 6 and 12 months after hospital discharge: a prospective, cohort study in Moscow (StopCOVID). BMC Med. 2022;20:244.
Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9:1275–87.
Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18:e1003773.
Antonelli M, Pujol JC, Spector TD, Ourselin S, Steves CJ. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet. 2022;399:2263–4.
Perlis RH, Santillana M, Ognyanova K, Safarpour A, Lunz Trujillo K, Simonson MD, et al. Prevalence and correlates of long COVID symptoms among US adults. JAMA Netw Open. 2022;5:e2238804.
Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226:1593–607.
Zeng N, Zhao YM, Yan W, Li C, Lu QD, Liu L et al. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol Psychiatry 2023;28:423–33.
Thompson EJ, Williams DM, Walker AJ, Mitchell RE, Niedzwiedz CL, Yang TC, et al. Long COVID burden and risk factors in 10 UK longitudinal studies and electronic health records. Nat Commun. 2022;13:3528.
Alkodaymi MS, Omrani OA, Fawzy NA, Shaar BA, Almamlouk R, Riaz M, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022;28:657–66.
Montefusco L, Ben Nasr M, D'Addio F, Loretelli C, Rossi A, Pastore I, et al. Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection. Nat Metab. 2021;3:774–85.
Fernández-Ortega M, Ponce-Rosas ER, Muñiz-Salinas DA, Rodríguez-Mendoza O, Nájera Chávez P, Sánchez-Pozos V, et al. Cognitive dysfunction, diabetes mellitus 2 and arterial hypertension: Sequelae up to one year of COVID-19. Travel Med Infect Dis. 2023;52:102553.
Lee JH, Yim JJ, Park J. Pulmonary function and chest computed tomography abnormalities 6-12 months after recovery from COVID-19: a systematic review and meta-analysis. Respir Res. 2022;23:233.
Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered From coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1265–73.
Lam MH, Wing YK, Yu MW, Leung CM, Ma RC, Kong AP, et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med. 2009;169:2142–7.
Epstein L, Wong KK, Kallen AJ, Uyeki TM. Post-Ebola signs and symptoms in U.S. survivors. N. Engl J Med. 2015;373:2484–6.
Choudhury A, Tariq R, Jena A, Vesely EK, Singh S, Khanna S, et al. Gastrointestinal manifestations of long COVID: a systematic review and meta-analysis. Ther Adv Gastroenterol. 2022;15:17562848221118403.
Stefanou MI, Palaiodimou L, Bakola E, Smyrnis N, Papadopoulou M, Paraskevas GP, et al. Neurological manifestations of long-COVID syndrome: a narrative review. Ther Adv Chronic Dis. 2022;13:20406223221076890.
Daroische R, Hemminghyth MS, Eilertsen TH, Breitve MH, Chwiszczuk LJ. Cognitive impairment after COVID-19-a review on objective test data. Front Neurol. 2021;12:699582.
Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604:697–707.
Bellan M, Soddu D, Balbo PE, Baricich A, Zeppegno P, Avanzi GC, et al. Respiratory and psychophysical sequelae among patients with COVID-19 four months after hospital discharge. JAMA Netw Open. 2021;4:e2036142.
McMahon DE, Gallman AE, Hruza GJ, Rosenbach M, Lipoff JB, Desai SR, et al. Long COVID in the skin: a registry analysis of COVID-19 dermatological duration. Lancet Infect Dis. 2021;21:313–4.
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–32.
Wise J. Long covid: hair loss and sexual dysfunction are among wider symptoms, study finds. BMJ. 2022;378:o1887.
WHO. Tracking SARS-CoV-2 variants. 2022. https://www.who.int/activities/tracking-SARS-CoV-2-variants.
Olaiz-Fernandez G, Vicuna de Anda FJ, Diaz-Ramirez JB, Fajardo Dolci GE, Bautista-Carbajal P, Angel-Ambrocio AH, et al. Effect of Omicron on the prevalence of COVID-19 in international travelers at the Mexico city international airport. December 16th, 2021 to January 31st, 2022. Travel Med Infect Dis. 2022;49:102361.
Ra SH, Lim JS, Kim GU, Kim MJ, Jung J, Kim SH. Upper respiratory viral load in asymptomatic individuals and mildly symptomatic patients with SARS-CoV-2 infection. Thorax. 2021;76:61–3.
Ralli M, Morrone A, Arcangeli A, Ercoli L. Asymptomatic patients as a source of transmission of COVID-19 in homeless shelters. Int J Infect Dis. 2021;103:243–5.
Fiercehealthcare. New data offer glimpse at potential impact of emerging COVID variants. 2022. https://www.fiercehealthcare.com/payers/preliminary-data-point-challenges-new-covid-variants-present.
Cao Y, Jian F, Wang J, Yu Y, Song W, Yisimayi A et al. Imprinted SARS-CoV-2 humoral immunity induces convergent Omicron RBD evolution. Nature 2023;614:521–29.
Qu P, Evans JP, Faraone JN, Zheng YM, Carlin C, Anghelina M et al. Enhanced neutralization resistance of SARS-CoV-2 Omicron subvariants BQ.1, BQ.1.1, BA.4.6, BF.7, and BA.2.75.2. Cell Host Microbe 2023;31:9–17.e13.
Sheward DJ, Kim C, Fischbach J, Sato K, Muschiol S, Ehling RA, et al. Omicron sublineage BA.2.75.2 exhibits extensive escape from neutralising antibodies. Lancet Infect Dis. 2022;22:1538–40.
Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9:815–27.
Ledford H. How severe are omicron infections? Nature. 2021;600:577–8.
Hui KPY, Ho JCW, Cheung MC, Ng KC, Ching RHH, Lai KL, et al. SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature. 2022;603:715–20.
Office for National Statistics (ONS). Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK. 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/3november2022.
Wang S, Quan L, Chavarro JE, Slopen N, Kubzansky LD, Koenen KC, et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions. JAMA psychiatry. 2022;79:1081–91.
Kayaaslan B, Eser F, Kalem AK, Kaya G, Kaplan B, Kacar D, et al. Post-COVID syndrome: a single-center questionnaire study on 1007 participants recovered from COVID-19. J Med Virol. 2021;93:6566–74.
Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–31.
Subramanian A, Nirantharakumar K, Hughes S, Myles P, Williams T, Gokhale KM, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28:1706–14.
Bowe B, Xie Y, Al-Aly Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat Med. 2022;28:2398–405.
Carvalho-Schneider C, Laurent E, Lemaignen A, Beaufils E, Bourbao-Tournois C, Laribi S, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2021;27:258–63.
Peghin M, Palese A, Venturini M, De Martino M, Gerussi V, Graziano E, et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin Microbiol Infect. 2021;27:1507–13.
de Oliveira JF, de Ávila RE, de Oliveira NR, da Cunha Severino Sampaio N, Botelho M, Gonçalves FA, et al. Persistent symptoms, quality of life, and risk factors in long COVID: a cross-sectional study of hospitalized patients in Brazil. Int J Infect Dis. 2022;122:1044–51.
Boglione L, Meli G, Poletti F, Rostagno R, Moglia R, Cantone M, et al. Risk factors and incidence of long-COVID syndrome in hospitalized patients: does remdesivir have a protective effect? QJM. 2022;114:865–71.
Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022;28:611.e619–611.e616.
Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post-COVID-19 manifestations. Int J Clin Pr. 2021;75:e13746.
Galal I, Hussein AARM, Amin MT, Saad MM, Zayan HEE, Abdelsayed MZ, et al. Determinants of persistent post-COVID-19 symptoms: value of a novel COVID-19 symptom score. Egypt J Bronchol. 2021;15:10.
Huang Y, Pinto MD, Borelli JL, Asgari Mehrabadi M, Abrahim HL, Dutt N, et al. COVID symptoms, symptom clusters, and predictors for becoming a long-hauler looking for clarity in the haze of the pandemic. Clin Nurs Res. 2022;31:1390–8.
FAIR Health. A detailed study of patients with long-haul COVID. 2021. https://s3.amazonaws.com/media2.fairhealth.org/whitepaper/asset/A%20Detailed%20Study%20of%20Patients%20with%20Long-Haul%20COVID--An%20Analysis%20of%20Private%20Healthcare%20Claims--A%20FAIR%20Health%20White%20Paper.pdf.
Strahm C, Seneghini M, Güsewell S, Egger T, Leal-Neto O, Brucher A, et al. Symptoms compatible with long coronavirus disease (COVID) in healthcare workers with and without severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection-results of a prospective multicenter cohort. Clin Infect Dis. 2022;75:e1011–19.
Hastie CE, Lowe DJ, McAuley A, Winter AJ, Mills NL, Black C, et al. Outcomes among confirmed cases and a matched comparison group in the Long-COVID in Scotland study. Nat Commun. 2022;13:5663.
Yomogida K, Zhu S, Rubino F, Figueroa W, Balanji N, Holman E. Post-acute sequelae of SARS-CoV-2 infection among adults aged ≥18 years - Long Beach, California, April 1-December 10, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:1274–7.
Poyraz BÇ, Poyraz CA, Olgun Y, Gürel Ö, Alkan S, Özdemir YE, et al. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatry Res. 2021;295:113604.
Pillay J, Rahman S, Guitard S, Wingert A, Hartling L. Risk factors and preventive interventions for post Covid-19 condition: systematic review. Emerg Microbes Infect. 2022;11:2762–80.
Singh B, Gornet M, Sims H, Kisanga E, Knight Z, Segars J. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its effect on gametogenesis and early pregnancy. Am J Reprod Immunol. 2020;84:e13351.
Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020;20:442–7.
Zhao Y, Shi L, Jiang Z, Zeng N, Mei H, Lu Y et al. The phenotype and prediction of long-term physical, mental and cognitive COVID-19 sequelae 20 months after recovery, a community-based cohort study in China. Mol Psychiatry. 2023;28:1793–1801.
Osmanov IM, Spiridonova E, Bobkova P, Gamirova A, Shikhaleva A, Andreeva M et al. Risk factors for post-COVID-19 condition in previously hospitalised children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur Respir J. 2022;59:2101341.
Yuan K, Gong YM, Liu L, Sun YK, Tian SS, Wang YJ, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry. 2021;26:4982–98.
Scott HR, Stevelink SAM, Gafoor R, Lamb D, Carr E, Bakolis I, et al. Prevalence of post-traumatic stress disorder and common mental disorders in health-care workers in England during the COVID-19 pandemic: a two-phase cross-sectional study. Lancet Psychiatry. 2023;10:40–9.
Ourworldindata. Coronavirus (COVID-19) vaccinations. 2023. https://ourworldindata.org/covid-vaccinations.
Moore S, Hill EM, Dyson L, Tildesley MJ, Keeling MJ. Retrospectively modeling the effects of increased global vaccine sharing on the COVID-19 pandemic. Nat Med. 2022;28:2416–23.
Koc HC, Xiao J, Liu W, Li Y, Chen G. Long COVID and its management. Int J Biol Sci. 2022;18:4768–80.
Antonelli M, Penfold RS, Merino J, Sudre CH, Molteni E, Berry S, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID symptom study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22:43–55.
Ayoubkhani D, Bosworth ML, King S, Pouwels KB, Glickman M, Nafilyan V, et al. Risk of long COVID in people infected with severe acute respiratory syndrome coronavirus 2 after 2 doses of a coronavirus disease 2019 vaccine: community-based, matched cohort study. Open Forum Infect Dis. 2022;9:ofac464.
Azzolini E, Levi R, Sarti R, Pozzi C, Mollura M, Mantovani A, et al. Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers. JAMA. 2022;328:676–8.
Gao P, Liu J, Liu M Effect of COVID-19 vaccines on reducing the risk of long COVID in the real world: a systematic review and meta-analysis. Int J Environ Res Public Health 2022;19:12422.
Taghioff SM, Slavin BR, Holton T, Singh D. Examining the potential benefits of the influenza vaccine against SARS-CoV-2: a retrospective cohort analysis of 74,754 patients. PloS One. 2021;16:e0255541.
Ahamed J, Laurence J Long COVID endotheliopathy: hypothesized mechanisms and potential therapeutic approaches. J Clin Invest. 2022;132:e161167.
Castanares-Zapatero D, Chalon P, Kohn L, Dauvrin M, Detollenaere J, Maertens de Noordhout C, et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med. 2022;54:1473–87.
Mantovani A, Morrone MC, Patrono C, Santoro MG, Schiaffino S, Remuzzi G, et al. Long Covid: where we stand and challenges ahead. Cell Death Differ. 2022;29:1891–1900.
Monje M, Iwasaki A .The neurobiology of long COVID. Neuron. 2022;110:3484–96.
Bakar Siddiq M, Rasker J. COVID-19, long COVID, and psychosomatic manifestations: a possible burden on existing rheumatology facilities. Heart Mind. 2022;6:195–202.
Stein SR, Ramelli SC, Grazioli A, Chung JY, Singh M, Yinda CK et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. 2022;612:758–63.
Li Q, Zheng XS, Shen XR, Si HR, Wang X, Wang Q, et al. Prolonged shedding of severe acute respiratory syndrome coronavirus 2 in patients with COVID-19. Emerg Microbes Infect. 2020;9:2571–7.
Han Y, Yuan K, Wang Z, Liu WJ, Lu ZA, Liu L, et al. Neuropsychiatric manifestations of COVID-19, potential neurotropic mechanisms, and therapeutic interventions. Transl Psychiatry. 2021;11:499.
de Melo GD, Lazarini F, Levallois S, Hautefort C, Michel V, Larrous F et al. COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci Transl Med. 2021;13:eabf8396.
Merad M, Blish CA, Sallusto F, Iwasaki A. The immunology and immunopathology of COVID-19. Science. 2022;375:1122.
Cohen JI. Epstein-Barr virus infection. N. Engl J Med. 2000;343:481–92.
Gold JE, Okyay RA, Licht WE, Hurley DJ. Investigation of long COVID prevalence and its relationship to epstein-barr virus reactivation. Pathogens. 2021;10:763.
Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185:881–895.e820.
Gaebler C, Wang Z, Lorenzi JCC, Muecksch F, Finkin S, Tokuyama M, et al. Evolution of antibody immunity to SARS-CoV-2. Nature. 2021;591:639–44.
Theofilopoulos AN, Kono DH, Baccala R. The multiple pathways to autoimmunity. Nat Immunol. 2017;18:716–24.
Wallukat G, Hohberger B, Wenzel K, Furst J, Schulze-Rothe S, Wallukat A, et al. Functional autoantibodies against G-protein coupled receptors in patients with persistent long-COVID-19 symptoms. J Transl Autoimmun. 2021;4:100100.
Klein J, Wood J, Jaycox J, Lu P, Dhodapkar RM, Gehlhausen JR et al. Distinguishing features of long COVID identified through immune profiling. medRxiv 2022;2022.08.09.22278592.
Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front Microbiol. 2021;12:698169.
Liu X, Yan W, Lu T, Han Y, Lu L. Longitudinal abnormalities in brain structure in COVID-19 patients. Neurosci Bull. 2022;38:1608–12.
Tian T, Wu J, Chen T, Li J, Yan S, Zhou Y et al. Long-term follow-up of dynamic brain changes in patients recovered from COVID-19 without neurological manifestations. JCI Insight. 2022;7:e155827.
Cecchetti G, Agosta F, Canu E, Basaia S, Barbieri A, Cardamone R, et al. Cognitive, EEG, and MRI features of COVID-19 survivors: a 10-month study. J Neurol. 2022;269:3400–12.
Du YY, Zhao W, Zhou XL, Zeng M, Yang DH, Xie XZ, et al. Survivors of COVID-19 exhibit altered amplitudes of low frequency fluctuation in the brain: a resting-state functional magnetic resonance imaging study at 1-year follow-up. Neural Regen Res. 2022;17:1576–81.
Pretorius E, Venter C, Laubscher GJ, Kotze MJ, Oladejo SO, Watson LR, et al. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovasc Diabetol. 2022;21:148.
Kruger A, Vlok M, Turner S, Venter C, Laubscher GJ, Kell DB, et al. Proteomics of fibrin amyloid microclots in long COVID/post-acute sequelae of COVID-19 (PASC) shows many entrapped pro-inflammatory molecules that may also contribute to a failed fibrinolytic system. Cardiovasc Diabetol. 2022;21:190.
Kell DB, Laubscher GJ, Pretorius E. A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications. Biochem J. 2022;479:537–59.
Cheng HY, Ning MX, Chen DK, Ma WT. Interactions between the gut microbiota and the host innate immune response against pathogens. Front Immunol. 2019;10:607.
Alharbi KS, Singh Y, Hassan Almalki W, Rawat S, Afzal O, Alfawaz Altamimi AS, et al. Gut microbiota disruption in COVID-19 or post-COVID illness association with severity biomarkers: a possible role of pre / pro-biotics in manipulating microflora. Chem Biol Interact. 2022;358:109898.
Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Zhan H, et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology. 2020;159:944–55.e948.
Vestad B, Ueland T, Lerum TV, Dahl TB, Holm K, Barratt-Due A, et al. Respiratory dysfunction three months after severe COVID-19 is associated with gut microbiota alterations. J Intern Med. 2022;291:801–12.
Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, et al. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021;76:396–8.
Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier CML, Patel SK, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol. 2022;23:210–6.
Bizjak DA, Stangl M, Börner N, Bösch F, Durner J, Drunin G, et al. Kynurenine serves as useful biomarker in acute, long- and post-COVID-19 diagnostics. Front Immunol. 2022;13:1004545.
Zhao J, Schank M, Wang L, Dang X, Cao D, Khanal S, et al. Plasma biomarkers for systemic inflammation in COVID-19 survivors. Proteom Clin Appl. 2022;16:e2200031.
Li H, Xiang X, Ren H, Xu L, Zhao L, Chen X, et al. Serum amyloid A is a biomarker of severe coronavirus disease and poor prognosis. J Infect. 2020;80:646–55.
Hua-Huy T, Günther S, Lorut C, Subileau M, Aubourg F, Morbieu C et al. Distal lung inflammation assessed by alveolar concentration of nitric oxide Is an individualised biomarker of severe COVID-19 pneumonia. J Pers Med 2022;12:1631.
Yang Z, Wu D, Lu S, Qiu Y, Hua Z, Tan F, et al. Plasma metabolome and cytokine profile reveal glycylproline modulating antibody fading in convalescent COVID-19 patients. Proc Natl Acad Sci USA. 2022;119:e2117089119.
Fernández-de-Las-Peñas C, Ryan-Murua P, Rodríguez-Jiménez J, Palacios-Ceña M, Arendt-Nielsen L, Torres-Macho J. Serological biomarkers at hospital admission are not related to long-term post-COVID fatigue and dyspnea in COVID-19 survivors. Respiration. 2022;101:658–65.
Sabanoglu C, Inanc IH, Polat E, Peker SA. Long-term predictive value of cardiac biomarkers in patients with COVID-19 infection. Eur Rev Med Pharm Sci. 2022;26:6396–403.
Motloch LJ, Jirak P, Gareeva D, Davtyan P, Gumerov R, Lakman I, et al. Cardiovascular biomarkers for prediction of in-hospital and 1-year post-discharge mortality in patients with COVID-19 pneumonia. Front Med (Lausanne). 2022;9:906665.
Petersen EL, Goßling A, Adam G, Aepfelbacher M, Behrendt CA, Cavus E, et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. Eur Heart J. 2022;43:1124–37.
Myhre PL, Heck SL, Skranes JB, Prebensen C, Jonassen CM, Berge T, et al. Cardiac pathology 6 months after hospitalization for COVID-19 and association with the acute disease severity. Am Heart J. 2021;242:61–70.
Tong M, Yan X, Jiang Y, Jin Z, Zhu S, Zou L, et al. Endothelial biomarkers in patients recovered from COVID-19 one year after hospital discharge: a cross-sectional study. Mediterr J Hematol Infect Dis. 2022;14:e2022033.
Puntmann VO, Martin S, Shchendrygina A, Hoffmann J, Ka MM, Giokoglu E, et al. Long-term cardiac pathology in individuals with mild initial COVID-19 illness. Nat Med. 2022;28:2117–23.
Wais T, Hasan M, Rai V, Agrawal DK. Gut-brain communication in COVID-19: molecular mechanisms, mediators, biomarkers, and therapeutics. Expert Rev Clin Immunol. 2022;18:947–60.
García-Grimshaw M, Chirino-Pérez A, Flores-Silva FD, Valdés-Ferrer SI, Vargas-Martínez M, Jiménez-Ávila AI, et al. Critical role of acute hypoxemia on the cognitive impairment after severe COVID-19 pneumonia: a multivariate causality model analysis. Neurol Sci. 2022;43:2217–29.
Alvarez M, Trent E, Goncalves BS, Pereira DG, Puri R, Frazier NA, et al. Cognitive dysfunction associated with COVID-19: prognostic role of circulating biomarkers and microRNAs. Front Aging Neurosci. 2022;14:1020092.
Kanberg N, Simrén J, Edén A, Andersson LM, Nilsson S, Ashton NJ, et al. Neurochemical signs of astrocytic and neuronal injury in acute COVID-19 normalizes during long-term follow-up. EBioMedicine. 2021;70:103512.
Sun B, Tang N, Peluso MJ, Iyer NS, Torres L, Donatelli JL et al. Characterization and biomarker analyses of post-COVID-19 complications and neurological manifestations. Cells. 2021;10:386.
Guasp M, Muñoz-Sánchez G, Martínez-Hernández E, Santana D, Carbayo Á, Naranjo L, et al. CSF biomarkers in COVID-19 associated encephalopathy and encephalitis predict long-term outcome. Front Immunol. 2022;13:866153.
Rhea EM, Logsdon AF, Hansen KM, Williams LM, Reed MJ, Baumann KK, et al. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nat Neurosci. 2021;24:368–78.
Meinhardt J, Radke J, Dittmayer C, Franz J, Thomas C, Mothes R, et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci. 2021;24:168–75.
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18–22.
Al-Hadrawi DS, Al-Rubaye HT, Almulla AF, Al-Hakeim HK, Maes M Lowered oxygen saturation and increased body temperature in acute COVID-19 largely predict chronic fatigue syndrome and affective symptoms due to Long COVID: A precision nomothetic approach. Acta Neuropsychiatr. 2022;35:76-87.
Mazza MG, Palladini M, De Lorenzo R, Magnaghi C, Poletti S, Furlan R, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun. 2021;94:138–47.
Carson G. Research priorities for long covid: refined through an international multi-stakeholder forum. BMC Med. 2021;19:84.
National institute for health and care excellence: clinical guidelines. COVID-19 rapid guideline: managing the long-term effects of COVID-19. National Institute for Health and Care Excellence (NICE) Copyright © NICE 2020: London, 2020.
Sachs JD, Karim SSA, Aknin L, Allen J, Brosbøl K, Colombo F et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. Lancet. 2022;400:1224–80.
Greenhalgh T, Sivan M, Delaney B, Evans R, Milne R. Long covid-an update for primary care. BMJ. 2022;378:e072117.
Joli J, Buck P, Zipfel S, Stengel A. Post-COVID-19 fatigue: a systematic review. Front Psychiatry. 2022;13:947973.
Gibson P, Wang G, McGarvey L, Vertigan AE, Altman KW, Birring SS, et al. Treatment of unexplained chronic cough: CHEST guideline and expert panel report. Chest. 2016;149:27–44.
Song WJ, Hui CKM, Hull JH, Birring SS, McGarvey L, Mazzone SB, et al. Confronting COVID-19-associated cough and the post-COVID syndrome: role of viral neurotropism, neuroinflammation, and neuroimmune responses. Lancet Respir Med. 2021;9:533–44.
Chamberlain Mitchell SA, Garrod R, Clark L, Douiri A, Parker SM, Ellis J, et al. Physiotherapy, and speech and language therapy intervention for patients with refractory chronic cough: a multicentre randomised control trial. Thorax. 2017;72:129–36.
National institute for health and care excellence. Atrial fibrillation: diagnosis and management NICE guideline. National Institute for Health and Care Excellence (NICE) Copyright © NICE 2020: London, 2020.
National institute for health and care excellence. Acute coronary syndromes NICE guideline. National Institute for Health and Care Excellence (NICE) Copyright © NICE 2020.: London, 2020.
Parker AM, Brigham E, Connolly B, McPeake J, Agranovich AV, Kenes MT, et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. Lancet Respir Med. 2021;9:1328–41.
Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12:29.
WHO. COVID-19 vaccines. 2022. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines.
Zheng YB, Sun J, Liu L, Zhao YM, Yan W, Yuan K, et al. COVID-19 vaccine-related psychological stress among general public in China. Front Psychiatry. 2021;12:774504.
Liu L, Ni SY, Yan W, Lu QD, Zhao YM, Xu YY, et al. Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: a systematic review, meta-analysis and call for action. EClinicalMedicine. 2021;40:101111.
Zheng YB, Shi L, Lu ZA, Que JY, Yuan K, Huang XL, et al. Mental health status of late-middle-aged adults in China during the coronavirus disease 2019 pandemic. Front Public Health. 2021;9:643988.
Gong Y, Liu X, Zheng Y, Mei H, Que J, Yuan K, et al. COVID-19 induced economic slowdown and mental health issues. Front Psychol. 2022;13:777350.
Byrne EA. Understanding long covid: nosology, social attitudes and stigma. Brain Behav Immun. 2022;99:17–24.
Yuan K, Huang XL, Yan W, Zhang YX, Gong YM, Su SZ, et al. A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. 2022;27:19–33.
Zhao YM, Liu L, Sun J, Yan W, Yuan K, Zheng YB et al. Public willingness and determinants of COVID-19 vaccination at the initial stage of mass vaccination in China. Vaccines (Basel). 2021;9:1172.
Li H, Yuan K, Sun YK, Zheng YB, Xu YY, Su SZ, et al. Efficacy and practice of facemask use in general population: a systematic review and meta-analysis. Transl Psychiatry. 2022;12:49.
Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–8.
Gong Y, Liu X, Su S, Bao Y, Kosten TR, Lu L. Addressing mental health issues amid the COVID-19 pandemic: a wake-up call. Sci Bull (Beijing). 2022;67:2259–62.
Acknowledgements
This study was supported by a grant from the National Key Research and Development Program of China (2021YFC0863700, 2019YFA0706200), Natural Science Foundation of Beijing Municipality of China (M23013), National Programs for Brain Science and Brain-like Intelligence Technology of China (STI2030-Major Projects, 2021ZD0200800, 2021ZD0200700), and the National Natural Science Foundation of China (no. 82288101, 82171514). The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be constructed as a potential conflict of interests.
Author information
Authors and Affiliations
Contributions
LL and YB proposed the topic and main idea, SS was responsible for literature search, drafting the manuscript, and making the figures, and revising all versions. XL, NZ, YZ, YZ, SW, YZ, JS, and SN contributed to the first draft. YG, ZZ, NG, KY, WY, LS, AVR, TK, and JS revised the manuscript for intellectual content. YB and LL proposed the topic of the review and commented on and revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Su, S., Zhao, Y., Zeng, N. et al. Epidemiology, clinical presentation, pathophysiology, and management of long COVID: an update. Mol Psychiatry 28, 4056–4069 (2023). https://doi.org/10.1038/s41380-023-02171-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02171-3
This article is cited by
-
Non-coding RNAs expression in SARS-CoV-2 infection: pathogenesis, clinical significance, and therapeutic targets
Signal Transduction and Targeted Therapy (2023)