Abstract
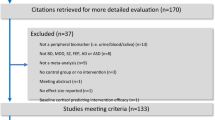
Psychotic disorders are severe mental disorders with poorly understood etiology. Biomarkers in the cerebrospinal fluid (CSF) could provide etiological clues and diagnostic tools for psychosis; however, an unbiased overview of CSF alterations in individuals with psychotic disorders is lacking. The objective of this study was to summarize all quantifiable findings in CSF from individuals with psychotic disorders compared to healthy controls (HC). Studies published before January 25th, 2023 were identified searching PubMed, EMBASE, Cochrane Library, Web of Science, ClinicalTrials.gov, and PsycINFO. Screening, full-text review, data extraction, and risk of bias assessments were performed by two independent reviewers following PRISMA guidelines. Findings in patients and healthy controls were compared and summarized using random-effects analyses and assessment of publication bias, subgroup and sensitivity analyses were performed. 145 studies, covering 197 biomarkers, were included, of which 163 biomarkers have not previously been investigated in meta-analyses. All studies showed some degree of bias. 55 biomarkers measured in CSF were associated with psychosis and of these were 15 biomarkers measured in ≥2 studies. Patients showed increased levels of noradrenaline (standardized mean difference/SMD, 0.53; 95% confidence interval/CI, 0.16 to 0.90) and its metabolite 3-methoxy-4-hydroxyphenylglycol (SMD, 0.30; 95% CI: 0.05 to 0.55), the serotonin metabolite 5-hydroxyindoleacetic acid (SMD, 0.11; 95% CI: 0.01 to 0.21), the pro-inflammatory neurotransmitter kynurenic acid (SMD, 1.58; 95% CI: 0.34 to 2.81), its precursor kynurenine (SMD,0.99; 95% CI: 0.60 to 1.38), the cytokines interleukin-6 (SMD, 0.58; 95% CI: 0.39 to 0.77) and interleukin-8 (SMD, 0.43; 95% CI: 0.24 to 0.62), the endocannabinoid anandamide (SMD, 0.78; 95% CI: 0.53 to 1.02), albumin ratio (SMD, 0.40; 95% CI: 0.08 to 0.72), total protein (SMD, 0.29; 95% CI: 0.16 to 0.43), immunoglobulin ratio (SMD, 0.45; 95% CI: 0.06 to 0.85) and glucose (SMD, 0.48; 95% CI: 0.01 to 0.94). Neurotensin (SMD, −0.67; 95% CI: −0.89 to −0.46) and γ-aminobutyric acid (SMD, −0.29; 95% CI: −0.50 to −0.09) were decreased. Most biomarkers showed no significant differences, including the dopamine metabolites homovanillic acid and 3,4-dihydroxyphenylacetic acid. These findings suggest that dysregulation of the immune and adrenergic system as well as blood-brain barrier dysfunction are implicated in the pathophysiology of psychotic disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All data used in this study can be found in the Supplementary Materials, which is available at the Molecular Psychiatry website.
References
Jongsma HE, Turner C, Kirkbride JB, Jones PB. International incidence of psychotic disorders, 2002–17: a systematic review and meta-analysis. Lancet Public Health. 2019;4:e229–44.
Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4:295–301.
Kahn RS, Sommer IE, Murray RM, Meyer-Lindenberg A, Weinberger DR, Cannon TD, et al. Schizophrenia. Nat Rev Dis Prim. 2015;1:1–23.
Mohammadi A, Rashidi E, Amooeian VG. Brain, blood, cerebrospinal fluid, and serum biomarkers in schizophrenia. Psychiatry Research. Vol. 265. Elsevier Ireland Ltd; 2018. p. 25–38.
Fernandes BS, Steiner J, Bernstein HG, Dodd S, Pasco JA, Dean OM, et al. C-reactive protein is increased in schizophrenia but is not altered by antipsychotics: Meta-analysis and implications. Mol Psychiatry. 2016;21:554–64.
Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yang S, et al. C-reactive protein is elevated in schizophrenia. Schizophr Res. 2013;143:198–202.
Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B. Meta-analysis of cytokine alterations in schizophrenia: Clinical status and antipsychotic effects. Biol Psychiatry. 2011;70:663–71.
Fraguas D, Díaz-Caneja CM, Ayora M, Hernández-Álvarez F, Rodríguez-Quiroga A, Recio S, et al. Oxidative stress and inflammation in first-episode psychosis: a systematic review and meta-analysis. Schizophr Bull. 2019;45:742–51.
Brouwer A, Luykx JJ, van Boxmeer L, Bakker SC, Kahn RS. NMDA-receptor coagonists in serum, plasma, and cerebrospinal fluid of schizophrenia patients: a meta-analysis of case-control studies. Neuroscience and Biobehavioral Reviews. Vol. 37. Pergamon; 2013. p. 1587–96.
Minichino A, Senior M, Brondino N, Zhang SH, Godwlewska BR, Burnet PWJ, et al. Measuring disturbance of the endocannabinoid system in psychosis: a systematic review and meta-analysis. JAMA Psychiatry. Vol. 76. American Medical Association; 2019. p. 914–23.
Aleksovska K, Leoncini E, Bonassi S, Cesario A, Boccia S, Frustaci A. Systematic review and meta-analysis of circulating S100B blood levels in schizophrenia. PLoS One. 2014;9:e106342.
Fernandes BS, Berk M, Turck CW, Steiner J, Gonçalves CA. Decreased peripheral brain-derived neurotrophic factor levels are a biomarker of disease activity in major psychiatric disorders: a comparative meta-analysis. Molecular Psychiatry. Vol. 19. Nature Publishing Group; 2014. p. 749–51.
Wright BLC, Lai JTF, Sinclair AJ. Cerebrospinal fluid and lumbar puncture: a practical review. J Neurol. 2012;259:1530–45.
Rutigliano G, Rocchetti M, Paloyelis Y, Gilleen J, Sardella A, Cappucciati M, et al. Peripheral oxytocin and vasopressin: Biomarkers of psychiatric disorders? A comprehensive systematic review and preliminary meta-analysis. Psychiatry Research. Vol. 241. Elsevier Ireland Ltd; 2016. p. 207–20.
Tuckwell HC, Koziol JA. A meta-analysis of homovanillic acid concentrations in schizophrenia. Int J Neurosci. 1993;73:109–14.
Tuckwell HC, Koziol JA. On the concentration of 5-hydroxyindoleacetic acid in schizophrenia: A meta-analysis. Psychiatry Res. 1996;59:239–44.
Plitman E, Iwata Y, Caravaggio F, Nakajima S, Chung JK, Gerretsen P, et al. Kynurenic acid in schizophrenia: a systematic review and meta-analysis. Schizophrenia Bulletin. Vol. 43. Oxford University Press; 2017. p. 764–77.
Cao B, Chen Y, Ren Z, Pan Z, McIntyre RS, Wang D. Dysregulation of kynurenine pathway and potential dynamic changes of kynurenine in schizophrenia: a systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews. Vol. 123. Elsevier Ltd; 2021. p. 203–14.
Gallego JA, Blanco EA, Husain-Krautter S, Madeline Fagen E, Moreno-Merino P, del Ojo-Jiménez JA, et al. Cytokines in cerebrospinal fluid of patients with schizophrenia spectrum disorders: New data and an updated meta-analysis. Schizophr Res. 2018;202:64–71.
Orlovska-Waast S, Köhler-Forsberg O, Brix SW, Nordentoft M, Kondziella D, Krogh J, et al. Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Molecular Psychiatry. Vol. 24. Nature Publishing Group; 2019. p. 869–87.
Wang AK, Miller BJ. Meta-analysis of cerebrospinal fluid cytokine and tryptophan catabolite alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder, and depression. Schizophr Bull. 2018;44:75–83.
Connemann BJ, Wolf RC, Tumani H, Brettschneider J. Cerebrospinal fluid biomarker candidates of schizophrenia: where do we stand? Eur Arch Psychiatry Clin Neurosci. 2012;262:375–91.
Hirsch J, Vacas S, Terrando N, Yuan M, Sands LP, Kramer J, et al. Perioperative cerebrospinal fluid and plasma inflammatory markers after orthopedic surgery. J Neuroinflammation. 2016;13:211.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia [2022]. Available at www.covidence.org.
Wells G, Shea B, D’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [cited 2021 Apr 12]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins J, Savovic J, Page M, Elbers R, Sterne J. Assessing risk of bias in a randomized trial. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane handbook for systematic reviews of interventions. 2nd ed. Cochrane; 2021.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Levine SZ, Rabinowitz J, Faries D, Lawson AH, Ascher-Svanum H. Treatment response trajectories and antipsychotic medications: Examination of up to 18months of treatment in the CATIE chronic schizophrenia trial. Schizophr Res. 2012;137:141–6.
Hedges LV. Estimation of effect size from a series of independent experiments. Psychol Bull. 1982;92:490–9.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Cochrane Training. Handbook. 2011 [cited 2020 Aug 10]. p. 649. Available from: https://training.cochrane.org/handbook/current.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34.
Team RC. R: A language and environment for statistical computing. Vienna, Austria: Foundation for Statistical Computing; 2020.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Albrecht P, Torrey EF, Boone E, Hicks JT, Daniel N. Raised cytomegalovirus-antibody level in cerebrospinal fluid of schizophrenic patients. Lancet. 1980;2:769–72.
Anckarsäter H, Forsman A, Blennow K. Increased CSF/serum albumin ratio: a recurrent finding in violent offenders. Acta Neurol Scand. 2005;112:48–50.
Bartfai A, Edman G, Levander SE, Schalling D, Sedvall G. Bilateral skin conductance activity, clinical symptoms and CSF monoamine metabolite levels in unmedicated schizophrenics, differing in rate of habituation. Biol Psychol. 1984;18:201–18.
Bjerkenstedt L, Edman G, Hagenfeldt L, Sedvall G, Wiesel FA. Plasma amino acids in relation to cerebrospinal fluid monoamine metabolites in schizophrenic patients and healthy controls. Br J Psychiatry. 1985;147:276–82.
Butler PD, Printz DJ, DeSanti L, Issa F, Gorman JM, Carraway RE. Neurotensin and metabolites in CSF of patients with schizophrenia and controls. Biol Psychiatry. 1996;39:300.
Checa A, Malmqvist A, Flyckt L, Schwieler L, Samuelsson M, Skogh E, et al. Cerebrospinal fluid levels of sphingolipids associate with disease severity in first episode psychosis patients. Schizophr Res. 2018;199:438–41.
Coughlin J, Hayes L, Tanaka T, Xiao M, Yolken R, Worley P, et al. Reduced superoxide dismutase-1 (SOD1) in cerebrospinal fluid of patients with early psychosis in association with clinical features. Schizophr Res. 2017;183:64–9.
Davis KL, Hollister LE, Livesey J, Berger PA. Cerebrospinal fluid acetylcholinesterase in neuropsychiatric disorders. Psychopharmacology (Berl). 1979;63:155–9.
Doran A, Boronow J, Weinberger, Wolkowitz OM, Breier A, Pickar D. Structural brain pathology in schizophrenia revisited. Prefrontal cortex pathology is inversely correlated with cerebrospinal fluid levels of homovanillic acid. Neuropsychopharmacology. 1987;1:25–32.
Dougherty GG, van Kammen DP, Yao JK. Covariance analysis of CSF amino acids in healthy normal and schizophrenia. Schizophr Bull. 2007;33:309.
Engberg G. Neuroinflammation in psychotic disorders. Int J Neuropsychopharmacol. 2012;15:28.
Engberg G, Xu C, Sellgren CM, Fatouros-Bergman H, Blennow K, Zetterberg H, et al. Synaptic elimination in first-episode psychosis subjects. Neuropsychopharmacology. 2019;44:169–70.
Engstrom G, Alling C, Blennow K, Regnell G, Traskman-Bendz L. Reduced cerebrospinal HVA concentrations and HVA/5-HIAA ratios in suicide attempters - Monoamine metabolites in 120 suicide attempters and 47 controls. Eur Neuropsychopharmacol. 1999;9:399–405.
Eratne D, Loi S, Walia N, Farrand S, Li Q, Varghese S, et al. A pilot study of the utility of cerebrospinal fluid neurofilament light chain in differentiating neurodegenerative from psychiatric disorders: A “C-reactive protein” for psychiatrists and neurologists? Aust N Z J Psychiatry. 2020;54:57–67.
Fleischhacker WW, Saria A, Humpel C, Miller C, Barnas C, Stuppack C. Decreased substance-p- and increased calcitonin gene-related peptide immunoreactivities in the cerebrospinal-fluid of drug-naive schizophrenic-patients. Schizophr Res. 1991;4:344–5.
Gerner RH, Yamada T. Altered neuropeptide concentrations in cerebrospinal fluid of psychiatric patients. Brain Res. 1982;238:298–302. https://doi.org/10.1016/0006-8993(82)90801-0.
Hattori K, Goto Y, Yoshida S, Sasayama D, Komurasaki T, Chaki S, et al. Cerebrospinal fluid biomarkers for schizophrenia revealed by a cicat proteomic analyses. Schizophr Res. 2014;153:S98–9.
Hayes L, Severance E, Leek J, Gressitt K, Rohleder C, Coughlin J, et al. Inflammatory molecular signature associated with infectious agents in psychosis. Schizophr Bull. 2014;40:963–72.
Hira S, Ozcan O, Ipcioglu O, Tutuncu R, Balibey H, Ulcay A, et al. Evaluation of one-carbon traffic in the case group of first episode psychosis by predicting methylation changes in central nervous system through measuring S-adenosyl methionine and sadenosyl homocysteine levels. Clin Chem Lab Med. 2015;53:S1348.
Hjärpe J, Söderman E, Andreou D, Sedvall GC, Agartz I, Jönsson EG. No major influence of regular tobacco smoking on cerebrospinal fluid monoamine metabolite concentrations in patients with psychotic disorder and healthy individuals. Psychiatry Res. 2018;263:30–4.
Holmes E, Tsang TM, Huang JT, Leweke FM, Koethe D, Gerth CW, et al. Metabolic profiling of CSF: evidence that early intervention may impact on disease progression and outcome in schizophrenia. PLoS Med. 2006;3:e327.
Huang JT, Leweke F, Tsang TM, Koethe D, Kranaster L, Gerth C, et al. CSF metabolic and proteomic profiles in patients prodromal for psychosis. PLoS One. 2007;2:e756.
Huang JT, Wang L, Prabakaran S, Wengenroth M, Lockstone HE, Koethe D, et al. Independent protein-profiling studies show a decrease in apolipoprotein A1 levels in schizophrenia CSF, brain and peripheral tissues. Mol Psychiatry. 2008;13:1118–28.
Husain-Krautter S, Gallego JA, Malhotra A, Rothstein TL. Proinflammatory cytokines, microRNAs and schizophrenia. J Neuroimmunol. 2014;275:62.
Husain-Krautter S, Gallego JA, Malhotra AK, Rothstein TL. A comparison of B cell repertoire in cerebrospinal fluid of patients with schizophrenia and healthy individuals. Schizophr Bull. 2015;41:S33.
Ishiwata S, Hattori K, Sasayama D, Teraishi T, Miyakawa T, Yokota Y, et al. Plasma and cerebrospinal fluid G72 protein levels in schizophrenia and major depressive disorder. Psychiatry Res. 2017;254:244–50.
Ishiwata S, Hattori K, Hidese S, Sasayama D, Miyakawa T, Matsumura R, et al. Lower cerebrospinal fluid CRH concentration in chronic schizophrenia with negative symptoms. J Psychiatr Res. 2020;127:13–9.
Janelidze S, Ventorp F, Erhardt S, Hansson O, Minthon L, Flax J, et al. Altered chemokine levels in the cerebrospinal fluid and plasma of suicide attempters. Psychoneuroendocrinology. 2013;38:853–62.
Janelidze S, Suchankova P, Ekman A, Erhardt S, Sellgren C, Samuelsson M, et al. Low IL-8 is associated with anxiety in suicidal patients: genetic variation and decreased protein levels. Acta Psychiatr Scand. 2015;131:269–78.
Johansson V, Nybom R, Wetterberg L, Hultman CM, Cannon TD, Johansson AG, et al. Microscopic particles in two fractions of fresh cerebrospinal fluid in twins with schizophrenia or bipolar disorder and in healthy controls. PLoS One. 2012;7:e45994.
Johansson V, Jakobsson J, Fortgang R, Zetterberg H, Blennow K, Cannon T, et al. Cerebrospinal fluid microglia and neurodegenerative markers in twins concordant and discordant for psychotic disorders. Eur Arch Psychiatry Clin Neurosci. 2017;267:391–402.
Johansson V, Erhardt S, Engberg G, Kegel M, Bhat M, Schwieler L, et al. Twin study shows association between monocyte chemoattractant protein-1 and kynurenic acid in cerebrospinal fluid. Eur Arch Psychiatry Clin Neurosci. 2020 Oct 1 [cited 2021 Nov 9];270:933–8. Available from: https://link.springer.com/article/10.1007/s00406-019-01042-9.
Karlsson H, Holtze M, Engberg G, Thomann P, Schroder J. Structural brain correlates of HERV-W related RNA detected in cerebrospinal fluids from patients with first-episode schizophrenia spectrum disorder. Brain Behav Immun. 2010;24:S51–2.
Kegel M, Johansson V, Wetterberg L, Bhat M, Schwieler L, Cannon T, et al. Kynurenic acid and psychotic symptoms and personality traits in twins with psychiatric morbidity. Psychiatry Res. 2017;247:105–12.
Kim J, Kornhuber H, Schmid-Burgk W, Holzmüller B. Low cerebrospinal fluid glutamate in schizophrenic patients and a new hypothesis on schizophrenia. Neurosci Lett. 1980;20:379–82.
Kirch DG, Suddath RL, Gerhardt GA, Issa F, Freedman R, Wyatt RJ. Analysis of cerebrospinal-fluid monoamines in schizophrenic-patients on and off neuroleptic treatment and compared with healthy controls. Schizophr Res. 1991;4:349.
Koethe D, Gerth CW, Schreiber D, Nolden BM, Gross S, Juelicher A, et al. The endocannabinoid anandamide in CSF is related to the patterns of cannabis use in first-episode schizophrenia. Biol Psychiatry. 2005;57:186S–186S.
Lao A, Conde B, Reyes A. Analysis of lymphocytes and macrophages in the CSF of first onset and chronic schizophrenia. Int J Neuropsychopharmacol. 2004;7:S218–S218.
Leweke F, Gerth C, Koethe D, Klosterkötter J, Ruslanova I, Krivogorsky B, et al. Antibodies to infectious agents in individuals with recent onset schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2004;254:4–8.
Leweke F, Giuffrida A, Koethe D, Schreiber D, Nolden BM, Kranaster L, et al. Anandamide levels in cerebrospinal fluid of first-episode schizophrenic patients: impact of cannabis use. Schizophr Res. 2007;94:29–36.
Li S, Wu H, Guo H, Zhao Z. Neuron-specific Enolase and myelin basic protein in cerebrospinal fluid of patients with first episode schizophrenia. J Huazhong Univ Sci Technolog Med Sci. 2006;26:228–30.
Lindqvist D, Janelidze S, Hagell P, Erhardt S, Samuelsson M, Minthon L, et al. Interleukin-6 Is Elevated in the Cerebrospinal Fluid of Suicide Attempters and Related to Symptom Severity. Biol Psychiatry. 2009;66:287–92.
Lindström L, Nyberg F, Terenius L, Bauer K, Besev G, Gunne L, et al. CSF and plasma beta-casomorphin-like opioid peptides in postpartum psychosis. Am J Psychiatry. 1984;141:1059–66.
Lindström L, Ekman R, Walleus H, Widerlöv E. Delta-sleep inducing peptide in cerebrospinal fluid from schizophrenics, depressives and healthy volunteers. Prog Neuropsychopharmacol Biol Psychiatry. 1985;9:83–90.
Lindström L, Wieselgren I, Klockhoff I, Svedberg A. Relationship between abnormal brainstem auditory-evoked potentials and subnormal CSF levels of HVA and 5-HIAA in first-episode schizophrenic patients. Biol Psychiatry. 1990;28:435–42.
Malmqvist A, Schwieler L, Orhan F, Fatouros-Bergman H, Bauer M, Flyckt L, et al. Increased peripheral levels of TARC/CCL17 in first episode psychosis patients. Schizophr Res. 2019;210:221–7.
Mätlik K, Garton DR, Montaño-Rodríguez AR, Olfat S, Eren F, Casserly L, et al. Elevated endogenous GDNF induces altered dopamine signalling in mice and correlates with clinical severity in schizophrenia. Mol Psychiatry. 2022;27:3247–61.
Martins-de-Souza D, Maccarrone G, Schmitt A, Falkai P, Dias-Neto E, Gattaz W, et al. Proteome analyses of post-mortembrain tissue from patients with schizophrenia suggest dysfunction of oligodendrocytes and astrocytes and potential biomarker candidates? Schizophr Res. 2012;136:S61.
Mathé A, Apéria B, Bergman P, Eberhard G, Jerling M, Lindström L, et al. Metabolic products of arachidonic acid in the central nervous system: possible role in mental disorders. Adv Prostaglandin Thromboxane Leukot Res. 1987;17B:958–62.
Mathé A, Agren H, Lindström L, Theodorsson E. Increased concentration of calcitonin gene-related peptide in cerebrospinal fluid of depressed patients. A possible trait marker of major depressive disorder. Neurosci Lett. 1994;182:138–42.
McAllister CG, Konicki E, Kirch DG, Rapaport MH, Paul SM, Pickar D. Increased percentages of lymphocytes-t in the csf of schizophrenic-patients. Schizophr Res. 1991;4:373.
McKenna T, Hughes CJ, Huang JT, Chan MK, Bahn S, Langridge JI. Proteomic profiling of cerebrospinal fluid and serum in schizophrenia using a label free mass spectrometric approach. Clin Chem. 2007;53:A70–A70.
Miller CH, Kirchmair R, Saria A, Fleischhacker WW, Winkler H. Concentrations of secretoneurin and chromogranin-a immunoreactivities in the cerebrospinal-fluid of schizophrenic-patients. Schizophr Res. 1995;15:67–8.
Mizui T, Hattori K, Ishiwata S, Hidese S, Yoshida S, Kunugi H, et al. Cerebrospinal fluid BDNF pro-peptide levels in major depressive disorder and schizophrenia. J Psychiatr Res. 2019;113:190–8.
Naber D, Pickar D, Post P, Van Kammen D, Waters R, Ballenger J, et al. Endogenous opioid activity and beta-endorphin immunoreactivity in CSF of psychiatric patients and normal volunteers. Am J Psychiatry. 1981;138:1457–62.
Nasrallah HA, Meng-Yang Z, Garver DL. Apoptotic markers in schizophrenia: Elevated CSF levels of bcl-2 in antipsychotic responders but not non-responders. Biol Psychiatry. 2003;53:109S–109S.
Nasrallah HA, Zhu MY, Garver DL. A controlled study of CSF levels of caspases 1, 3, 8 and 9 in schizophrenia: Evidence of apoptotic overexpression. Neuropsychopharmacology. 2004;29:S158–S158.
Nasrallah HA. A controlled study of CSF levels of caspases 1,3,8 and 9 in schizophrenia: Evidence of apoptotic overexpression. Schizophr Bull. 2005;31:291.
Nemeroff C, Widerlöv E, Bissette G, Walléus H, Karlsson I, Eklund K, et al. Elevated concentrations of CSF corticotropin-releasing factor-like immunoreactivity in depressed patients. Science. 1984;226:1342–4.
Nemeroff C, Bissette G, Widerlov E, Beckmann H, Gerner R, Manberg PJ, et al. Neurotensin-like immunoreactivity in cerebrospinal fluid of patients with schizophrenia, depression, anorexia nervosa-bulimia, and premenstrual syndrome. J Neuropsychiatry Clin Neurosci. 1989;1:16–20.
Niwa M, Hayes, Tanaka T, Faust T, Fukudome D, Cash-Padgett T, et al. Oxidative stress in the pathophysiology of psychiatric disorders: Studies of patient biospecimens and animal models. Neuropsychopharmacology. 2015;40:S228–9.
Ohlund L, Lindstrom L, Ohman A. Electrodermal orienting response and central nervous system dopamine and serotinin activity in schizophrenia. J Nerv Ment Dis. 1992;180:304–13.
Oleszak EL, Lin WL, Chang JR, Zhang X, Bhattacharjee M, Rudner G, et al. Cerebrospinal fluid (CSF) from patients with schizophrenia or affective disorders contain oligoclonal populations of T cells. J Neuroimmunol. 2004;154:138.
Omori W, Hattori K, Kajitani N, Okada-Tsuchioka M, Boku S, Kunugi H, et al. Increased matrix metalloproteinases in cerebrospinal fluids of patients with major depressive disorder and schizophrenia. Int J Neuropsychopharmacol. 2020;23:713–20.
Orhan F, Fatouros-Bergman H, Goiny M, Malmqvist A, Piehl F, Cervenka S, et al. CSF GABA is reduced in first-episode psychosis and associates to symptom severity. Mol Psychiatry. 2018;23:1244–50.
Oxenstierna G, Bergstrand G, Edman G, Flyckt L, Nybäck H, Sedvall G. Increased frequency of aberrant CSF circulation in schizophrenic patients compared to healthy volunteers. Eur Psychiatry. 1996;11:16–20.
Pickar D, Naber D, Post RM, van Kammen DP, Ballenger J, Kalin N, et al. Measurement of endorphins in CSF. Relationship to psychiatric diagnosis. Mod Probl Pharmacopsychiatry. 1981;17:246–62.
Pillai A, Kale A, Joshi S, Naphade N, Raju MSVK, Nasrallah H, et al. Decreased BDNF levels in CSF of drug-naive first-episode psychotic subjects: correlation with plasma BDNF and psychopathology. Int J Neuropsychopharmacol. 2010;13:535–9.
Poltorak M, Khoja I, Hemperly JJ, Williams J, Elmallakh R, Freed WJ. Disturbances in cell recognition molecules (L1 and N-CAM) in the csf of patients with schizophrenia. Neurology. 1994;44:A377–A377.
Poltorak M, Wright R, Hemperly JJ, Torrey EF, Issa F, Wyatt RJ, et al. Monozygotic twins discordant for schizophrenia are discordant for N-CAM and L1 in CSF. Brain Res. 1997;751:152–4.
Post R, Fink E, Carpenter WT Jr, Goodwin F. Cerebrospinal fluid amine metabolites in acute schizophrenia. Arch Gen Psychiatry. 1975;32:1063–9.
Prell G, Green J, Kaufmann C, Khandelwal JK, Morrishow AM, Kirch DG, et al. Histamine metabolites in cerebrospinal fluid of patients with chronic schizophrenia: their relationships to levels of other aminergic transmitters and ratings of symptoms. Schizophr Res. 1995;14:93–104.
Raedler TJ, Wittke S, Mischak H, Jahn H, Wiedemann K. Disease-specific polypeptide-patterns in CSF in schizophrenia and Alzheimer disease. Schizophr Bull. 2005;31:292.
Regenold W, Phatak P, Marano C, Sassan A, Conley R, Kling M. Elevated cerebrospinal fluid lactate concentrations in patients with bipolar disorder and schizophrenia: implications for the mitochondrial dysfunction hypothesis. Biol Psychiatry. 2009;65:489–94.
Ringo D, Lindley S, Faull K, Faustman W. Cholesterol and serotonin: seeking a possible link between blood cholesterol and CSF 5-HIAA. Biol Psychiatry. 1994;35:957–9.
Ramaekers V, Thöny B, Sequeira J, Ansseau M, Philippe P, Boemer F, et al. Folinic acid treatment for schizophrenia associated with folate receptor autoantibodies. Mol Genet Metab. 2014;113:307–14.
Sasayama D, Hattori K, Teraishi T, Hori H, Ota M, Yoshida S, et al. Negative correlation between cerebrospinal fluid oxytocin levels and negative symptoms of male patients with schizophrenia. Schizophr Res. 2012;139:201–6.
Sato Y, Suzuki I, Nakamura T, Bernier F, Aoshima K, Oda Y. Investigation of new AD plasma biomarker and its possibility. Neurodegener Dis. 2011;8;(Suppl. 1, 13).
Skinner A, Mahadik S, Garver D. Thiobarbituric acid reactive substances in the cerebrospinal fluid in schizophrenia. Schizophr Res. 2005;76:83–7.
Stanta J, Saldova R, Struwe W, Byrne J, Leweke F, Rothermund M, et al. Identification of N-glycosylation changes in the CSF and serum in patients with schizophrenia. J Proteome Res. 2010;9:4476–89.
Söderlund J, Schröder J, Nordin C, Mamuelsson M, Walther-Jallow L, Karlsson H, et al. Activation of brain MPopen interleukin-1β in schizophrenia. Mol Psychiatry. 2009;14:1069–71.
Torrey EF, Yolken RH, Zito M, Heyes M. Increased CSF and brain quinolinic acid in schizophrenia and bipolar disorder. Schizophr Res. 1998;29:91–2.
Uete T, Nishimura S, Oya H, Shimomura T, Tatebayashi Y. Corticosteroid levels in blood and cerebrospinal fluid in various diseases. J Clin Endocrinol Metab. 1970;30:208–14.
van Kammen D, Kelley, Yao J, Gilbertson M, Gurklis J, Inosaka T, et al. Predicting haloperidol treatment response in chronic schizophrenia. Psychiatry Res. 1996;64:47–58.
van Praag H. CSF 5-HIAA and suicide in non-depressed schizophrenics. Lancet. 1983;2:977–8.
Vawter M, Hemperly J, Freed W, Garver D. CSF N-CAM in neuroleptic-naïve first-episode patients with schizophrenia. Schizophr Res. 1998;34:123–31.
Vawter M, Frye M, Hemperly J, VanderPutten D, Usen N, Doherty P, et al. Elevated concentration of N-CAM VASE isoforms in schizophrenia. J Psychiatr Res. 2000;34:25–34.
Wieselgren I, Lindström L. CSF levels of HVA and 5-HIAA in drug-free schizophrenic patients and healthy controls: a prospective study focused on their predictive value for outcome in schizophrenia. Psychiatry Res. 1998;81:101–10.
Yao JK, van Kammen DP, Peters JL, Gurklis JA. CSF serine levels in schizophrenia. J Neurochem. 2001;78:158.
Anderson G, Gerner R, Cohen D, Fairbanks L. Central tryptamine turnover in depression, schizophrenia, and anorexia: measurement of indoleacetic acid in cerebrospinal fluid. Biol Psychiatry. 1984;19:1427–35.
Andreou D, Söderman E, Axelsson T, Sedvall GC, Terenius L, Agartz I, et al. Polymorphisms in genes implicated in dopamine, serotonin and noradrenalin metabolism suggest association with cerebrospinal fluid monoamine metabolite concentrations in psychosis. Behav Brain Funct. 2014;10:26.
Barbaccia M, Costa E, Ferrero P, Guidotti A, Roy A, Sunderland T, et al. Diazepam-binding inhibitor. A brain neuropeptide present in human spinal fluid: studies in depression, schizophrenia, and Alzheimer’s disease. Arch Gen Psychiatry. 1986;43:1143–7.
Beck O, Borg S, Edman G, Fyrö B, Oxenstierna G, Sedvall G. 5-hydroxytryptophol in human cerebrospinal fluid: conjugation, concentration gradient, relationship to 5-hydroxyindoleacetic acid, and influence of hereditary factors. J Neurochem. 1984;43:58–61.
Beinfeld B, Garver D. Concentration of cholecystokinin in cerebrospinal fluid is decreased in psychosis: relationship to symptoms and drug response. Prog Neuropsychopharmacol Biol Psychiatry. 1991;15:601–9.
Bendikov I, Nadri C, Amar S, Panizzutti R, De Miranda J, Wolosker H, et al. A CSF and postmortem brain study of D-serine metabolic parameters in schizophrenia. Schizophr Res. 2007;90:41–51.
Berger P, Faull K, Kilkowski J, Anderson P, Kraemer H, Davis K, et al. CSF monoamine metabolites in depression and schizophrenia. Am J Psychiatry. 1980;137:174–80.
Berrettini W, Doran A, Kelsoe J, Roy A, Pickar D. Cerebrospinal fluid neuropeptide Y in depression and schizophrenia. Neuropsychopharmacology. 1987;1:81–3.
Peters J, Van Kammen D, Gelernter J, Yao J, Shaw D. Neuropeptide Y-like immunoreactivity in schizophrenia. Relationships with clinical measures. Schizophr Res. 1990;3:287–94.
Beuger M, Van Kammen DP, Kelley ME, Yao J. Dopamine turnover in schizophrenia before and after haloperidol withdrawal: CSF, plasma, and urine studies. Neuropsychopharmacology. 1996;15:75–86.
Bissette G, Widerlöv E, Walléus H, Karlsson I, Eklund K, Forsman A, et al. Alterations in cerebrospinal fluid concentrations of somatostatinlike immunoreactivity in neuropsychiatric disorders. Arch Gen Psychiatry. 1986;43:1148–51.
Bowers M Jr. 5-Hydroxyindoleacetic acid (5HIAA) and homovanillic acid (HVA) following probenecid in acute psychotic patients treated with phenothiazines. Psychopharmacologia. 1973;28:309–18.
Breier A, Wolkowitz OM, Doran AR, Bellar S, Pickar D. Neurobiological effects of lumbar puncture stress in psychiatric patients and healthy volunteers. Psychiatry Res. 1988;25:187–94.
Breslin N, Suddath R, Bissette G, Nemeroff C, Lowrimore P, Weinberger D. CSF concentrations of neurotensin in schizophrenia: an investigation of clinical and biochemical correlates. Schizophr Res. 1994;12:35–41.
Catlin DH, Gorelick DA, Gerner RH. Clinical pharmacology of β‐endorphin in depression and schizophrenia. Ann N Y Acad Sci. 1982;398:434–47.
Comasco E, Vumma R, Toffoletto S, Johansson J, Flyckt L, Lewander T, et al. Genetic and functional study of L-type amino acid transporter 1 in schizophrenia. Neuropsychobiology. 2016;74:96–103.
Coughlin J, Ishizuka K, Kano S, Edwards J, Seifuddin F, Shimano M, et al. Marked reduction of soluble superoxide dismutase-1 (SOD1) in cerebrospinal fluid of patients with recent-onset schizophrenia. Mol Psychiatry. 2013;18:10–1.
Coughlin JM, Wang Y, Ambinder EB, Ward RE, Minn I, Vranesic M, et al. In vivo Markers of inflammatory response in recent-onset schizophrenia: a combined study using [11 C]DPA-713 PET and analysis of CSF and plasma. Transl Psychiatry. 2016;6:1–8.
Csernansky J, King R, Faustman W, Moses JA Jr, Poscher M, Faull K. 5-HIAA in cerebrospinal fluid and deficit schizophrenic characteristics. Br J Psychiatry. 1990;156:501–7.
Deutsch S, Mohs R, Levy M, Rothpearl A, Stockton D, Horvath T, et al. Acetylcholinesterase activity in CSF in schizophrenia, depression, Alzheimer’s disease and normals. Biol Psychiatry. 1983;18:1363–73.
Egan M, El-Mallakh R, Suddath R, Lohr J, Bracha H, Wyatt R. Cerebrospinal fluid and serum levels of neuron-specific enolase in patients with schizophrenia. Psychiatry Res. 1992;43:187–95.
El-Mallakh RS, Suddath RL, Wyatt RJ. Interleukin-1!a and interleukin-2 in cerebrospinal fluid of schizophrenic subjects. Prog Neuropsychopharmacol Biol Psychiatry. 1993;17:383–91.
Erhardt S, Blennow K, Nordin C, Skogh E, Lindström L, Engberg G. Kynurenic acid levels are elevated in the cerebrospinal fluid of patients with schizophrenia. Neurosci Lett. 2001;313:96–8.
Faustman W, Elliott R, Ringo D, Faull K. CSF 5-HIAA and atmospheric pressure: failure to replicate. Biol Psychiatry. 1993;33:61–3.
Gallego JA, Blanco EA, Morell C, Lencz T, Malhotra AK. Complement component C4 levels in the cerebrospinal fluid and plasma of patients with schizophrenia. Neuropsychopharmacology. 2020;46:1140–4.
Garbutt J, van Kammen D, Levine R, Sternberg D, Murphy D, Ballenger J, et al. Cerebrospinal fluid hydroxylase cofactor in schizophrenia. Psychiatry Res. 1982;6:145–51.
Garver D, Beinfeld M, Yao J. Cholecystokinin, dopamine and schizophrenia. Psychopharmacol Bull. 1990;26:377–80.
Garver D, Bissette G, Yao J, Nemeroff C. Relation of CSF neurotensin concentrations to symptoms and drug response of psychotic patients. Am J Psychiatry. 1991;148:484–8.
Garver DL, Tamas RL, Holcomb JA. Elevated lnterleukin-6 in the Cerebrospinal Fluid of a Previously Delineated Schizophrenia Subtype. Neuropsychopharmacology. 2003;28:1515–20.
Gerner R, Hare T. CSF GABA in normal subjects and patients with depression, schizophrenia, mania, and anorexia nervosa. Am J Psychiatry. 1981;138:1098–101.
Gerner R, Sharp B. CSF beta-endorphin-immunoreactivity in normal, schizophrenic, depressed, manic and anorexic subjects. Brain Res. 1982;237:244–7.
Gerner R, Merrill J. Cerebrospinal fluid prostaglandin E in depression, mania, and schizophrenia compared to normals. Biol Psychiatry. 1983;18:565–9.
Gerner R, Fairbanks L, Anderson G, Young J, Scheinin M, Linnoila M, et al. CSF neurochemistry in depressed, manic, and schizophrenic patients compared with that of normal controls. Am J Psychiatry. 1984;141:1533–40.
Gerner R, van Kammen D, Ninan R. Cerebrospinal fluid cholecystokinin, bombesin and somatostatin in schizophrenia and normals. Prog Neuropsychopharmacol Biol Psychiatry. 1985;9:73–82.
Giuffrida A, Leweke F, Gerth C, Schreiber D, Koethe D, Faulhaber J, et al. Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms. Neuropsychopharmacology. 2004;29:2108–14.
Glovinsky D, Kalogeras K, Kirch D, Suddath R, Wyatt R. Cerebrospinal fluid oxytocin concentration in schizophrenic patients does not differ from control subjects and is not changed by neuroleptic medication. Schizophr Res. 1994;11:273–6.
Gotoh L, Yamada M, Hattori K, Sasayama D, Noda T, Yoshida S, et al. Levels of lysophosphatidic acid in cerebrospinal fluid and plasma of patients with schizophrenia. Psychiatry Res. 2019;273:331–5.
Gottfries C, Gottfries I, Johansson B, Olsson R, Persson T, Roos B, et al. Acid monoamine metabolites in human cerebrospinal fluid and their relations to age and sex. Neuropharmacology. 1971;10:665–72.
Gracias J, Orhan F, Hörbeck E, Holmén-Larsson J, Khanlarkani N, Malwade S, et al. Cerebrospinal fluid concentration of complement component 4 A is increased in first episode schizophrenia. Nat Commun. 2022;13:6427.
Harrington M, Merril C, Torrey E. Differences in cerebrospinal fluid proteins between patients with schizophrenia and normal persons. Clin Chem. 1985;31:722–6.
Hashimoto K, Engberg G, Shimizu E, Nordin C, Lindström LH, Iyo M. Reduced D-serine to total serine ratio in the cerebrospinal fluid of drug naive schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:767–9.
Hashimoto K, Engberg G, Shimizu E, Nordin C, Lindström LH, Iyo M. Elevated glutamine/glutamate ratio in cerebrospinal fluid of first episode and drug naive schizophrenic patients. BMC Psychiatry. 2005;5:6.
Hattori K, Sasayama D, Teraishi T, Fujii T. Analyses of monoamine metabolites in the cerebrospinal fluid of patients with schizophrenia. Schizophr Res. 2012;136:S137.
Hidese S, Hattori K, Sasayama D, Tsumagari T, Miyakawa T, Matsumura R, et al. Cerebrospinal fluid neuroplasticity-associated protein levels in patients with psychiatric disorders: a multiplex immunoassay study. Transl Psychiatry. 2020;10:161.
Hidese S, Hattori K, Sasayama D, Tsumagari T, Miyakawa T, Matsumura R, et al. Cerebrospinal fluid inflammatory cytokine levels in patients with major psychiatric disorders: a multiplex immunoassay study. Front Pharmacol. 2021;11:594394.
Hsiao J, Colison J, Bartko JJ, Doran A, Konicki PE, Potter WZ, et al. Monoamine neurotransmitter interactions in drug-free and neuroleptic-treated schizophrenics. Arch Gen Psychiatry. 1993;50:606–14.
Husain-Krautter S, Lee J, Vos D, Gallego JA, Malhotra AK, Rothstein TL. Skewing of the antibody repertoire in cerebrospinal fluid B cells from healthy controls and patients with schizophrenia. Behav Brain Res. 2022;422:113743.
Iadarola J, Flores C, Cadet J, Suddath R, Illowsky B, Berman K. Met5-enkephalin-Arg6-Gly7-Leu8 immunoreactivity in rat and human cerebrospinal fluid: influence of neuroleptic drugs and electroconvulsive shock. Brain Res. 1988;474:75–85.
Ishii T, Hattori K, Miyakawa T, Watanabe K, Hidese S, Sasayama D, et al. Increased cerebrospinal fluid complement C5 levels in major depressive disorder and schizophrenia. Biochem Biophys Res Commun. 2018;497:683–8.
Issa F, Gerhardt GA, Bartko JJ, Suddath RL, Lynch M, Gamache PH, et al. A multidimensional approach to analysis of cerebrospinal-fluid biogenic-amines in schizophrenia .1. Comparisons with healthy control subjects and neuroleptic-treated/unmedicated pairs analyses. Psychiatry Res. 1994;52:237–49.
Jeppesen R, Orlovska-Waast S, Sørensen NV, Christensen RH, Benros ME. Cerebrospinal fluid and blood biomarkers of neuroinflammation and blood-brain barrier in psychotic disorders and individually matched healthy controls. Schizophr Bull. 2022;48:1206–16.
Kale A, Joshi S, Naphade N, Sapkale S, Raju MSVK, Pillai A, et al. Opposite changes in predominantly docosahexaenoic acid (DHA) in cerebrospinal fluid and red blood cells from never-medicated first-episode psychotic patients. Schizophr Res. 2008;98:295–301.
Kale A, Joshi S, Pillai A, Naphade N, Raju MSVK, Nasrallah H, et al. Reduced cerebrospinal fluid and plasma nerve growth factor in drug-naïve psychotic patients. Schizophr Res. 2009;115:209–14.
Katila G, Hurme M, Wahlbeck K, Appelberg B, Rimón R. Plasma and cerebrospinal fluid lnterleukin-1ß and lnterleukin-6 in hospitalized schizophrenic patients. Neuropsychobiology. 1994;30:20–3.
Kegel M, Bhat M, Skogh E, Samuelsson M, Lundberg K, Dahl M, et al. Imbalanced kynurenine pathway in schizophrenia. Int J Tryptophan Res. 2014;7:15–22.
Kirch D, Alexander R, Suddath R, Papadopoulos N, Kaufmann C, Daniel D, et al. Blood-CSF barrier permeability and central nervous system immunoglobulin G in schizophrenia. J Neural Transm Gen Sect. 1992;89:219–32.
Koponen H, Riekkinen P. Cerebrospinal fluid acetylcholinesterase in patients with dementia associated with schizophrenia or chronic alcoholism. Acta Psychiatr Scand. 1991;83:441–3.
Koponen H, Riekkinen PJ. Cerebrospinal fluid beta-endorphin-like immunoreactivity in patients with dementia associated with schizophrenia and chronic alcoholism. Nordisk Psykiatrisk Tidsskrift. 1991;45:309–11.
Lake C, Sternberg D, van Kammen D, Ballenger J, Ziegler M, Post R, et al. Schizophrenia: elevated cerebrospinal fluid norepinephrine. Science. 1980;207:331–3.
Landén M, Grenfeldt B, Davidsson P, Stridsberg M, Regland B, Gottfries CG, et al. Reduction of chromogranin A and B but not C in the cerebrospinal fluid in subjects with schizophrenia. Eur Neuropsychopharmacol. 1999;9:311–5.
Levine J, Agam G, Sela BA, Garver DL, Torrey EF, Belmaker RH. CSF homocysteine is not elevated in schizophrenia. J Neural Transm (Vienna). 2005;112:297–302.
Lewine R, Risch S, Risby E, Stipetic M, Jewart R, Eccard M, et al. Lateral ventricle-brain ratio and balance between CSF HVA and 5-HIAA in schizophrenia. Am J Psychiatry. 1991;148:1189–94.
Licinio J, Seibyl J, Altemus M, Charney D, Krystal J. Elevated CSF levels of interleukin-2 in neuroleptic-free schizophrenic patients. Am J Psychiatry. 1993;150:1408–10.
Lindström L, Widerlöv E, Gunne L, Wahlström A, Terenius L. Endorphins in human cerebrospinal fluid: clinical correlations to some psychotic states. Acta Psychiatr Scand. 1978;57:153–64.
Lindström L, Besev G, Gunne L, Terenius L. CSF levels of receptor-active endorphins in schizophrenic patients: correlations with symptomatology and monoamine metabolites. Psychiatry Res. 1986;19:93–100.
Lindström L, Widerlöv E, Bisette G, Nemeroff C. Reduced CSF neurotensin concentration in drug-free schizophrenic patients. Schizophr Res. 1988;1:55–9.
Lotstra F, Verbanck P. Reduced cholecystokinin levels in cerebrospinal fluid of Parkinsonian and schizophrenic patients. Effect of ceruletide in schizophrenia. Ann N Y Acad Sci. 1985;448:507–17.
Mathé A, Sedvall G, Wiesel F, Nybäck H. Increased content of immunoreactive prostaglandin E in cerebrospinal fluid of patients with schizophrenia. Lancet. 1980;1:16–8.
Maas JW, Contreras SA, Miller AL, Bennan N, Bowden CL, Javors MA, et al. Studies of catecholamine metabolism in schizophrenia/psychosis-I. Neuropsychopharmacology. 1993;8:97–109.
Maas J, Bowden C, Miller A, Javors M, Funderburg L, Berman N, et al. Schizophrenia, psychosis, and cerebral spinal fluid homovanillic acid concentrations. Schizophr Bull. 1997;23:147–54.
Nakao K, Oki S, Tanaka I, Horii K, Nakai Y, Furui T, et al. Immunoreactive beta-endorphin and adrenocorticotropin in human cerebrospinal fluid. J Clin Invest. 1980;66:1383–90.
Nikkilä HV, Ahokas A, Wahlbeck K, Rimón R, Andersson LC. Neopterin and macrophage inflammatory protein-1α in the cerebrospinal fluid of schizophrenic patients: No evidence of intrathecal inflammation. Neuropsychobiology. 2002;46:169–72.
Nilsson L, Linderholm K, Engberg G, Paulson L, Blennow K, Lindström L, et al. Elevated levels of kynurenic acid in the cerebrospinal fluid of male patients with schizophrenia. Schizophr Res. 2005;80:315–22.
Nilsson-Todd LK, Nordin C, Jönsson EG, Skogh E, Erhardt S. Cerebrospinal fluid kynurenic acid in male patients with schizophrenia – correlation with monoamine metabolites. Acta Neuropsychiatr. 2007;19:45–52.
Härnryd C, Bjerkenstedt L, Björk K, Gullberg B, Oxenstierna G, Sedvall G, et al. Clinical evaluation of sulpiride in schizophrenic patients-a double-blind comparison with chlorpromazine. Acta Psychiatr Scand Suppl. 1984;311:7–30.
Oxenstierna G, Bergstrand G, Bjerkenstedt L, Sedvall G, Wik G. Evidence of disturbed CSF circulation and brain atrophy in cases of schizophrenic psychosis. Br J Psychiatry J Ment Sci. 1984;144:654–61.
Nishino S, Mignot E, Benson KL, Zarcone VP Jr. Cerebrospinal fluid prostaglandins and corticotropin releasing factor in schizophrenics and controls: relationship to sleep architecture. Psychiatry Res. 1998;78:141–50.
Nishino S, Ripley B, Mignot E, Benson KL, Zarcone VP. CSF hypocretin-1 levels in schizophrenics and controls: relationship to sleep architecture. Psychiatry Res. 2002;110:1–7.
Nybäck H, Berggren B, Hindmarsh T, Sedvall G, Wiesel FA. Cerebroventricular size and cerebrospinal fluid monoamine metabolites in schizophrenic patients and healthy volunteers. Psychiatry Res. 1983;9:301–8.
Orhan F, Schwieler L, Fatouros-Bergman H, Malmqvist A, Cervenka S, Collste K, et al. Increased number of monocytes and plasma levels of MCP-1 and YKL-40 in first-episode psychosis. Acta Psychiatr Scand. 2018;138:432–40.
Pandey S, Devpura J, Bedi H, Babel C. An estimation of magnesium and calcium in serum and C.S.F. in schizophrenia. J Assoc Physicians India. 1973;21:203–5.
Pickar D, Naber D, Post RM, Kammen DP, Kaye W, Rubinow DR, et al. Endorphins in the cerebrospinal fluid of psychiatric patients. Ann N Y Acad Sci. 1982;398:399–412.
Pickar D, Breier A, Hsiao JK, Doran AR, Wolkowitz OM, Pato CN, et al. Cerebrospinal fluid and plasma monoamine metabolites and their relation to psychosis: implications for regional brain dysfunction in schizophrenia. Arch Gen Psychiatry. 1990;47:641–8.
Potkin S, Shore D, Torrey E, Weinberger D, Gillin J, Henkin R, et al. Cerebrospinal fluid zinc concentrations in ex-heroin addicts and patients with schizophrenia: some preliminary observations. Biol Psychiatry. 1982;17:1315–22.
Prell GD, Green JP, Kaufmann CA, Khandelwal JK, Morrishow AM, Kirch DG, et al. Histamine metabolites in cerebrospinal-fluid of patients with chronic-schizophrenia - their relationships to levels of other aminergic transmitters and ratings of symptoms, (VOL 14, PG 93, 1995). Schizophr Res. 1995;14:268.
Rapaport M, McAllister C, Pickar D, Tamarkin L, Kirch D, Paul S. CSF IL-1 and IL-2 in medicated schizophrenic patients and normal volunteers. Schizophr Res. 1997;25:123–9.
Reinikainen K, Koponen H, Jolkkonen J, Riekkinen P. Decreased somatostatin-like immunoreactivity in the cerebrospinal fluid of chronic schizophrenic patients with cognitive impairment. Psychiatry Res. 1990;33:307–12.
Reuter A, Bumb, Mueller J, Rohleder C, Pahlisch F, Hanke F, et al. Association of anandamide with altered binocular depth inversion illusion in schizophrenia. World J Biol Psychiatry. 2017;18:483–8.
Risby E, Jewart R, Lewine R, Risch S, Stipetic M, McDaniel J, et al. An association between increased concentrations of cerebrospinal fluid dopamine sulfate and higher negative symptom scores in patients with schizophrenia and schizoaffective disorder. Biol Psychiatry. 1993;34:661–4.
Risch S, Lewine R, Kalin N, Jewart R, Risby E, Caudle J, et al. Limbic-hypothalamic-pituitary-adrenal axis activity and ventricular-to-brain ratio studies in affective illness and schizophrenia. Neuropsychopharmacology. 1992;6:95–100.
Roos R, Davis K, Meltzer H. Immunoglobulin studies in patients with psychiatric diseases. Arch Gen Psychiatry. 1985;42:124–8.
Rubinow DR. Cerebrospinal fluid somatostatin and psychiatric illness. Biol Psychiatry. 1986;21:341–65.
Saito T, Ishizawa H, Tsuchiya F, Ozawa H, Takahata N. Neurochemical findings in the cerebrospinal fluid of schizophrenic patients with tardive dyskinesia and neuroleptic-induced parkinsonism. Jpn J Psychiatry Neurol. 1986;40:189–94.
Samuelsson M, Skogh E, Lundberg K, Vrethem M, Öllinger K. Taurine and glutathione in plasma and cerebrospinal fluid in olanzapine treated patients with schizophrenia. Psychiatry Res. 2013;210:819–24.
Santillo A, Lundgren S, Xu C, Orhan F, Fatouros-Bergman H, Blennow K, et al. Neurogranin as a potential synaptic marker in the cerebrospinal fluid of patients with a first episode psychosis. Schizophr Res. 2019;208:490–2.
Sasayama D, Hattori K, Wakabayashi C, Teraishi T, Hori H, Ota M, et al. Increased cerebrospinal fluid interleukin-6 levels in patients with schizophrenia and those with major depressive disorder. J Psychiatr Res. 2013;47:401–6.
Schultz K, Träskman-Bendz L, Petersén Å. Transthyretin in cerebrospinal fluid from suicide attempters. J Affect Disord. 2008;109:205–8.
Schwieler L, Larsson M, Skogh E, Kegel M, Orhan F, Abdelmoaty S, et al. Increased levels of IL-6 in the cerebrospinal fluid of patients with chronic schizophrenia-significance for activation of the kynurenine pathway. J Psychiatry Neurosci. 2015;40:126–33.
Seppala T, Scheinin M, Capone A, Linnoila M. Liquid chromatographic assay for CSF catecholamines using electrochemical detection. Acta Pharmacol Toxicol (Copenh). 1984;55:81–7.
Severance E, Gressitt K, Alaedini A, Rohleder C, Enning F, Bumb J, et al. IgG dynamics of dietary antigens point to cerebrospinal fluid barrier or flow dysfunction in first-episode schizophrenia. Brain Behav Immun. 2015;44:148–58.
Sharma R, Faull K, Javaid J, Davis J. Cerebrospinal fluid levels of phenylacetic acid in mental illness: behavioral associations and response to neuroleptic treatment. Acta Psychiatr Scand. 1995;91:293–8.
Shore D, Potkin S, Weinberger D, Torrey E, Henkin R, Agarwal R, et al. CSF copper concentrations in chronic schizophrenia. Am J Psychiatry. 1983;140:754–7.
Sierra-Honigmann A, Carbone K, Yolken R. Polymerase chain reaction (PCR) search for viral nucleic acid sequences in schizophrenia. Br J Psychiatry. 1995;166:55–60.
Spiegel D. Hypnotizability and CSF HVA levels among psychiatric patients. Biol Psychiatry. 1992;31:95–8.
Sternberg DE. The effect of pimozide on CSF norepinephrine in schizophrenia. Am J Psychiatry. 1981;138:1045–51.
Sternberg D, van Kammen D, Lerner P, Ballenger J, Marder S, Post R. CSF dopamine beta-hydroxylase in schizophrenia. Low activity associated with good prognosis and good response to neuroleptic treatment. Arch Gen Psychiatry. 1983;40:743–7.
Swahn C. Gas chromatographic-mass spectrometric determination of myo-inositol in human cerebrospinal fluid. J Neurochem. 1985;45:331–4.
Swahn C, Sedvall G. CSF creatinine in schizophrenia. Biol Psychiatry. 1988;23:586–94.
Swahn C. Determination of N-acetylaspartic acid in human cerebrospinal fluid by gas chromatography-mass spectrometry. J Neurochem. 1990;54:1584–8.
Tamminga C, Littman R, Alphs L, Chase T, Thaker G, Wagman A. Neuronal cholecystokinin and schizophrenia: pathogenic and therapeutic studies. Psychopharmacology (Berl). 1986;88:387–91.
Thompson P, Rosenberger C, Qualls C. CSF SNAP-25 in schizophrenia and bipolar illness. A pilot study. Neuropsychopharmacology. 1999;21:717–22.
Thompson P, Kelley M, Yao J, Tsai G, van Kammen D. Elevated cerebrospinal fluid SNAP-25 in schizophrenia. Biol Psychiatry. 2003;53:1132–7.
Tsai G, van Kammen DP, Chen S, Kelley ME, Grier A, Coyle JT. Glutamatergic neurotransmission involves structural and clinical deficits of schizophrenia. Biol Psychiatry. 1998;44:667–74.
Ueno Y, Aoki N, Yabuki T, Kuraishi F. Electrolyte metabolism in blood and cerebrospinal fluid in psychoses. Folia Psychiatr Neurol Jpn. 1961;15:304–26.
van Kammen D, Sternberg D, Hare T, Waters R, Bunney W Jr. CSF levels of gamma-aminobutyric acid in schizophrenia. Low values in recently ill patients. Arch Gen Psychiatry. 1982;39:91–7.
van Kammen D, O’Connor D, Neylan T, Mouton A, Gurklis J, Gilbertson M, et al. CSF chromogranin A-like immunoreactivity in schizophrenia: relationships with REM latency and slow wave sleep. Psychiatry Res. 1992;42:53–63.
Van Kammen DP, Kelley ME, Gilbertson MW, Gurklis J, O’Connor DT. CSF dopamine!b-hydroxylase in schizophrenia: Associations with premorbid functioning and brain computerized tomography scan measures. Am J Psychiatry. 1994;151:372–8.
van Kammen D, Poltorak M, Kelley M, Yao J, Gurklis J, Peters J, et al. Further studies of elevated cerebrospinal fluid neuronal cell adhesion molecule in schizophrenia. Biol Psychiatry. 1998;43:680–6.
Van Kammen DP, McAllister-Sistilli CG, Kelley ME, Gurklis JA, Yao JK. Elevated interleukin-6 in schizophrenia. Psychiatry Res. 1999;87:129–36.
Vawter MP, Dillon-Carter O, Issa F, Wyatt RJ, Freed WJ. Transforming growth factors β1 and β2 in the cerebrospinal fluid of chronic schizophrenic patients. Neuropsychopharmacology. 1997;16:83–7.
Verbanck P, Lotstra F, Gilles C, Linkowski P, Mendlewicz J, Vanderhaeghen J. Reduced cholecystokinin immunoreactivity in the cerebrospinal fluid of patients with psychiatric disorders. Life Sci. 1984;34:67–72.
Wahlbeck K, Rimón R, Fyhrquist F. Elevated angiotensin-converting enzyme (kininase II) in the cerebrospinal fluid of neuroleptic-treated schizophrenic patients. Schizophr Res. 1993;9:77–82.
Wahlbeck K, Ahokas A, Miettinen K, Nikkilä H, Rimón R. Higher cerebrospinal fluid angiotensin-converting enzyme levels in neuroleptic-treated than in drug-free patients with schizophrenia. Schizophr Bull. 1998;24:391–7.
Widerlöv E, Lindström LH, Besev G, Manberg PJ, Nemeroff CB, Breese GR, et al. Subnormal CSF levels of neurotensin in a subgroup of schizophrenic patients: normalization after neuroleptic treatment. Am J Psychiatry. 1982;139:1122–6.
Widerlöv E, Lindström, Wahlestedt C, Ekman R. Neuropeptide Y and peptide YY as possible cerebrospinal fluid markers for major depression and schizophrenia, respectively. J Psychiatr Res. 1988;22:69–79.
Wik G, Wiesel F. Regional brain glucose metabolism: correlations to biochemical measures and anxiety in patients with schizophrenia. Psychiatry Res. 1991;40:101–14.
Xu C, Sellgren C, Fatouros-Bergman H, Piehl F, Blennow K, Zetterberg H, et al. CSF levels of synaptosomal-associated protein 25 and synaptotagmin-1 in first-episode psychosis subjects. IBRO Rep. 2020;8:136–42.
Hornykiewicz O. Brain noradrenaline and schizophrenia. Prog Brain Res. 1986;65:29–39.
van Kammen DP, Kelley M. Dopamine and norepinephrine activity in schizophrenia. An intergrative perspective. Schizophr Res. 1991;4:173–91.
Brosda J, Jantschak F, Pertz HH. α2-Adrenoceptors are targets for antipsychotic drugs. Psychopharmacology. 2014;231:801–12.
Hertel P, Fagerquist MV, Svensson TH. Enhanced cortical dopamine output and antipsychotic-like effects of raclopride by α2 adrenoceptor blockade. Science (1979). 1999;286:105–7.
Breier A, Wolkowitz OM, Roy A, Potter WZ, Pickar D. Plasma norepinephrine in chronic schizophrenia. Am J Psychiatry. 1990;147:1467–70.
Klimek V, Rajkowska G, Luker SN, Dilley G, Meltzer HY, Overholser JC, et al. Brain noradrenergic receptors in major depression and schizophrenia. Neuropsychopharmacology. 1999;21:69–81.
Mäki-Marttunen V, Andreassen OA, Espeseth T. The role of norepinephrine in the pathophysiology of schizophrenia. Neuroscience and Biobehavioral Reviews. Vol. 118. Elsevier Ltd; 2020. p. 298–314.
Pollak TA, Drndarski S, Stone JM, David AS, McGuire P, Abbott NJ. The blood–brain barrier in psychosis. The Lancet Psychiatry. Vol. 5. Elsevier Ltd; 2018. p. 79–92.
Wu N, Zhang X, Ye L, Xu Q, Jin S, Wang Z, et al. A weak association of the CLDN5 locus with schizophrenia in Chinese case-control samples. Eur Psychiatry. 2009;24:1–1.
Schümberg K, Polyakova M, Steiner J, Schroeter ML. Serum S100B is related to illness duration and clinical symptoms in schizophrenia—a meta-regression analysis. Front Cell Neurosci. 2016;10:46.
Benros ME, Waltoft BL, Nordentoft M, Ostergaard SD, Eaton WW, Krogh J, et al. Autoimmune diseases and severe infections as risk factors for mood disorders a nationwide study. JAMA Psychiatry. 2013;70:812–20.
Garbers C, Heink S, Korn T, Rose-John S. Interleukin-6: designing specific therapeutics for a complex cytokine. Vol. 17. Nature Publishing Group; 2018.
Kopf M, Baumann H, Freer G, Freudenberg M, Lamers M, Kishimoto T, et al. Impaired immune and acute-phase responses in interleukin-6-deficient mice. Nature. 1994;368:339–42.
Weaver JD, Huang MH, Albert M, Harris T, Rowe JW, Seeman TE. Interleukin-6 and risk of cognitive decline: Macarthur studies of successful aging. Neurology. 2002;59:371–8.
Kossmann T, Stahel PF, Lenzlinger PM, Redl H, Dubs RW, Trentz O, et al. Interleukin-8 released into the cerebrospinal fluid after brain injury is associated with blood-brain barrier dysfunction and nerve growth factor production. J Cereb Blood Flow Metab. 1997;17:280–9.
Zhang XY, Zhou DF, Cao LY, Zhang PY, Wu GY, Shen YC. Changes in serum interleukin-2, −6, and −8 levels before and during treatment with risperidone and haloperidol: Relationship to outcome in schizophrenia. J Clin Psychiatry. 2004;65:940–7.
Schwarcz R, Bruno JP, Muchowski PJ, Wu HQ. Kynurenines in the mammalian brain: When physiology meets pathology. Nat Rev Neurosci. 2012;13:465–77.
Jolicoeur FB, Gagné MA, Rivest R, Drumheller A, St-Pierre S. Atypical neuroleptic-like behavioral effects of neurotensin. Brain Res Bull. 1993;32:487–91.
de Hert M, Schreurs V, Vancampfort D, van Winkel R. Metabolic syndrome in people with schizophrenia: a review. Vol. 8, World Psychiatry. Masson SpA; 2009 [cited 2021 Apr 28]. p. 15–22. Available from: https://doi.org/10.1002/j.2051-5545.2009.tb00199.x.
Katchan V, David P, Shoenfeld Y. Cannabinoids and autoimmune diseases: a systematic review. Autoimmun Rev [Internet]. 2016 Jun 1 [cited 2021 Nov 9];15:513–28. Available from: https://pubmed.ncbi.nlm.nih.gov/26876387/.
Lupica CR, Hu Y, Devinsky O, Hoffman AF. Cannabinoids as hippocampal network administrators. Neuropharmacology [Internet]. 2017 Sep 15 [cited 2021 Nov 9];124:25–37. Available from: https://pubmed.ncbi.nlm.nih.gov/28392266/.
Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: Version III - The final common pathway. Schizophrenia Bulletin. Vol. 35. Oxford University Press; 2009. p. 549–62.
Olney JW, Farber NB. Glutamate receptor dysfunction and schizophrenia. Archives of General Psychiatry. Vol. 52. American Medical Association; 1995. p. 998–1007.
Acknowledgements
The authors would like to thank Dr. Daniel P. Van Kammen, Dr. Göran Engberg, Dr. Sophie Erhardt, Dr. Viktoria Johansson, Dr. Craig Wheelock, Dr. Kärt Mätlik, Dr. Kotaro Hattori and Dr. Dhamidhu Eratne for providing data for the study and information specialist Susie Rimborg for assistance in the design of the search string. The project was funded by the Independent Research Fund Denmark (grant number 7025-00078B) and an unrestricted grant from the Lundbeck Foundation (R268-2016-3925). The sponsors had no role in the acquisition of the data, interpretation of the results, or the decision to publish the findings.
Author information
Authors and Affiliations
Contributions
MEB, TBR, and RJ conceived and designed the study. TBR and RJ performed screening, review and data extraction. RHBC conducted the statistical analysis. TBR drafted the manuscript. All authors contributed to the critical revision of the manuscript, approved the final version before submission and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rømer, T.B., Jeppesen, R., Christensen, R.H.B. et al. Biomarkers in the cerebrospinal fluid of patients with psychotic disorders compared to healthy controls: a systematic review and meta-analysis. Mol Psychiatry 28, 2277–2290 (2023). https://doi.org/10.1038/s41380-023-02059-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02059-2
This article is cited by
-
Association between psychiatric admissions in patients with schizophrenia and IL-6 plasma levels polygenic score
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
The common misconception of blood–brain barrier terminology in psychiatry and neurology
European Archives of Psychiatry and Clinical Neuroscience (2023)