Abstract
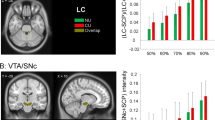
Previous studies both in laboratory animals and humans have reported that abstinence induces incubation of cue-induced drug craving for nicotine, alcohol, cocaine, and methamphetamine. However, current experimental procedures utilized to study incubation of methamphetamine craving do not incorporate the temporal dynamics of neuropsychological measures and electrophysiological activities associated with this incubation process. This study utilized the high-density electroencephalogram (EEG) signals as a rapid, inexpensive, and noninvasive measure of cue-induced craving potential. A total of 156 male individuals with methamphetamine use disorder (MUD) enrolled in this multisite, cross-sectional study. Structured clinical interview data, self-report questionnaires (cued craving, quality of sleep, impulsivity, anxiety, and depression) and resting-state, eye-closed 128 high-density channel EEG signals were collected at 5 abstinence duration time points (<1, 1–3, 3–6, 6–12, and 12–24 months) to track the neuropsychological and neurophysiological signatures. Cue-induced craving was higher after 1–3 months than after the other time points. This incubation effect was also observed for sleep quality but not for anxiety, depression, and impulsivity symptoms, along with exhibited decreased power spectrum for theta (5.5–8 Hz) and alpha (8–13 Hz), and increased in beta (16.5–26.5 Hz) frequency band. Source reconstructed resting-state EEG analysis showed increased synchronization of medial prefrontal cortex (MPFC) for the beta frequency band in 1–3 months abstinent MUD group, and associated with the incubation of craving. Remarkably, the robust incubation-related abnormalities may be driven by beta-band source space connectivity between MPFC and bilateral orbital gyrus (ORB). Our findings suggest the enhancement of beta activity in the incubation period most likely originates from a dysfunction involving frontal brain regions. This neurophysiological signature of incubation of craving can be used to identify individuals who might be most susceptible to relapse, providing a potential insight into future therapeutic interventions for MUD via neuromodulation of beta activity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data and materials availability
Original data are available upon request from corresponding author.
References
Office of China National Narcotics Control Commission. Drug situation in China. 2019. Retrieved from http://www.nncc626.com/2020-06/25/c_1210675877.htm. Accessed 20 June 2021.
Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Annu Rev Clin Psychol. 2007;3:257–84.
Sinha R. New findings on biological factors predicting addiction relapse vulnerability. Curr Psychiatry Rep. 2011;13:398–405.
Childress AR, Mozley PD, McElgin W, Fitzgerald J, Reivich M, O’Brien CP. Limbic activation during cue-induced cocaine craving. Am J Psychiatry. 1999;156:11–8.
Gawin FH, Kleber HD. Abstinence symptomatology and psychiatric diagnosis in cocaine abusers. Clin observations Arch Gen Psychiatry. 1986b;43:107–13.
Gawin FH, Kleber HD. Abstinence symptomatology and psychiatric diagnosis in cocaine abusers: clinical observations. Arch Gen Psychiatry. 1986a;43:107–13.
Grimm JW, Hope BT, Wise RA, Shaham Y. Neuroadaptation. Incubation of cocaine craving after withdrawal. Nature. 2001;412:141–2.
Pickens CL, Airavaara M, Theberge F, Fanous S, Hope BT, Shaham Y. Neurobiology of the incubation of drug craving. Trends Neurosci. 2011;34:411–20.
Venniro M, Caprioli D, Shaham Y. Animal models of drug relapse and craving: from drug priming-induced reinstatement to incubation of craving after voluntary abstinence. Prog Brain Res. 2016;224:25–52.
Wolf ME. Synaptic mechanisms underlying persistent cocaine craving. Nat Rev Neurosci. 2016;17:351–65.
Bedi G, Preston KL, Epstein DH, Heishman SJ, Marrone GF, Shaham Y, et al. Incubation of cue-induced cigarette craving during abstinence in human smokers. Biol Psychiatry. 2011;69:708–11.
Li P, Wu P, Xin X, Fan YL, Wang GB, Wang F, et al. Incubation of alcohol craving during abstinence in patients with alcohol dependence. Addict Biol. 2015;20:513–22.
Parvaz MA, Moeller SJ, Goldstein RZ. Incubation of cue-induced craving in adults addicted to cocaine measured by electroencephalography. JAMA Psychiatry. 2016;73:1127–34.
Wang G, Shi J, Chen N, Xu L, Li J, Li P, et al. Effects of length of abstinence on decision-making and craving in methamphetamine abusers. PloS ONE. 2013;8:e68791–91.
Altshuler RD, Lin H, Li X. Neural mechanisms underlying incubation of methamphetamine craving: a mini-review. Pharmacol Biochem Behav. 2020;199:173058.
Chen B, Wang Y, Liu X, Liu Z, Dong Y, Huang YH. Sleep regulates incubation of cocaine craving. J Neurosci. 2015;35:13300–10.
Franken IH, Dietvorst RC, Hesselmans M, Franzek EJ, van de Wetering BJ, Van Strien JW. Cocaine craving is associated with electrophysiological brain responses to cocaine-related stimuli. Addict Biol. 2008;13:386–92.
Marhe R, van de Wetering BJM, Franken IHA. Error-related brain activity predicts cocaine use after treatment at 3-month follow-up. Biol Psychiatry. 2013;73:782–8.
Brown DR, Jackson TCJ, Claus ED, Votaw VR, Stein ER, Robinson CSH, et al. Decreases in the late positive potential to alcohol images among alcohol treatment seekers following mindfulness-based relapse prevention. Alcohol Alcohol. 2019;55:78–85.
Andrew C, Fein G. Induced theta oscillations as biomarkers for alcoholism. Clin Neurophysiol. 2010;121:350–8.
Wang GY, Kydd R, Wouldes TA, Jensen M, Russell BR. Changes in resting EEG following methadone treatment in opiate addicts. Clin Neurophysiol. 2015;126:943–50.
Leyton M, Vezina P. Dopamine ups and downs in vulnerability to addictions: a neurodevelopmental model. Trends Pharmacol Sci. 2014;35:268–76.
Newton TF, Cook IA, Kalechstein AD, Duran S, Monroy F, Ling W, et al. Quantitative EEG abnormalities in recently abstinent methamphetamine dependent individuals. Clin Neurophysiol. 2003;114:410–5.
Newton TF, Kalechstein AD, Hardy DJ, Cook IA, Nestor L, Ling W, et al. Association between quantitative EEG and neurocognition in methamphetamine-dependent volunteers. Clin Neurophysiol. 2004;115:194–8.
Porjesz B, Rangaswamy M, Kamarajan C, Jones KA, Padmanabhapillai A, Begleiter H. The utility of neurophysiological markers in the study of alcoholism. Clin Neurophysiol. 2005;116:993–1018.
Rangaswamy M, Porjesz B, Chorlian DB, Wang K, Jones KA, Bauer LO, et al. Beta power in the EEG of alcoholics. Biol Psychiatry. 2002b;52:831–42.
Bauer LO. Predicting relapse to alcohol and drug abuse via quantitative electroencephalography. Neuropsychopharmacology. 2001;25:332–40.
Shen Y, Cao X, Tan T, Shan C, Wang Y, Pan J, et al. 10-Hz repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex reduces heroin cue craving in long-term addicts. Biol psychiatry. 2016;80:e13–4.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J consulting Clin Psychol. 1988;56:893.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Reise SP, Moore TM, Sabb FW, Brown AK, London ED. The Barratt Impulsiveness Scale–11: Reassessment of its structure in a community sample. Psychological Assess. 2013;25:631.
Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann. Stat. 2001;29:1165–88.
Imperatori LS, Betta M, Cecchetti L, Canales-Johnson A, Ricciardi E, Siclari F, et al. EEG functional connectivity metrics wPLI and wSMI account for distinct types of brain functional interactions. Sci Rep. 2019;9:8894.
Toll R, Wu W, Naparstek S, Zhang Y, Narayan M, Patenaude B, et al. An electroencephalography connectomic profile of post-traumatic stress disorder. Am J Psychiatry. 2020;177:233–43.
Angarita GA, Emadi N, Hodges S, Morgan PT. Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addict Sci Clin Pr. 2016;11:9–9.
Moallem NR, Courtney KE, Ray LA. The relationship between impulsivity and methamphetamine use severity in a community sample. Drug Alcohol Depend. 2018;187:1–7.
Zorick T, Nestor L, Miotto K, Sugar C, Hellemann G, Scanlon G, et al. Withdrawal symptoms in abstinent methamphetamine-dependent subjects. Addiction. 2010;105:1809–18.
Wang Y, Guo R, Chen B, Rahman T, Cai L, Li Y, et al. Cocaine-induced neural adaptations in the lateral hypothalamic melanin-concentrating hormone neurons and the role in regulating rapid eye movement sleep after withdrawal. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-00921-1.
Marissen MA, Franken IH, Waters AJ, Blanken P, Van Den Brink W, Hendriks VM. Attentional bias predicts heroin relapse following treatment. Addiction. 2006;101:1306–12.
Haifeng J, Wenxu Z, Hong C, Chuanwei L, Jiang D, Haiming S, et al. P300 event-related potential in abstinent methamphetamine-dependent patients. Physiol Behav. 2015;149:142–8.
Marhe R, Franken I. Error-related brain activity as a biomarker for cocaine relapse. Neuropsychopharmacology. 2014;39:241–41.
Franken IH, Stam CJ, Hendriks VM, van den Brink W. Electroencephalographic power and coherence analyses suggest altered brain function in abstinent male heroin-dependent patients. Neuropsychobiology. 2004;49:105–10.
Son KL, Choi JS, Lee J, Park SM, Lim JA, Lee JY, et al. Neurophysiological features of Internet gaming disorder and alcohol use disorder: a resting-state EEG study. Transl Psychiatry. 2015;5:e628.
Winterer G, Enoch MA, White KV, Saylan M, Coppola R, Goldman D. EEG phenotype in alcoholism: increased coherence in the depressive subtype. Acta Psychiatr Scand. 2003;108:51–60.
Putman P, Hermans E, van Honk J. Emotional stroop performance for masked angry faces: it’s BAS, not BIS. Emotion. 2004;4:305.
Kim KM, Choi SW, Lee J, Kim JW. EEG correlates associated with the severity of gambling disorder and serum BDNF levels in patients with gambling disorder. J Behav Addict. 2018;7:331–8.
Kohno M, Okita K, Morales AM, Robertson CL, Dean AC, Ghahremani DG, et al. Midbrain functional connectivity and ventral striatal dopamine D2-type receptors: link to impulsivity in methamphetamine users. Mol Psychiatry. 2016;21:1554–60.
London E. Impulsivity, stimulant abuse, and dopamine receptor signaling. Adv Pharmacol. 2016;76:67–84.
Mash LE, Keehn B, Linke AC, Liu TT, Helm JL, Haist F, et al. Atypical relationships between spontaneous EEG and fMRI activity in autism. Brain Connectivity. 2020;10:18–28.
Wade EC, Iosifescu DV. Using electroencephalography for treatment guidance in major depressive disorder. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2016;1:411–22.
Jasinska AJ, Chen BT, Bonci A, Stein EA. Dorsal medial prefrontal cortex (MPFC) circuitry in rodent models of cocaine use: implications for drug addiction therapies. Addiction Biol. 2015;20:215–26.
Koya E, Uejima JL, Wihbey KA, Bossert JM, Hope BT, Shaham Y. Role of ventral medial prefrontal cortex in incubation of cocaine craving. Neuropharmacology. 2009;56:177–85.
Courtney KE, Schacht JP, Hutchison K, Roche DJO, Ray LA. Neural substrates of cue reactivity: association with treatment outcomes and relapse. Addiction Biol. 2016;21:3–22.
Schacht JP, Anton RF, Myrick H. Functional neuroimaging studies of alcohol cue reactivity: a quantitative meta-analysis and systematic review. Addiction Biol. 2013;18:121–33.
Hanlon CA, Dowdle LT, Gibson NB, Li X, Hamilton S, Canterberry M, et al. Cortical substrates of cue-reactivity in multiple substance dependent populations: transdiagnostic relevance of the medial prefrontal cortex. Transl Psychiatry. 2018;8:186.
Dom G, Sabbe B, Hulstijn W, Van Den Brink W. Substance use disorders and the orbitofrontal cortex: systematic review of behavioural decision-making and neuroimaging studies. Br J Psychiatry. 2005;187:209–20.
Geng X, Hu Y, Gu H, Salmeron BJ, Adinoff B, Stein EA, et al. Salience and default mode network dysregulation in chronic cocaine users predict treatment outcome. Brain. 2017;140:1513–24.
Liang X, He Y, Salmeron BJ, Gu H, Stein EA, Yang Y. Interactions between the salience and default-mode networks are disrupted in cocaine addiction. J Neurosci. 2015;35:8081–90.
Su H, Liu Y, Yin D, Chen T, Li X, Zhong N, et al. Neuroplastic changes in resting-state functional connectivity after rTMS intervention for methamphetamine craving. Neuropharmacology. 2020;175:108177.
Ekhtiari H, Tavakoli H, Addolorato G, Baeken C, Bonci A, Campanella S, et al. Transcranial electrical and magnetic stimulation (tES and TMS) for addiction medicine: a consensus paper on the present state of the science and the road ahead. Neurosci Biobehav Rev. 2019;104:118–40.
Kearney-Ramos TE, Dowdle LT, Lench DH, Mithoefer OJ, Devries WH, George MS, et al. Transdiagnostic effects of ventromedial prefrontal cortex transcranial magnetic stimulation on cue reactivity. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2018;3:599–609.
Acknowledgements
General: We thank Yavin Shaham for critical comments on a draft of the paper. We thank Qian Zhuang, Bin Zhan, Xi He, Yexi Leng, Yaowen Liang, Yan Zeng, and Na Li for helps during data collection.
Funding
NSFC grant (81822017, 32020103008, 31900765), the Science and Technology Commission of Shanghai Municipality (18JC1420302, 18JC1420304), the Shanghai Municipal Science and Technology Major Project (2018SHZDZX05), Shanghai Sailing Program (19YF1441900), Shanghai Municipal Education Commission - Gaofeng Clinical Medicine Grant Support (20181715). We also thank the support from the Innovative Research Team of High-level Local Universities in Shanghai.
Author information
Authors and Affiliations
Contributions
TY, WL and DZ conceived and designed the study. DZ, MZ, WT, XC, LY and YL collected the data. DZ, MZ, WT, TX, WL and TY analyzed the data and wrote the paper together.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, D., Zhang, M., Tian, W. et al. Neurophysiological correlate of incubation of craving in individuals with methamphetamine use disorder. Mol Psychiatry 26, 6198–6208 (2021). https://doi.org/10.1038/s41380-021-01252-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-021-01252-5
This article is cited by
-
Assessment of rTMS treatment effects for methamphetamine addiction based on EEG functional connectivity
Cognitive Neurodynamics (2024)
-
Effect of aerobic exercise on brain metabolite profiles in the mouse models of methamphetamine addiction: LC-MS-based metabolomics study
BMC Psychiatry (2023)
-
Increased EEG gamma power under exposure to drug-related cues: a translational index for cue-elicited craving in METH-dependent individuals
BMC Psychiatry (2023)
-
Preventing incubation of drug craving to treat drug relapse: from bench to bedside
Molecular Psychiatry (2023)
-
Non-Invasive Brain-Computer Interfaces: a New Perspective on the Assessment and Classification of Individuals with Methamphetamine Addiction
SN Comprehensive Clinical Medicine (2023)