Abstract
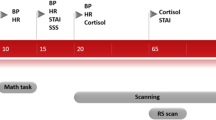
It is of great clinical importance to explore more efficacious treatments for OCD. Recently, cognitive-coping therapy (CCT), mainly focusing on recognizing and coping with a fear of negative events, has been reported as an efficacious psychotherapy. However, the underlying neurophysiological mechanism remains unknown. This study of 79 OCD patients collected Yale-Brown Obsessive Compulsive Scale (Y-BOCS) and resting-state functional magnetic resonance imaging (rs-fMRI) scans before and after four weeks of CCT, pharmacotherapy plus CCT (pCCT), or pharmacotherapy. Amygdala seed-based functional connectivity (FC) analysis was performed. Compared post- to pretreatment, pCCT-treated patients showed decreased left amygdala (LA) FC with the right anterior cingulate gyrus (cluster 1) and with the left paracentral lobule/the parietal lobe (cluster 2), while CCT-treated patients showed decreased LA-FC with the left middle occipital gyrus/the left superior parietal/left inferior parietal (cluster 3). The z-values of LA-FC with the three clusters were significantly lower after pCCT or CCT than pretreatment in comparisons of covert vs. overt and of non-remission vs. remission patients, except the z-value of cluster 2 in covert OCD. CCT and pCCT significantly reduced the Y-BOCS score. The reduction in the Y-BOCS score was positively correlated with the z-value of cluster 1. Our findings demonstrate that both pCCT and CCT with large effect sizes lowered LA-FC, indicating that FCs were involved in OCD. Additionally, decreased LA-FC with the anterior cingulate cortex (ACC) or paracentral/parietal cortex may be a marker for pCCT response or a marker for distinguishing OCD subtypes. Decreased LA-FC with the parietal region may be a common pathway of pCCT and CCT. Trial registration: ChiCTR-IPC-15005969.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Holes RE, Yudofsky SC, Roberts LW. Textbook of psychiatry. Arlington, VA: The American Psychiatric Publishing; 2014.
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211–24.
Maia TV, Cooney RE, Peterson BS. The neural bases of obsessive-compulsive disorder in children and adults. Dev Psychopathol. 2008;20:1251–83.
Marsh R, Horga G, Parashar N, Wang Z, Peterson BS, Simpson HB. Altered activation in fronto-striatal circuits during sequential processing of conflict in unmedicated adults with obsessive-compulsive disorder. Biol Psychiatry. 2014;75:615–22.
Paul S, Beucke JC, Kaufmann C, Mersov A, Heinzel S, Kathmann N, et al. Amygdala-prefrontal connectivity during appraisal of symptom-related stimuli in obsessive-compulsive disorder. Psychol Med. 2019;49:278–86.
Viol K, Aas B, Kastinger A, Kronbichler M, Schöller H, Reiter EM, et al. Individual OCD-provoking stimuli activate disorder-related and self-related neuronal networks in fMRI. Psychiatry Res Neuroimaging. 2019;283:135–44.
Kuhn S, Kaufmann C, Simon D, Endrass T, Gallinat J, Kathmann N. Reduced thickness of anterior cingulate cortex in obsessive-compulsive disorder. Cortex. 2013;49:2178–85.
Stern ER, Fitzgerald KD, Welsh RC, Abelson JL, Taylor SF. Resting-state functional connectivity between fronto-parietal and default mode networks in obsessive-compulsive disorder. PLoS ONE. 2012;7:3.
Jaspers-Fayer F, Lin SY, Chan E, Ellwyn R, Lim R, Best J, et al. Neural correlates of symptom provocation in pediatric obsessive-compulsive disorder. NeuroImage Clin. 2019;24:102034.
Boedhoe PS, Schmaal L, Abe Y, Ameis SH, Arnold PD, Batistuzzo MC, et al. Distinct subcortical volume alterations in pediatric and adult OCD: a worldwide meta- and mega-analysis. Am J Psychiatry. 2017;174:60–9.
Viol K, Aas B, Kastinger A, Kronbichler M, Schöller HJ, Reiter EM, et al. Erroneously disgusted: fMRI study supports disgust-related neural reuse in obsessive-compulsive disorder (OCD). Front Behav Neurosci. 2019;13:81.
Eng GK, Sim K, Chen S-HA. Meta-analytic investigations of structural grey matter, executive domain-related functional activations, and white matter diffusivity in obsessive compulsive disorder: an integrative review. Neurosci Biobehav Rev. 2015;52:233–57.
Hollander E, Bienstock CA, Koran LM, Pallanti S, Marazziti D, Rasmussen SA, et al. Refractory obsessive-compulsive disorder: state-of-the-art treatment. J Clin Psychiatry. 2002;63 Suppl 6:20–9.
Otte C. Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin Neurosci. 2011;13:413–21.
Saxena S, Gorbis E, O’Neill J, Baker SK, Mandelkern MA, Maidment KM, et al. Rapid effects of brief intensive cognitive-behavioral therapy on brain glucose metabolism in obsessive-compulsive disorder. Mol Psychiatry. 2009;14:197–205.
Baxter LR Jr., Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC, et al. Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch Gen Psychiatry. 1992;49:681–9.
Li P, Yang X, Greenshaw AJ, Li S, Luo J, Han H, et al. The effects of cognitive behavioral therapy on resting-state functional brain network in drug-naive patients with obsessive-compulsive disorder. Brain Behav. 2018;8:e00963.
Moody TD, Morfini F, Cheng G, Sheen C, Tadayonnejad R, Reggente N, et al. Mechanisms of cognitive-behavioral therapy for obsessive-compulsive disorder involve robust and extensive increases in brain network connectivity. Transl Psychiatry. 2017;7:e1230.
Feusner JD, Moody T, Lai TM, Sheen C, Khalsa S, Brown J, et al. Brain connectivity and prediction of relapse after cognitive-behavioral therapy in obsessive-compulsive disorder. Front Psychiatry. 2015;6:74.
Reggente N, Moody TD, Morfini F, Sheen C, Rissman J, O’Neill J, et al. Multivariate resting-state functional connectivity predicts response to cognitive behavioral therapy in obsessive-compulsive disorder. Proc Natl Acad Sci USA. 2018;115:2222–7.
Ma JD, Wang CH, Li HF, Zhang XL, Zhang YL, Hou YH, et al. Cognitive-coping therapy for obsessive-compulsive disorder: a randomized controlled trial. J Psychiatr Res. 2013;47:1785–90.
Hu X-Z. A novel cognitive-coping therapy for obsessive-complusive disorder. J Appl Clin Pediatr. 2010;25:1848–51.
Hu X-Z, Ma J-D. Clinical effect of pharmacotherapy combined with cognitive-coping therapy on obsessive-compulsive disorder. J Xinxiang Med Coll. 2011;28:68–72.
Hu XZ, Wen YS, Ma JD, Han DM, Li YX, Wang SF. A promising randomized trial of a new therapy for obsessive-compulsive disorder. Brain Behav. 2012;2:443–54.
Hu XZ, Ma JD, Huang P, Shan XW, Zhang ZH, Zhang JH, et al. Highly efficacious cognitive-coping therapy for overt or covert compulsions. Psychiatry Res. 2015;229:732–8.
Sang DE, Shi LJ, Yue KC, He CY, Zhao HZ, Wang CH, et al. Clinical remission of a treatment-refractory individual with severe repetitive rituals and rumination. Asian J Psychiatr. 2020;47:101878.
Ji G, Wei W, Yue K-C, Li H, Shi L-J, Ma J-D, et al. Effects of the COVID-19 pandemic on obsessive-compulsive symptoms among university students: prospective cohort survey study. J Med Internet Res. 2020;22:e21915.
Szeszko PR, MacMillan S, McMeniman M, Lorch E, Madden R, Ivey J, et al. Amygdala volume reductions in pediatric patients with obsessive-compulsive disorder treated with paroxetine: preliminary findings. Neuropsychopharmacology. 2004;29:826–32.
Viard A, Flament MF, Artiges E, Dehaene S, Naccache L, Cohen D, et al. Cognitive control in childhood-onset obsessive-compulsive disorder: a functional MRI study. Psychol Med. 2005;35:1007–17.
Milad MR, Rauch SL. Obsessive-compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci. 2012;16:43–51.
van Velzen LS, de Wit SJ, Ćurĉić-Blake B, Cath DC, de Vries FE, Veltman DJ, et al. Altered inhibition-related frontolimbic connectivity in obsessive-compulsive disorder. Hum Brain Mapp. 2015;36:4064–75.
de Vries FE, de Wit SJ, Cath DC, van der Werf YD, van der Borden V, van Rossum TB, et al. Compensatory frontoparietal activity during working memory: an endophenotype of obsessive-compulsive disorder. Biol Psychiatry. 2014;76:878–87.
Göttlich M, Krämer UM, Kordon A, Hohagen F, Zurowski B. Resting-state connectivity of the amygdala predicts response to cognitive behavioral therapy in obsessive compulsive disorder. Biol Psychol. 2015;111:100–9.
Hayasaka Y, Purgato M, Magni LR, Ogawa Y, Takeshima N, Cipriani A, et al. Dose equivalents of antidepressants: Evidence-based recommendations from randomized controlled trials. J Affect Disord. 2015;180:179–84.
Yan C-G, Zang Y-F. DPARSF: A MATLAB Toolbox for “Pipeline” Data Analysis of Resting-State fMRI. Front Syst Neurosci. 2010;4:13.
Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Steps toward optimizing motion artifact removal in functional connectivity MRI; a reply to Carp. NeuroImage. 2013;76:439–41.
Thorsen AL, Hagland P, Radua J, Mataix-Cols D, Kvale G, Hansen B, et al. Emotional processing in obsessive-compulsive disorder: a systematic review and meta-analysis of 25 functional neuroimaging studies. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3:563–71.
Zikopoulos B, Höistad M, John Y, Barbas H. Posterior orbitofrontal and anterior cingulate pathways to the amygdala target inhibitory and excitatory systems with opposite functions. J Neurosci. 2017;37:5051–64.
Adler CM, McDonough-Ryan P, Sax KW, Holland SK, Arndt S, Strakowski SM. fMRI of neuronal activation with symptom provocation in unmedicated patients with obsessive compulsive disorder. J Psychiatr Res. 2000;34:317–24.
Perani D, Colombo C, Bressi S, Bonfanti A, Grassi F, Scarone S, et al. [18F]FDG PET study in obsessive-compulsive disorder. A clinical/metabolic correlation study after treatment. Br J Psychiatry. 1995;166:244–50.
Lustberg D, Iannitelli AF, Tillage RP, Pruitt M, Liles LC, Weinshenker D. Central norepinephrine transmission is required for stress-induced repetitive behavior in two rodent models of obsessive-compulsive disorder. Psychopharmacology. 2020;237:1973–87.
Senova S, Clair A-H, Palfi S, Yelnik J, Domenech P, Mallet L. Deep brain stimulation for refractory obsessive-compulsive disorder: towards an individualized approach. Front Psychiatry. 2019;10:905.
Bjorgvinsson T, Hart J, Heffelfinger S. Obsessive-compulsive disorder: update on assessment and treatment. J Psychiatr Pract. 2007;13:362–72.
O’Neill J, Gorbis E, Feusner JD, Yip JC, Chang S, Maidment KM, et al. Effects of intensive cognitive-behavioral therapy on cingulate neurochemistry in obsessive-compulsive disorder. J Psychiatr Res. 2013;47:494–504.
Rus OG, Reess TJ, Wagner G, Zimmer C, Zaudig M, Koch K. Functional and structural connectivity of the amygdala in obsessive-compulsive disorder. NeuroImage Clin. 2017;13:246–55.
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev. 2008;32:525–49.
Nordahl TE, Benkelfat C, Semple WE, Gross M, King AC, Cohen RM. Cerebral glucose metabolic rates in obsessive compulsive disorder. Neuropsychopharmacology. 1989;2:23–8.
Kwon JS, Kim JJ, Lee DW, Lee JS, Lee DS, Kim MS, et al. Neural correlates of clinical symptoms and cognitive dysfunctions in obsessive-compulsive disorder. Psychiatry Res. 2003;122:37–47.
Goncalves OF, Marques TR, Lori NF, Sampaio A, Branco MC. Obsessive-compulsive disorder as a visual processing impairment. Med Hypotheses. 2010;74:107–9.
Gonçalves ÓF, Carvalho S, Leite J, Fernandes-Gonçalves A, Carracedo A, Sampaio A. Cognitive and emotional impairments in obsessive-compulsive disorder: evidence from functional brain alterations. Porto Biomed J. 2016;1:92–105.
Tadayonnejad R, Deshpande R, Ajilore O, Moody T, Morfini F, Ly R, et al. Pregenual anterior cingulate dysfunction associated with depression in OCD: an integrated multimodal fMRI/(1)H MRS study. Neuropsychopharmacology. 2018;43:1146–55.
Cardoner N, Soriano-Mas C, Pujol J, Alonso P, Harrison BJ, Deus J, et al. Brain structural correlates of depressive comorbidity in obsessive-compulsive disorder. NeuroImage. 2007;38:413–21.
Kong XZ, Boedhoe PSW, Abe Y, Alonso P, Ameis SH, Arnold PD, et al. Mapping cortical and subcortical asymmetry in obsessive-compulsive disorder: findings from the ENIGMA consortium. Biol Psychiatry. 2020;87:1022–34.
Remijnse PL, van den Heuvel OA, Nielen MM, Vriend C, Hendriks GJ, Hoogendijk WJ, et al. Cognitive inflexibility in obsessive-compulsive disorder and major depression is associated with distinct neural correlates. PLoS ONE. 2013;8:e59600.
Saxena S, Brody AL, Ho ML, Alborzian S, Ho MK, Maidment KM, et al. Cerebral metabolism in major depression and obsessive-compulsive disorder occurring separately and concurrently. Biol Psychiatry. 2001;50:159–70.
Acknowledgements
The authors acknowledge support from the National Natural Foundation of China (81671365). The funder played no role in the preparation, review, or approval of the paper or decision to submit the paper for publication. We thank Tao Lou, Xingxia Zhu, Xiao-Xia Li, Min Sun, Hua Zheng, and Qiang Li from the Second Affiliated Hospital of Xinxiang Medical University for their efforts on data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhao, Z., Wang, CH., Ma, JD. et al. Decreased left amygdala functional connectivity by cognitive-coping therapy in obsessive-compulsive disorder. Mol Psychiatry 26, 6952–6962 (2021). https://doi.org/10.1038/s41380-021-01131-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-021-01131-z