Abstract
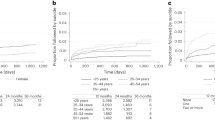
The role of sex, race, and suicide method on recent increases in suicide mortality in the United States remains unclear. Estimating the age, period, and cohort effects underlying suicide mortality trends can provide important insights for the causal hypothesis generating process. We generated updated age-period-cohort effect estimates of recent suicide mortality rates in the US, examining the putative roles of sex, race, and method for suicide, using data from all death certificates in the US between 1999 and 2018. After designating deaths as attributable to suicide according to ICD-10 underlying cause of death codes X60-X84, Y87.0, and U03, we (i) used hexagonal grids to describe rates of suicide by age, period, and cohort visually and (ii) modeled sex-, race-, and suicide method-specific age, period, and cohort effects. We found that, while suicide mortality increased in the US between 1999 and 2018 across age, sex, race, and suicide method, there was substantial heterogeneity in age and cohort effects by method, sex, and race, with a first peak of suicide risk in youth, a second peak in older ages—specific to male firearm suicide, and increased rates among younger cohorts of non-White individuals. Our findings should prompt discussion regarding age-specific clinical firearm safety interventions, drivers of minoritized populations’ adverse early-life experiences, and racial differences in access to and quality of mental healthcare.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Turecki G, Brent DA, Gunnel D, O’Connor RC, Oquendo MA, Pirkis J, et al. Suicide and suicide risk. Nat Rev Dis Prim. 2019;5:74.
Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Web‐based Injury Statistics Query and Reporting System (WISQARS). 2020. www.cdc.gov/injury/wisqars/index.html.
Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019;364:l94.
Hedegaard H, Curtin SC, Warner M. Increase in suicide mortality in the United States, 1999–2018. NCHS Data Brief. 2020. https://www.cdc.gov/nchs/data/databriefs/db362-h.pdf.
Baker SP, Hu G, Wilcox HC, Baker TD. Increase in suicide by hanging/suffocation in the U.S., 2000–2010. Am J Prev Med. 2013;44:146–9.
Keyes KM, Li G. Age-period-cohort modeling. In: Li G, Baker S, editors. Injury research. Boston, MA: Springer; 2012. https://doi.org/10.1007/978-1-4614-1599-2_22
Susser M. Commentary: the longitudinal perspective and cohort analysis. Int J Epidemiol. 2001;30:684–7.
Phillips JA. A changing epidemiology of suicide? The influence of birth cohorts on suicide rates in the United States. Soc Sci Med. 2014;114:151–60.
Park S, Song Y-J, Kim J, Ki M, Shin JY, Kwon YM, et al. Age, period, and cohort effects on suicide mortality in South Korea, 1992−2015. Int J Environ Res Public Health. 2018;15. https://doi.org/10.3390/ijerph15081580
Cha ES, Chang S-S, Choi Y, Lee WJ. Trends in pesticide suicide in South Korea, 1983-2014. Epidemiol Psychiatr Sci. 2019;29:e25.
Chen X, Sun Y, Li Z, Yu B, Gao G, Wang P. Historical trends in suicide risk for the residents of mainland China: APC modeling of the archived national suicide mortality rates during 1987–2012. Soc Psychiatry Psychiatr Epidemiol. 2019;54:99–110.
Chung RY, Yip BHK, Chan SSM, Wong SYS. Cohort effects of suicide mortality are sex specific in the rapidly developed Hong Kong Chinese population, 1976–2010. Depress Anxiety. 2016;33:558–66.
Ajdacic–Gross V, Bopp M, Gostynski M, Lauber C, Gutzwiller F, Rössler W. Age–period–cohort analysis of Swiss suicide data, 1881–2000. Eur Arch Psychiatry Clin Neurosci. 2006;256:207–14.
Gunnell D, Middleton N, Whitley E, Dorling D, Frankel S. Influence of cohort effects on patterns of suicide in England and Wales, 1950–1999. Br J Psychiatry. 2003;182:164–70.
Odagiri Y, Uchida H, Nakano M. Gender differences in age, period, and birth-cohort effects on the suicide mortality rate in Japan, 1985–2006. Asia Pac J Public Heal. 2009;23:581–7.
Yu B, Chen X. Age and birth cohort–adjusted rates of suicide mortality among US male and female youths aged 10 to 19 years from 1999 to 2017. JAMA Netw Open. 2019;2:e1911383–e1911383.
Wang Z, Yu C, Wang J, Bao J, Gao X, Xiang H. Age-period-cohort analysis of suicide mortality by gender among white and black Americans, 1983-2012. Int J Equity Health. 2016;15:107.
Haviland MJ, Rowhani-Rahbar A, Rivara FP. Age, period and cohort effects in firearm homicide and suicide in the USA, 1983–2017. Inj Prev. 2020. https://doi.org/10.1136/injuryprev-2020-043714.
Conner A, Azrael D, Miller M. Suicide case-fatality rates in the United States, 2007 to 2014. Ann Intern Med. 2019;171:885–95.
Council NR. Vital statistics: summary of a workshop. (Siri MJ, Cork DL, eds.). Washington, DC: The National Academies Press; 2009. https://doi.org/10.17226/12714.
Jalal H, Burke DS. Hexamaps for age–period–cohort data visualization and implementation in R. Epidemiology. 2020. https://journals.lww.com/epidem/Fulltext/9000/Hexamaps_for_Age_Period_Cohort_Data_Visualization.98384.aspx.
Clayton D, Schifflers E. Models for temporal variation in cancer rates. II: age-period-cohort models. Stat Med. 1987;6:469–81.
Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries. Int J Epidemiol. 2003;32:902–9.
Smith TW, Son J. General Social Survey Final Report: Trends in Gun Ownership in the United States, 1972–2018. Published online in 2020. https://www.norc.org/Research/Projects/Pages/general-social-survey.aspx. Accessed 2 Mar 2021.
McKnight R, Levine PB. Three million more guns: The Spring 2020 spike in firearm sales. Brookings. Published July 13, 2020. https://www.brookings.edu/blog/up-front/2020/07/13/three-million-more-guns-the-spring-2020-spike-in-firearm-sales/. Accessed 2 Mar 2021.
National Institute of Mental Health. NIMH Suicide Statistics. 2018. https://www.nimh.nih.gov/health/statistics/suicide.shtml#part_154971.
Hassan A. Deaths from drugs and suicide reach a record in the US. The New York Times. 2019. https://www.nytimes.com/2019/03/07/us/deaths-drugs-suicide-record.html.
Bureau of Justice Statistics. Key facts at a glance: firearm deaths by intent, 1991–2001. 2010. https://web.archive.org/web/20130118071124/http:/bjs.ojp.usdoj.gov/content/glance/tables/frmdth.cfm.
Preventing suicide by limiting access to guns. Harvard Sch Public Heal News. 2020. https://www.hsph.harvard.edu/news/hsph-in-the-news/preventing-suicide-by-limiting-access-to-guns/.
Miller M, Barber C, White RA, Azrael D. Firearms and suicide in the United States: Is risk independent of underlying suicidal behavior? Am J Epidemiol. 2013;178:946–55.
Siegel M, Rothman EF. Firearm ownership and suicide rates among US men and women, 1981–2013. Am J Public Health. 2016;106:1316–22.
Studdert DM, Zhang Y, Swanson SA, Prince L, Rodden JA, Holsinger EE, et al. Handgun ownership and suicide in California. N Engl J Med. 2020;382:2220–9.
Smith PN, Currier J, Drescher K. Firearm ownership in veterans entering residential PTSD treatment: associations with suicide ideation, attempts, and combat exposure. Psychiatry Res. 2015;229:220–4.
Wang J, Sumner SA, Simon TR, Crosby AE, Annor FB, Gaylor E, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006 to 2015. JAMA Psychiatry. 2020;77:684–93.
Ludwig J, Cook PJ. Homicide and suicide rates associated with implementation of the Brady Handgun Violence Prevention Act. JAMA. 2000;284:585–91.
Rodríguez Andrés A, Hempstead K. Gun control and suicide: the impact of state firearm regulations in the United States, 1995-2004. Health Policy. 2011;101:95–103.
Giffords Law Center to Prevent Gun Violence. Minimum age to purchase & possess. 2020. https://giffords.org/lawcenter/gun-laws/policy-areas/who-can-have-a-gun/minimum-age/.
Raifman J, Larson E, Barry CL, Siegel M, Ulrich M, Knopov A, et al. State handgun purchase age minimums in the US and adolescent suicide rates: regression discontinuity and difference-in-differences analyses. BMJ. 2020;370. https://doi.org/10.1136/bmj.m2436.
Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138:e20161878.
Keyes KM, Gary D, O’Malley PM, Hamilton A, Schulenberg JE. Recent increases in depressive symptoms among US adolescents: trends from 1991–2018. Soc Psychiatry Psychiatr Epidemiol. 2019;54:987–96.
Plemmons G, Hall M, Doupnik S, Gay J, Brown C, Browning W, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics. 2018;141:e20172426.
Centers for Disease Control and Prevention. Trends in the prevalence of suicide-related behaviors national YRBS: 1997–2017. Youth Risk Behav Surv. 2018. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/2017_suicide_trend_yrbs.pdf.
Stone DM, Simon TR, Fowler KA, Kegler SR, Yuan K, Holland KM, et al. Vital Signs: Trends in state suicide rates—United States, 1999–2016 and circumstances contributing to suicide—27 states, 2015. Morb Mortal Wkly Rep. 2018;67:617–24.
Oquendo MA, Volkow ND. Suicide: a silect contributor to opioid-overdose deaths. N. Engl J Med. 2018;378:1567–9.
Kaiser Family Foundation. Opioid overdose deaths by race/ethnicity. 2020. https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
Nunn KB. Race, crime and the pool of surplus criminality: or why the war on drugs was a war on blacks. J Gender, Race Justice. 2002;6.
Moore LD, Elkavich A. Who’s using and who’s doing time: incarceration, the war on drugs, and public health. Am J Public Health. 2008;98:S176–S180.
Clear T. Imprisoning communities: how mass incarceration makes disadvantaged neighborhoods worse. New York, NY: Oxford University Press; 2007.
Wildeman C, Goldman AW, Lee H. Health consequences of family member incarceration for adults in the household. Public Health Rep. 2019;134:15S–21S.
Kajeepeta S, Rutherford CG, Keyes KM, El-Sayed AM, Prins SJ. County jail incarceration rates and county mortality rates in the United States, 1987–2016. Am J Public Health. 2020;110:S109–S115.
Bakst SS, Braun T, Zucker I, Amitai Z, Shohat T. The accuracy of suicide statistics: are true suicide deaths misclassified? Soc Psychiatry Psychiatr Epidemiol. 2016;51:115–23.
De Leo D. Can we rely on suicide mortality data? Cris J Cris Inter Suicide Prev. 2015;36:1–3.
Gunnell D, Bennewith O, Simkin S, Cooper J, Klineberg E, Rodway C, et al. Time trends in coroners’ use of different verdicts for possible suicides and their impact on officially reported incidence of suicide in England: 1990–2005. Psychol Med. 2013;43:1415–22.
Silva C, Van Orden KA. Suicide among Hispanics in the United States. Curr Opin Psychol. 2018;22:44–49.
The President´s roadmap to empower veterans and end a national tragedy of suicide. https://www.va.gov/PREVENTS/EO-13861.asp. Accessed 10 Dec 2020.
Lee-Tauler SY, Progovac AM, Samson F, Sanchez MJ. A review of mental health and mental health care disparities research: 2011–2014. Med Care Res Rev. 2019;76:683–710.
Alegria M, Nakash O, Johnson K, et al. Effectiveness of the DECIDE interventions on shared decision making and perceived quality of care in behavioral health with multicultural patients: a randomized clinical trial. JAMA Psychiatry. 2018;75:325–35.
Acknowledgements
This work was funded by the National Institute of Mental Health (R01-MH121410). The funder/sponsor had no role in the conception, design, or execution of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JS and Columbia University declare partial ownership of SK Analytics. SK was a consultant for SK Analytics. JS was a consultant for BNI. KK has been compensated as an expert witness in litigation. No other disclosures were reported.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41380_2021_1078_MOESM1_ESM.docx
Supplementary Tables and Figures Age, period, and cohort effects on suicide death in the US from 1999 to 2018: moderation by sex, race, and firearm involvement
Rights and permissions
About this article
Cite this article
Martínez-Alés, G., Pamplin, J.R., Rutherford, C. et al. Age, period, and cohort effects on suicide death in the United States from 1999 to 2018: moderation by sex, race, and firearm involvement. Mol Psychiatry 26, 3374–3382 (2021). https://doi.org/10.1038/s41380-021-01078-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-021-01078-1
This article is cited by
-
Sleep deprivation and suicide risk among minoritized US adolescents
BMC Psychiatry (2023)
-
Acculturation and suicide-related risk in ethnoracially minoritized youth in the US: a scoping review and content analysis of the empirical evidence
Social Psychiatry and Psychiatric Epidemiology (2023)
-
Sexual orientation-related patterns of 12-month course and severity of suicidality in a longitudinal, population-based cohort of young adults in Sweden
Social Psychiatry and Psychiatric Epidemiology (2022)