Abstract
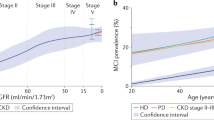
Amyloid-β (Aβ) accumulation in the brain is a pivotal event in the pathogenesis of Alzheimer’s disease (AD), and its clearance from the brain is impaired in sporadic AD. Previous studies suggest that approximately half of the Aβ produced in the brain is cleared by transport into the periphery. However, the mechanism and pathophysiological significance of peripheral Aβ clearance remain largely unknown. The kidney is thought to be responsible for Aβ clearance, but direct evidence is lacking. In this study, we investigated the impact of unilateral nephrectomy on the dynamic changes in Aβ in the blood and brain in both humans and animals and on behavioural deficits and AD pathologies in animals. Furthermore, the therapeutic effects of the diuretic furosemide on Aβ clearance via the kidney were assessed. We detected Aβ in the kidneys and urine of both humans and animals and found that the Aβ level in the blood of the renal artery was higher than that in the blood of the renal vein. Unilateral nephrectomy increased brain Aβ deposition; aggravated AD pathologies, including Tau hyperphosphorylation, glial activation, neuroinflammation, and neuronal loss; and aggravated cognitive deficits in APP/PS1 mice. In addition, chronic furosemide treatment reduced blood and brain Aβ levels and attenuated AD pathologies and cognitive deficits in APP/PS1 mice. Our findings demonstrate that the kidney physiologically clears Aβ from the blood, suggesting that facilitation of Aβ clearance via the kidney represents a novel potential therapeutic approach for AD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Alzheimer’s Association . 2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 2020. https://doi.org/10.1002/alz.12068.
Braak H, Del, Trecidi K. Neuroanatomy and pathology of sporadic Alzheimer’s disease. Adv Anat Embryol Cell Biol. 2015;215:1–162.
Hardy JA, Higgins GA. Alzheimer’s disease: the amyloid cascade hypothesis. Science. 1992;256:184–5.
Beyreuther K, Masters CL. Amyloid precursor protein (APP) and beta A4 amyloid in the etiology of Alzheimer’s disease: precursor-product relationships in the derangement of neuronal function. Brain Pathol. 1991;1:241–51.
Mawuenyega KG, Sigurdson W, Ovod V, Munsell L, Kasten T, Morris JC, et al. Decreased clearance of CNS beta-amyloid in Alzheimer’s disease. Science. 2010;330:1774.
Panza F, Lozupone M, Logroscino G, Imbimbo BP. A critical appraisal of amyloid-beta targeting therapies for Alzheimer disease. Nat Rev Neurol. 2019;15:73–88.
Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, et al. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015;11:457–70.
Wang J, Gu BJ, Masters CL, Wang YJ. A systemic view of Alzheimer disease - insights from amyloid-beta metabolism beyond the brain. Nat Rev Neurol. 2017;13:612–23.
Deane R, Bell RD, Sagare A, Zlokovic BV. Clearance of amyloid-beta peptide across the blood-brain barrier: implication for therapies in Alzheimer’s disease. CNS Neurol Disord Drug Targets. 2009;8:16–30.
Sweeney MD, Zlokovic BV. A lymphatic waste-disposal system implicated in Alzheimer’s disease. Nature. 2018;560:172–4.
Cheng Y, Wang YJ. Meningeal lymphatic vessels: a drain of the brain involved in neurodegeneration? Neurosci Bull. 2020;36:557–60.
Qosa H, Abuasal BS, Romero IA, Weksler B, Couraud PO, Keller JN, et al. Differences in amyloid-beta clearance across mouse and human blood-brain barrier models: kinetic analysis and mechanistic modeling. Neuropharmacology. 2014;79:668–78.
Yuede CM, Lee H, Restivo JL, Davis TA, Hettinger JC, Wallace CE, et al. Rapid in vivo measurement of beta-amyloid reveals biphasic clearance kinetics in an Alzheimer’s mouse model. J Exp Med. 2016;213:677–85.
Xiang Y, Bu XL, Liu YH, Zhu C, Shen LL, Jiao SS, et al. Physiological amyloid-beta clearance in the periphery and its therapeutic potential for Alzheimer’s disease. Acta Neuropathol. 2015;130:487–99.
Sun BL, Chen Y, Fan DY, Zhu C, Zeng F, Wang YJ. Critical thinking on amyloid-beta-targeted therapy: challenges and perspectives. Sci China Life sci. 2020. https://doi.org/10.1007/s11427-020-1810-y.
Verberk IMW, Slot RE, Verfaillie SCJ, Heijst H, Prins ND, van Berckel BNM, et al. Plasma amyloid as prescreener for the earliest Alzheimer pathological changes. Ann Neurol. 2018;84:648–58.
Jiao SS, Bu XL, Liu YH, Zhu C, Wang QH, Shen LL, et al. Sex dimorphism profile of Alzheimer’s disease-type pathologies in an APP/PS1 mouse model. Neurotox Res. 2016;29:256–66.
Jiao SS, Yao XQ, Liu YH, Wang QH, Zeng F, Lu JJ, et al. Edaravone alleviates Alzheimer’s disease-type pathologies and cognitive deficits. Proc Natl Acad Sci USA. 2015;112:5225–30.
Ghiso J, Calero M, Matsubara E, Governale S, Chuba J, Beavis R, et al. Alzheimer’s soluble amyloid beta is a normal component of human urine. FEBS Lett. 1997;408:105–8.
Nielsen R, Christensen EI, Birn H. Megalin and cubilin in proximal tubule protein reabsorption: from experimental models to human disease. Kidney Int. 2016;89:58–67.
Dietrich M, Antequera D, Pascual C, Castro N, Bolos M, Carro E. Alzheimer’s disease-like impaired cognition in endothelial-specific megalin-null mice. J Alzheimer’s Dis. 2014;39:711–7.
Stanciu GD, Ababei DC, Bild V, Bild W, Paduraru L, Gutu MM, et al. Renal Contributions in the pathophysiology and neuropathological substrates shared by chronic kidney disease and Alzheimer’s disease. Brain Sci. 2020;10:563.
Liu YH, Xiang Y, Wang YR, Jiao SS, Wang QH, Bu XL, et al. Association between serum amyloid-beta and renal functions: implications for roles of kidney in amyloid-beta clearance. Mol Neurobiol. 2015;52:115–9.
Sakai K, Senda T, Hata R, Kuroda M, Hasegawa M, Kato M, et al. Patients that have undergone hemodialysis exhibit lower amyloid deposition in the brain: evidence supporting a therapeutic strategy for Alzheimer’s disease by removal of blood amyloid. J Alzheimers Dis. 2016;51:997–1002.
Gronewold J, Klafki HW, Baldelli E, Kaltwasser B, Seidel UK, Todica O, et al. Factors responsible for plasma beta-amyloid accumulation in chronic kidney disease. Mol Neurobiol. 2016;53:3136–45.
O’Sullivan ED, Hughes J, Ferenbach DA. Renal aging: causes and consequences. J Am Soc Nephrology. 2017;28:407–20.
Kuro OM. The Klotho proteins in health and disease. Nat Rev Nephrol. 2019;15:27–44.
Jansen WJ, Ossenkoppele R, Knol DL, Tijms BM, Scheltens P, Verhey FR, et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA. 2015;313:1924–38.
Liu YH, Giunta B, Zhou HD, Tan J, Wang YJ. Immunotherapy for Alzheimer’s disease: the challenge of adverse effects. Nat Rev Neurol. 2012;8:465–9.
Iijima-Ando K, Hearn SA, Granger L, Shenton C, Gatt A, Chiang HC, et al. Overexpression of neprilysin reduces Alzheimer amyloid-beta42 (Abeta42)-induced neuron loss and intraneuronal Abeta42 deposits but causes a reduction in cAMP-responsive element-binding protein-mediated transcription, age-dependent axon pathology, and premature death in Drosophila. J Biol Chem. 2008;283:19066–76.
Jin WS, Shen LL, Bu XL, Zhang WW, Chen SH, Huang ZL, et al. Peritoneal dialysis reduces amyloid-beta plasma levels in humans and attenuates Alzheimer-associated phenotypes in an APP/PS1 mouse model. Acta Neuropathol. 2017;134:207–20.
Boada M, Lopez OL, Olazaran J, Nunez L, Pfeffer M, Paricio M, et al. A randomized, controlled clinical trial of plasma exchange with albumin replacement for Alzheimer’s disease: primary results of the AMBAR Study. Alzheimers Dement. 2020;16:1412–25.
Ding XL, Lei P. Plasma replacement therapy for Alzheimer’s disease. Neurosci Bull. 2020;36:89–90.
Chuang YF, Breitner JCS, Chiu YL, Khachaturian A, Hayden K, Corcoran C, et al. Use of diuretics is associated with reduced risk of Alzheimer’s disease: the Cache County Study. Neurobiol Aging. 2014;35:2429–35.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (91749206, 81930028, 81625007, and 31921003).
Author information
Authors and Affiliations
Contributions
Y.J.W., J.W., and H.W.Z. conceived and designed the project, D.Y.T., X.L.H., Y.Y.S., G.H.Z., and S.H.C. conducted patient enrolment, assessment, and sample treatment, D.Y.T., Y.C., Z.Q.Z., C.Y.H., Q.G.P, M.Z.T., Y.R.W., H.L.S., P.Y.S., Z.Y.Y., D.Y.F., X.L.B., J.W., and C.R.T. conducted animal and in vitro experiments, D.Y.T., Y.C., and C.R.T. analysed data, D.Y.T. and Y.J.W. wrote the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tian, DY., Cheng, Y., Zhuang, ZQ. et al. Physiological clearance of amyloid-beta by the kidney and its therapeutic potential for Alzheimer’s disease. Mol Psychiatry 26, 6074–6082 (2021). https://doi.org/10.1038/s41380-021-01073-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-021-01073-6
This article is cited by
-
Heart rate and breathing effects on attention and memory (HeartBEAM): study protocol for a randomized controlled trial in older adults
Trials (2024)
-
Modulating heart rate oscillation affects plasma amyloid beta and tau levels in younger and older adults
Scientific Reports (2023)
-
Advances in Molecular Psychiatry – March 2023: mitochondrial function, stress, neuroinflammation – bipolar disorder, psychosis, and Alzheimer’s disease
Molecular Psychiatry (2023)
-
Ferulic Acid Improves Synaptic Plasticity and Cognitive Impairments by Alleviating the PP2B/DARPP-32/PP1 Axis-Mediated STEP Increase and Aβ Burden in Alzheimer's Disease
Neurotherapeutics (2023)
-
Associations of Blood and Cerebrospinal Fluid Aβ and tau Levels with Renal Function
Molecular Neurobiology (2023)