Abstract
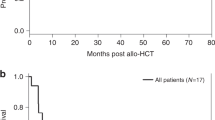
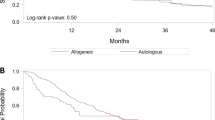
Blastic plasmacytoid dendritic cell neoplasia (BPDCN) is a rare myeloid malignancy with a generally poor prognosis. Although preliminary evidence suggests that hematopoietic cell transplantation (HCT) could improve outcome in patients with BPDCN, the individual contributions of conditioning and graft-versus-tumor (GVT) effects to HCT success are undefined. We present a retrospective study of 162 adult patients who underwent a first HCT (allogeneic 146, autologous 16) between 2009 and 2017, and were registered with the EBMT. Median age was 57 (range 20–73) years, and disease status at HCT was first complete remission (CR1) in 78%. Among patients receiving allogeneic HCT (alloHCT), myeloablative conditioning (MAC), reduced intensity conditioning (RIC) and in-vivo T-cell depletion (TCD) were used in 54%, 46%, and 59% respectively. Total body irradiation (TBI) was the conditioning backbone in 61% of MAC and 26% of RIC transplants. One-year overall survival (OS) and progression-free survival (PFS) rates were comparable after alloHCT and autologous HCT (autoHCT). Among alloHCT recipients, MAC with TBI significantly improved OS and PFS, independently of CR1, age, Karnofsky index and TCD. Accordingly, MAC (ideally based on TBI) should be preferred for alloHCT recipients with BPDCN. In patients who are not elegible for MAC alloHCT, autoHCT could be considered.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The dataset analysed during the current study is available from the EBMT ProMISe databank on reasonable request to protect the privacy of the patients.
References
Herling M, Teitell MA, Shen RR, Medeiros LJ, Jones D. TCL1 expression in plasmacytoid dendritic cells (DC2s) and the related CD4+ CD56+ blastic tumors of skin. Blood. 2003;101:5007–9.
Laribi K, Baugier de Materre A, Sobh M, Cerroni L, Valentini CG, Aoki T, et al. Blastic plasmacytoid dendritic cell neoplasms: results of an international survey on 398 adult patients. Blood Adv. 2020;4:4838–48.
Garnache-Ottou F, Vidal C, Biichle S, Renosi F, Poret E, Pagadoy M, et al. How should we diagnose and treat blastic plasmacytoid dendritic cell neoplasm patients? Blood Adv. 2019;3:4238–51.
Martin-Martin L, Almeida J, Pomares H, Gonzalez-Barca E, Bravo P, Gimenez T, et al. Blastic plasmacytoid dendritic cell neoplasm frequently shows occult central nervous system involvement at diagnosis and benefits from intrathecal therapy. Oncotarget. 2016;7:10174–81.
Taylor J, Haddadin M, Upadhyay VA, Grussie E, Mehta-Shah N, Brunner AM, et al. Multicenter analysis of outcomes in blastic plasmacytoid dendritic cell neoplasm offers a pretargeted therapy benchmark. Blood 2019;134:678–87.
Reimer P, Rudiger T, Kraemer D, Kunzmann V, Weissinger F, Zettl A, et al. What is CD4+CD56+ malignancy and how should it be treated? Bone Marrow Transplant. 2003;32:637–46.
Dietrich S, Andrulis M, Hegenbart U, Schmitt T, Bellos F, Martens UM, et al. Blastic plasmacytoid dendritic cell neoplasia (BPDC) in elderly patients: results of a treatment algorithm employing allogeneic stem cell transplantation with moderately reduced conditioning intensity. Biol Blood Marrow Transplant. 2011;17:1250–4.
Roos-Weil D, Dietrich S, Boumendil A, Polge E, Bron D, Carreras E, et al. Stem cell transplantation can provide durable disease control in blastic plasmacytoid dendritic cell neoplasm: a retrospective study from the European Group for Blood and Marrow Transplantation. Blood. 2013;121:440–6.
Aoki T, Suzuki R, Kuwatsuka Y, Kako S, Fujimoto K, Taguchi J, et al. Long-term survival following autologous and allogeneic stem cell transplantation for blastic plasmacytoid dendritic cell neoplasm. Blood. 2015;125:3559–62.
Kharfan-Dabaja MA, Reljic T, Murthy HS, Ayala E, Kumar A. Allogeneic hematopoietic cell transplantation is an effective treatment for blastic plasmacytoid dendritic cell neoplasm in first complete remission: systematic review and meta-analysis. Clin Lymphoma Myeloma Leuk. 2018;18:703–9.e1
Kharfan-Dabaja MA, Al Malki MM, Deotare U, Raj RV, El-Jurdi N, Majhail N, et al. Haematopoietic cell transplantation for blastic plasmacytoid dendritic cell neoplasm: a North American multicentre collaborative study. Br J Haematol. 2017;179:781–9.
Yun S, Chan O, Kerr D, Vincelette ND, Idrees A, Mo Q, et al. Survival outcomes in blastic plasmacytoid dendritic cell neoplasm by first-line treatment and stem cell transplant. Blood Adv. 2020;4:3435–42.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Pemmaraju N, Konopleva M. Approval of tagraxofusp-erzs for blastic plasmacytoid dendritic cell neoplasm. Blood Adv. 2020;4:4020–7.
Leclerc M, Peffault de Latour R, Michallet M, Blaise D, Chevallier P, Rohrlich PS, et al. Can a reduced-intensity conditioning regimen cure blastic plasmacytoid dendritic cell neoplasm? Blood. 2017;129:1227–30.
Kaloyannidis P, Zomas A, Paterakis G, Vadikoliou C, Mallouri D, Sakkas L, et al. GVL effect in plasmacytoid DC leukemia/lymphoma. Bone marrow Transplant. 2010;45:961–2.
Ben Amor R, Hicheri Y, Pautas C, Jouault H, Kuentz M, Cordonnier C, et al. Successful non-myeloablative allogeneic HLA-identical stem cell transplantation for CD4/CD56 positive acute leukemia. Transplantation. 2007;84:1066–7.
D’Souza A, Fretham C, Lee SJ, Arora M, Brunner J, Chhabra S, et al. Current use of and trends in hematopoietic cell transplantation in the United States. Biol Blood Marrow Transplant. 2020;26:e177–e82.
Pemmaraju N, Lane AA, Sweet KL, Stein AS, Vasu S, Blum W, et al. Tagraxofusp in blastic plasmacytoid dendritic-cell neoplasm. N Engl J Med. 2019;380:1628–37.
Montero J, Stephansky J, Cai T, Griffin GK, Cabal-Hierro L, Togami K, et al. Blastic plasmacytoid dendritic cell neoplasm is dependent on BCL2 and sensitive to venetoclax. Cancer Discov. 2017;7:156–64.
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of conditioning intensity of allogeneic transplantation for acute myeloid leukemia with genomic evidence of residual disease. J Clin Oncol. 2020;38:1273–83.
Wang W, Khoury JD, Miranda RN, Jorgensen JL, Xu J, Loghavi S, et al. Immunophenotypic characterization of reactive and neoplastic plasmacytoid dendritic cells permits establishment of a 10-color flow cytometric panel for initial workup and residual disease evaluation of blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2021;106:1047–55.
Funding
This study is supported by EBMT.
Author information
Authors and Affiliations
Contributions
Conception and design: SD, PD. Collection and assembly of data: HF, AB. Data analysis: SD, P-MB, AB. Interpretation: All authors. Manuscript writing: First draft prepared by SD and PD. All authors helped with further developing the manuscript. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
PD: consultancy for AbbVie, AstraZeneca, Gilead, Janssen, Novartis, Riemser, Roche; speakers bureau for AbbVie, Gilead, Novartis, Riemser, Roche; research support from Neovii and Riemser. SD: consultancy for AbbVie, AstraZeneca, Gilead, Janssen, Novartis, Riemser, Roche; speakers bureau for AbbVie, Gilead, Novartis, Riemser, Roche; research support from Gilead and Janssen. P-MB: speakers bureau for AstraZeneca. TH: consultancy Eurocept, travel grants from Jazz, Gilead, Eurocept and Daichii. All other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bruch, PM., Dietrich, S., Finel, H. et al. Retrospective analysis of hematopoietic cell transplantation for blastic plasmacytoid dendritic cell neoplasm: conditioning intensity matters. Leukemia 37, 465–472 (2023). https://doi.org/10.1038/s41375-022-01782-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01782-z
This article is cited by
-
Ulcerating skin lesions from blastic plasmacytoid dendritic cell neoplasm responding to low-dose radiotherapy—a case report and literature review
Strahlentherapie und Onkologie (2024)
-
Thiotepa-busulfan-fludarabine-based conditioning as a promising approach prior to allogeneic hematopoietic stem cell transplantation in patients with blastic plasmacytoid dendritic cell neoplasm
Annals of Hematology (2024)