Abstract
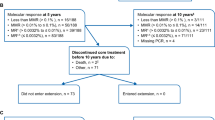
Ibrutinib has superior progression-free survival compared with bendamustine plus rituximab (BR) in older CLL patients, however, differences in treatment duration, six monthly BR cycles versus continuous ibrutinib, complicate adverse event (AE) comparisons. We introduce the AE burden score (AEsc) to compare AEs, calculated for each patient by summing over products of reporting period length and grade for each all-cause grade 1–4 AE and dividing by the length of time over which AEs are assessed. A total of 176 patients received BR and 361 ibrutinib alone or with six cycles of rituximab. At 38 months median follow-up, 64% remained on ibrutinib. Median AEsc was higher with BR versus ibrutinib in the first six cycles (7.2 versus 4.9, p < 0.0001). Within ibrutinib arms, median AEsc decreased significantly to 3.7 after six cycles (p < 0.0001). 10% and 14% of BR and ibrutinib patients discontinued treatment for AEs. In ibrutinib arms, cumulative incidence of grade 3 or higher atrial fibrillation, hypertension, and infection (AEs of clinical interest) at 12 months was 4.5%, 17.5%, and 12.8%, respectively, and increased more slowly thereafter to 7.7%, 25.4%, and 20.5% at 36 months. Analytical tools including the AEsc and cumulative incidence of AEs can help to better characterize AE burden over time. ClinicalTrials.gov identifier: NCT01886872.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Eichhorst B, Dreyling M, Robak T, Montserrat E, Hallek M. Chronic lymphocytic leukemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2011;22:vi50–4.
Eichhorst BF, Busch R, Stilgenbauer S, Stauch M, Bergmann MA, Ritgen M, et al. First-line therapy with fludarabine compared with chlorambucil does not result in a major benefit for elderly patients with advanced chronic lymphocytic leukemia. Blood.2009;114:3382–91.
Eichhorst B, Fink AM, Bahlo J, Busch R, Math D, Kovacs G. et al. First-line chemoimmunotherapy with bendamustine and rituximab versus fludarabine, cyclophosphamide, and rituximab in patients with advanced chronic lymphocytic leukaemia (CLL10): an international, open-label, randomised, phase 3, non-inferiority trial. Lancet Oncol. 2016;17:928–42.
Burger JA, Tedeschi A, Barr PM, Robak T, Owen C, Ghia P. et al. RESONATE-2 investigators. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N. Engl J Med. 2015;373:2425–37.
Woyach JA, Ruppert AS, Heerema NA, Zhao W, Booth AM, Ding W. et al. Ibrutinib regimens versus chemoimmunotherapy in older patients with untreated CLL. N. Engl J Med. 2018;379:2517–28.
Hilal T, Gea-Banacloche JC, Leis JF. Chronic lymphocytic leukemia and infection risk in the era of targeted therapies: linking mechanisms with infections. Blood Rev. 2018;32:387–99.
Barr PM, Robak T, Owen C, Tedeschi A, Bairey O, Bartlett NL. et al. Sustained efficacy and detailed clinical follow-up of first-line ibrutinib treatment in older patients with chronic lymphocytic leukemia: extended phase 3 results from RESONATE-2. Haematologica. 2018;103:1502–10.
National Cancer Institute: CTEP. Common terminology criteria for adverse events (CTCAE) Version 4.0. Bethesda, MD: National Institutes of Health; 2009.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Thanarajasingam G, Hubbard JM, Sloan JA, Grothey A. The imperative for a new approach to toxicity analysis in oncology clinical trials. J Natl Cancer Inst. 2015;107:djv216. https://doi.org/10.1093/jnci/djv216.
Carbini M, Suárez-Fariñas M, Maki RG. A method to summarize toxicity in cancer randomized cinical trials. Clin Cancer Res. 2018;24:4968–75.
Trotti A, Pajak TF, Gwede CK, Paulus R, Cooper J, Forastiere A. et al. TAME: development of a new method for summarising adverse events of cancer treatment by the Radiation Therapy Oncology Group. Lancet Oncol. 2007;8:613–24.
Lee SM, Hershman DL, Martin P, Leonard JP, Cheung YK. Toxicity burden score: a novel approach to summarize multiple toxic effects. Ann Oncol. 2012;23:537–41.
Le-Rademacher JG, Hillman S, Storrick E, Mahoney MR, Thall PF, Jatoi A. et al. Adverse event burden score – a versatile summary measure for cancer clinical trials. Cancers. 2020;12:3251.
Schuurhuizen CS, Verheul HM, Braamse AM, Buffart LM, Bloemendal HJ, Dekker J. et al. The predictive value of cumulative toxicity for quality of life in patients with metastatic colorectal cancer during first-line palliative chemotherapy. Cancer Manag Res. 2018;10:3015–21.
Sivendran S, Latif A, McBride RB, Stensland KD, Wisnivesky J, Haines L. et al. Adverse event reporting in cancer clinical trial publications. J Clin Oncol. 2014;32:83–9.
Hillman SL, Mandrekar SJ, Bot B, DeMatteo RP, Perez EA, Ballman KV. et al. Evaluation of the value of attribution in the interpretation of adverse event data: a North Central cancer treatment group and american college of surgeons oncology group investigation. J Clin Oncol. 2010;28:3002–7.
George GC, Barata PC, Campbell A, Chen A, Cortes JA, Hyman DM, et al. Improving attribution of adverse events in oncology clinical trials. Cancer Treat Rev. 2019;76:33–40.
Bercusson A, Colley T, Shah A, Warris A, Armstrong-James D. Ibrutinib blocks Btk-dependent NF-ĸB and NFAT responses in human macrophages during Aspergillus fumigatus phagocytosis. Blood. 2018;132:1985–8.
Rogers KA, Mousa L, Zhao Q, Bhat SA, Byrd JC, El Boghdadly Z. et al. Incidence of opportunistic infections during ibrutinib treatment for B-cell malignancies. Leukemia. 2019;33:2527–30.
Shanafelt TD, Wang V, Kay NE, Hanson CA, O’Brien SM, Barrientos JC. et al. Ibrutinib and rituximab provides superior clinical outcome compared to FCR in younger patients with chronic lymphocytic leukemia (CLL): extended follow-up from the E1912 trial. Blood. 2019;134:33.
Acknowledgements
Support: Research reported in this publication was supported in part by National Cancer Institute of the National Institutes of Health under Award Numbers U10CA180821, U10CA180882, and U24CA196171, (to the Alliance for Clinical Trials in Oncology), UG1CA232760, UG1CA233180, UG1CA233253, UG1CA233327, UG1CA233331, R35CA198183 (JCB), and R01CA192928 (JCB/JAW), U10CA180863 (CCTG). Also supported in part by Pharmacyclics which provided ibrutinib for the clinical trial. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Those providing support to Alliance for Clinical Trials in Oncology and Alliance Foundation Trials are found at https://acknowledgments.alliancefound.org.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors would like to disclose conflicts of interest. ASR has acted as a consultant or advisor to Telios Pharma. WD has received clinical research support from Merck. NLB has acted as a consultant or advisor to Seattle Genetics, and has received clinical research support from ADC Therapeutics, Autolus, Bristol-Myers Squibb, Celgene, Forty Seven, Genentech, Immune Design, Janssen, Kite Pharma, Merck, Millennium, Pharmacyclics, and Seattle Genetics. DMB has received honoraria from Genentech, Abbvie, Teva, TG Therapeutics, has acted as a consultant or advisor to Genentech, Abbvie, Novartis Pharma SAS, Pharmacyclics, Teva, TG Therapeutics, has had travel and accommodation expenses paid for by Abbvie, Teva, and TG Therapeutics, and has declared other relationships with Novartis Pharma SAS. SC has stock and other ownership interests in Abbvie/Pharmacyclics, has received honoraria from Janssen Oncology and Pharmacyclics, has acted as a consultant or advisor to Abbie, Adpative Biotechnologies, Astellas Pharma, AstraZeneca, BeiGene, Celgene, Genentech/Roche, Gilead Sciences, Janssen Oncology, Novartis, and Pharmacyclics, has received clinical research support from Abbvie, Acerta Pharma/AstraZeneca, Celgene, Janssen Oncology, Pharmacyclics, and Takeda, provided expert testimony for Genentech, and has had travel and accommodation expenses paid for by Abbvie, BeiGene, Celgene, Genentech, Janssen Oncology, and Pharmacyclics. JRB has received honoraria from Abbvie and Janssen, has acted as a consultant or advisor to Astellas Pharma, AstraZeneca, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Abbvie, Janssen, Pharmacyclics, Redx Pharma, Roche/Genentech, and Sun Pharma and has received clinical research support from Gilead Sciences. RAL has acted as a consultant or advisor to Novartis, Amgen, Ariad/Takeda, Astellas, Celgene/BMS, CVS/Caremark, Epizyme, and MorphoSys, and has received clinical research support from Novartis, Astellas, Celgene, Cellectis, Daiichi Sankyo, Forty Seven, Rafael Pharmaceuticals, and royalties from UpToDate. HE has acted as a consultant or advisor to Agios, Amgen, Astellas Pharma, Celgene, Daiichi Sankyo, Glycomimetics, Immunogen, Incyte, Jazz Pharmaceuticals, Macrogenics, Novartis, Pfizer, and Seattle Genetics, was on a Speakers’ Bureau for Agios, Celgene, Incyte, Jazz Pharmaceuticals, and Novartis, has received clinical research support from Abbvie, has declared other relationships with Celgene and Glycomimetics, and has declared uncompensated relationships with Daiichi Sankyo. ML has acted as a consultant or advisor to Newlink Genetics and Sanofi, and has received clinical research support from Abbvie, Abbvie/Genentech, Actinium Pharmaceuticals, Amgen, Astellas Pharma, Pluristem Therapeutics, and Tolero Pharmaceuticals. JSA has acted as a consultant or advisor to Abbvie, Allogene, Bayer, Bristol-Myers Squibb, Celgene, EMD Serono, Genentech, Gilead Sciences, Janssen, Juno Therapeutics, Karyopharm Therapeutics, Kite Pharma, Merck, MorphoSys, Novartis, and Verastem, and has received clinical research support from AI Therapeutics, Celgene, and Seattle Genetics. RMS has received honoraria from DAVA Pharmaceuticals, Medscape, Prime Oncology, and Research to Practice, has acted as a consultant or advisor to Abbvie, Actinium Pharmaceuticals, Ageios, Amgen, argenx, Arog, Astellas Pharma, AstraZeneca, Biolinerx, Celgene, Celgene/Jazz, Cornerstone Pharmaceuticals, Daiichi Sankyo, Gemoab, Macrogenics, Novartis, Otsuka, Pfizer, Roche/Genentech, Stemline Therapeutics, Syntrix, Takeda, Trovagene, and has received clinical research support from Abbvie/Genentech, Agios, and Novartis. JCB has acted as a consultant or advisor to Acerta Pharma, Genentech, Jazz Pharmaceuticals, and Pharmacyclics, and has received clinical research support from Acerta Pharma, Genentech, Janssen, and Pharmacyclics. SJM has acted as a consultant or advisor to Pfizer and Pique and has declared other relationships with BioGene. JAW has acted as a consultant or advisor to ArQule, AstraZeneca, Janssen, and Pharmacyclics, and has received clinical research support from Abbvie, Janssen, Karyopharm Therapeutics, Loxo, MorphoSys, and Verastem. All other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ruppert, A.S., Booth, A.M., Ding, W. et al. Adverse event burden in older patients with CLL receiving bendamustine plus rituximab or ibrutinib regimens: Alliance A041202. Leukemia 35, 2854–2861 (2021). https://doi.org/10.1038/s41375-021-01342-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-021-01342-x