Abstract
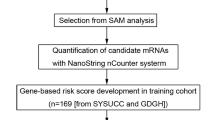
New prognostic factors are needed to establish indications for haematopoietic stem cell transplantation (HSCT) in first complete remission (CR1) for T-cell lymphoblastic lymphoma (T-LBL) patients. We used microarray to compare T-LBL tissue samples (n = 75) and fetal thymus tissues (n = 20), and identified 35 differentially expressed miRNAs. Using 107 subjects as the training group, we developed a five-miRNA-based classifier to predict patient survival with LASSO Cox regression: lower risk was associated with better prognosis (disease-free survival (DFS): hazard ratio (HR) 4.548, 95% CI 2.433–8.499, p < 0.001; overall survival (OS): HR 5.030, 95% CI 2.407–10.513, p < 0.001). This classifier displayed good performance in the internal testing set (n = 106) and the independent external set (n = 304). High risk was associated with more favorable response to HSCT (DFS: HR 1.675, 95% CI 1.127–2.488, p = 0.011; OS: HR 1.602, 95% CI 1.055–2.433, p = 0.027). When combined with ECOG-PS and/or NOTCH1/FBXW7 status, this classifier had even better prognostic performance in patients receiving HSCT (DFS: HR 2.088, 95% CI 1.290–3.379, p = 0.003; OS: HR 1.996, 95% CI 1.203–3.311, p = 0.007). The five-miRNA classifier may be a useful prognostic biomarker for T-LBL adults, and could identify subjects who could benefit from HSCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The key raw data have been uploaded onto the Research Data Deposit public platform (RDD), with the approval RDD number of RDDA2018000588. The microarray data have been deposited online under accession number GSE113749.
References
Portell CA, Sweetenham JW. Adult lymphoblastic lymphoma. Cancer J. 2012;18:432–8.
Raetz EA, Perkins SL, Bhojwani D, Smock K, Philip M, Carroll WL, et al. Gene expression profiling reveals intrinsic differences between T-cell acute lymphoblastic leukemia and T-cell lymphoblastic lymphoma. Pediatr Blood Cancer. 2006;47:130–40.
Basso K, Mussolin L, Lettieri A, Brahmachary M, Lim WK, Califano A, et al. T-cell lymphoblastic lymphoma shows differences and similarities with T-cell acute lymphoblastic leukemia by genomic and gene expression analyses. Genes Chromosomes Cancer. 2011;50:1063–75.
Burkhardt B, Mueller S, Khanam T, Perkins SL. Current status and future directions of T-lymphoblastic lymphoma in children and adolescents. Br J Haematol. 2016;173:545–59.
Sweetenham JW. Treatment of lymphoblastic lymphoma in adults. Oncology. 2009;23:1015–20.
Cortelazzo S, Ponzoni M, Ferreri AJ, Hoelzer D. Lymphoblastic lymphoma. Crit Rev Oncol Hematol. 2011;79:330–43.
Hoelzer D, Gokbuget N, Digel W, Faak T, Kneba M, Reutzel R, et al. Outcome of adult patients with T-lymphoblastic lymphoma treated according to protocols for acute lymphoblastic leukemia. Blood. 2002;99:4379–85.
Thomas DA, O’Brien S, Cortes J, Giles FJ, Faderl S, Verstovsek S, et al. Outcome with the hyper-CVAD regimens in lymphoblastic lymphoma. Blood. 2004;104:1624–30.
Lepretre S, Touzart A, Vermeulin T, Picquenot JM, Tanguy-Schmidt A, Salles G, et al. Pediatric-like acute lymphoblastic leukemia therapy in adults with lymphoblastic lymphoma: the GRAALL-LYSA LL03 study. J Clin Oncol. 2016;34:572–80.
Aljurf M, Zaidi SZ. Chemotherapy and hematopoietic stem cell transplantation for adult T-cell lymphoblastic lymphoma: current status and controversies. Biol Blood Marrow Transplant. 2005;11:739–54.
Network. NCC. (NCCN) Clinical practice guidelines in oncology. In: Acute Lymphoblastic Leukemia, Version 1. 2018. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 12 Mar 2018.
Song KW, Barnett MJ, Gascoyne RD, Chhanabhai M, Forrest DL, Hogge DE, et al. Primary therapy for adults with T-cell lymphoblastic lymphoma with hematopoietic stem-cell transplantation results in favorable outcomes. Ann Oncol. 2007;18:535–40.
Gu Y, Pan Y, Meng B, Guan B, Fu K, Sun B, et al. High levels of bcl-2 protein expression do not correlate with genetic abnormalities but predict worse prognosis in patients with lymphoblastic lymphoma. Tumour Biol. 2013;34:1441–50.
Tilak TV, Raina V, Kumar L, Sharma A, Sharma MC, Vishnubhatla S, et al. Superior vena cava syndrome and poor performance status at presentation affect survival in mediastinal T-lymphoblastic lymphoma—a single institute experience from India. Ann Hematol. 2013;92:917–23.
Callens C, Baleydier F, Lengline E, Ben Abdelali R, Petit A, Villarese P, et al. Clinical impact of NOTCH1 and/or FBXW7 mutations, FLASH deletion, and TCR status in pediatric T-cell lymphoblastic lymphoma. J Clin Oncol. 2012;30:1966–73.
Hoelzer D, Gokbuget N. Treatment of lymphoblastic lymphoma in adults. Best Pract Res Clin Haematol. 2002;15:713–28.
Lujambio A, Lowe SW. The microcosmos of cancer. Nature. 2012;482:347–55.
Qian D, Chen K, Deng H, Rao H, Huang H, Liao Y, et al. MicroRNA-374b suppresses proliferation and promotes apoptosis in T-cell lymphoblastic lymphoma by repressing AKT1 and Wnt-16. Clin Cancer Res. 2015;21:4881–91.
Gonzalez-Gugel E, Villa-Morales M, Santos J, Bueno MJ, Malumbres M, Rodriguez-Pinilla SM, et al. Down-regulation of specific miRNAs enhances the expression of the gene Smoothened and contributes to T-cell lymphoblastic lymphoma development. Carcinogenesis. 2013;34:902–8.
Xi Y, Li J, Zhang P, Bai W, Gao N, Bai W, et al. Upregulation of miRNA-17 and miRNA-19 is associated with unfavorable prognosis in patients with T-cell lymphoblastic lymphoma. Exp Mol Pathol. 2015;99:297–302.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:937–51.
Burkhardt B, Oschlies I, Klapper W, Zimmermann M, Woessmann W, Meinhardt A, et al. Non-Hodgkin’s lymphoma in adolescents: experiences in 378 adolescent NHL patients treated according to pediatric NHL-BFM protocols. Leukemia. 2011;25:153–60.
Kantarjian HM, O’Brien S, Smith TL, Cortes J, Giles FJ, Beran M, et al. Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol. 2000;18:547–61.
Asnafi V, Buzyn A, Le Noir S, Baleydier F, Simon A, Beldjord K, et al. NOTCH1/FBXW7 mutation identifies a large subgroup with favorable outcome in adult T-cell acute lymphoblastic leukemia (T-ALL): a Group for Research on Adult Acute Lymphoblastic Leukemia (GRAALL) study. Blood. 2009;113:3918–24.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86.
Levine JE, Harris RE, Loberiza FR Jr., Armitage JO, Vose JM, et al. A comparison of allogeneic and autologous bone marrow transplantation for lymphoblastic lymphoma. Blood. 2003;101:2476–82.
Sweetenham JW, Santini G, Qian W, Guelfi M, Schmitz N, Simnett S, et al. High-dose therapy and autologous stem-cell transplantation versus conventional-dose consolidation/maintenance therapy as postremission therapy for adult patients with lymphoblastic lymphoma: results of a randomized trial of the European Group for Blood and Marrow Transplantation and the United Kingdom Lymphoma Group. J Clin Oncol. 2001;19:2927–36.
Fabbri M, Paone A, Calore F, Galli R, Gaudio E, Santhanam R, et al. MicroRNAs bind to Toll-like receptors to induce prometastatic inflammatory response. Proc Natl Acad Sci USA. 2012;109:E2110–2116.
Chen J, Jiang CC, Jin L, Zhang XD. Regulation of PD-L1: a novel role of pro-survival signalling in cancer. Ann Oncol. 2016;27:409–16.
Guraya S. Prognostic significance of circulating microRNA-21 expression in esophageal, pancreatic and colorectal cancers; a systematic review and meta-analysis. Int J Surg. 2018;60:41–47.
Wang WZ, Lin XH, Pu QH, Liu MY, Li L, Wu LR, et al. Targeting miR-21 sensitizes Ph + ALL Sup-b15 cells to imatinib-induced apoptosis through upregulation of PTEN. Biochem Biophys Res Commun. 2014;454:423–8.
Junker F, Chabloz A, Koch U, Radtke F. Dicer1 imparts essential survival cues in Notch-driven T-ALL via miR-21-mediated tumor suppressor Pdcd4 repression. Blood. 2015;126:993–1004.
Mavrakis KJ, Van Der Meulen J, Wolfe AL, Liu X, Mets E, Taghon T, et al. A cooperative microRNA-tumor suppressor gene network in acute T-cell lymphoblastic leukemia (T-ALL). Nat Genet. 2011;43:673–8.
Mavrakis KJ, Wolfe AL, Oricchio E, Palomero T, de Keersmaecker K, McJunkin K, et al. Genome-wide RNA-mediated interference screen identifies miR-19 targets in Notch-induced T-cell acute lymphoblastic leukaemia. Nat Cell Biol. 2010;12:372–9.
Di Lisio L, Gomez-Lopez G, Sanchez-Beato M, Gomez-Abad C, Rodriguez ME, Villuendas R, et al. Mantle cell lymphoma: transcriptional regulation by microRNAs. Leukemia. 2010;24:1335–42.
Lin Y, Li D, Liang Q, Liu S, Zuo X, Li L, et al. miR-638 regulates differentiation and proliferation in leukemic cells by targeting cyclin-dependent kinase 2. J Biol Chem. 2015;290:1818–28.
Acknowledgements
We thank Junhang Luo (First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China) for manuscript consultation, and Wenjun He (Department of Medical Statistics and Epidemiology, School of Public Health, Sun Yat-sen University, Guangzhou, China) for supporting part of the data extraction and processing. This work was supported by grants from the National Natural Science Foundation of China (81672686, 81603137); Natural Science Foundation of Guangdong Province, China (2015A030313020); Sister Institution Net-work Fund of the MD Anderson Cancer Center; National Key R&D Program of China (2017YFC1309001, 2016YFC1302305).
Author information
Authors and Affiliations
Contributions
Q-QC and DX designed the study. X-PT, W-JH, H-QH, Y-HL, XZ, T-YL, H-LR, ML, FL, FZ, L-YZ, LL, X-LL, JL, BL, Z-HL, Q-LT, QL, C-KS, Q-LZ, R-FC, QS, KR, XG, X-NL, KY, Y-RS, X-DL, WD, WS, CS, HL, Z-GZ, JR, Q-NG, YZ, X-LM, YZ, C-LH, Y-RJ, YZ, LW, H-YG and Z-JX obtained and assembled data. X-PT, W-JH, DX, Q-QC, and H-YW analyzed and interpreted the data. X-PT, W-JH, XD, and Q-QC wrote the manuscript. X-PT, M-YZ, W-JH did the statistical analysis. All authors reviewed the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tian, XP., Huang, WJ., Huang, HQ. et al. Prognostic and predictive value of a microRNA signature in adults with T-cell lymphoblastic lymphoma. Leukemia 33, 2454–2465 (2019). https://doi.org/10.1038/s41375-019-0466-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0466-0
This article is cited by
-
The β-catenin-LINC00183-miR-371b-5p-Smad2/LEF1 axis promotes adult T-cell lymphoblastic lymphoma progression and chemoresistance
Journal of Experimental & Clinical Cancer Research (2023)
-
Lymphoblastic Lymphoma: a Concise Review
Current Oncology Reports (2022)
-
A nomogram prognostic index for risk-stratification in diffuse large B-cell lymphoma in the rituximab era: a multi-institutional cohort study
British Journal of Cancer (2021)
-
Epigenetic signature predicts overall survival clear cell renal cell carcinoma
Cancer Cell International (2020)
-
Hematopoietic stem cell transplantation for adults with T-cell lymphoblastic lymphoma: can we successfully step into the era of precision medicine?
Leukemia (2020)