Abstract
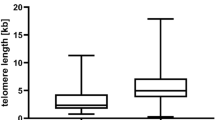
Telomere length in chronic lymphocytic leukemia (CLL) has been shown to be of prognostic importance, but the analyses have largely been executed on heterogeneous patient cohorts outside of clinical trials. In the present study, we performed a comprehensive analysis of telomere length associations in the well characterized CLL8 trial (n = 620) of the German CLL study group, with validation in a representative cohort of the CLL4 trial (n = 293). Absolute telomere length was analyzed using quantitative-PCR. Apart from identifying associations of short telomere length with adverse prognostic factors and survival, the study identified cases with 17p- and 11q- associated with TP53 and ATM loss, respectively, to have the shortest telomeres, even when these aberrations were present in small subclones. Thus, telomere shortening may precede acquisition of the high-risk aberrations, contributing to disease evolution. In line with this, telomere shortening was associated with an increase in genomic complexity as well as clonal evolution, highlighting its importance as a biomarker especially in monitoring disease progression in non-high-risk CLL.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Kipps TJ, Stevenson FK, Wu CJ, Croce CM, Packham G, Wierda WG, et al. Chronic lymphocytic leukaemia. Nat Rev Dis Prim. 2017;3:16096.
The International CLL-IPI working group. An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): a meta-analysis of individual patient data. Lancet Oncol. 2016;17:779–90.
Bechter OE, Eisterer W, Pall G, Hilbe W, Kühr T, Thaler J. Telomere length and telomerase activity predict survival in patients with B cell chronic lymphocytic leukemia. Cancer Res. 1998;58:4918–22.
Damle RN, Batliwalla FM, Ghiotto F, Valetto A, Albesiano E, Sison C, et al. Telomere length and telomerase activity delineate distinctive replicative features of the B-CLL subgroups defined by immunoglobulin V gene mutations. Blood. 2004;103:375–82.
Grabowski P, Hultdin M, Karlsson K, Tobin G, Aleskog A, Thunberg U, et al. Telomere length as a prognostic parameter in chronic lymphocytic leukemia with special reference to VH gene mutation status. Blood. 2005;105:4807–12.
Ricca I, Rocci A, Drandi D, Francese R, Compagno M, Lobetti Bodoni C, et al. Telomere length identifies two different prognostic subgroups among VH-unmutated B-cell chronic lymphocytic leukemia patients. Leukemia. 2007;21:697–705.
Roos G, Kröber A, Grabowski P, Kienle D, Bühler A, Döhner H, et al. Short telomeres are associated with genetic complexity, high-risk genomic aberrations, and short survival in chronic lymphocytic leukemia. Blood. 2008;111:2246–52.
Rampazzo E, Bonaldi L, Trentin L, Visco C, Keppel S, Giunco S, et al. Telomere length and telomerase levels delineate subgroups of B-cell chronic lymphocytic leukemia with different biological characteristics and clinical outcomes. Haematologica. 2012;97:56–63.
Strefford JC, Kadalayil L, Forster J, Rose-Zerilli MJJ, Parker A, Lin TT, et al. Telomere length predicts progression and overall survival in chronic lymphocytic leukemia: data from the UK LRF CLL4 trial. Leukemia. 2015;29:2411–4.
Blackburn EH, Greider CW, Szostak JW. Telomeres and telomerase: the path from maize, tetrahymena and yeast to human cancer and aging. Nat Med. 2006;12:1133–8.
Calado RT, Young NS. Telomere diseases. N Engl J Med. 2009;361:2353–65.
Xu L, Li S, Stohr BA. The role of telomere biology in cancer. Annu Rev Pathol. 2013;8:49–78.
Zhang C, Doherty JA, Burgess S, Hung RJ, Lindström S, Kraft P, et al. Genetic determinants of telomere length and risk of common cancers: a Mendelian randomization study. Hum Mol Genet. 2015;24:5356–66.
Boardman LA, Litzelman K, Seo S, Johnson RA, Vanderboom RJ, Kimmel GW, et al. The association of telomere length with colorectal cancer differs by the age of cancer onset. Clin Transl Gastroenterol. 2014;5:e52.
Seguí N, Guinó E, Pineda M, Navarro M, Bellido F, Lázaro C, et al. Longer telomeres are associated with cancer risk in MMR-proficient hereditary non-polyposis colorectal cancer. PLoS ONE. 2014;9:e86063.
Baichoo E, Boardman LA. Toward a molecular classification of colorectal cancer: the role of telomere length. Front Oncol. 2014;4:158.
Wang H, Wang Y, Kota KK, Kallakury B, Mikhail NN, Sayed D, et al. Strong association between long and heterogeneous telomere length in blood lymphocytes and bladder cancer risk in Egyptian. Carcinogenesis. 2015;36:1284–90.
Du J, Zhu X, Xie C, Dai N, Gu Y, Zhu M, et al. Telomere length, genetic variants and gastric cancer risk in a Chinese population. Carcinogenesis. 2015;36:963–70.
Svenson U, Roos G. Telomere length as a biological marker in malignancy. Biochim Biophys Acta. 2009;1792:317–23.
Xu Y, Goldkorn A. Telomere and telomerase therapeutics in cancer. Genes (Basel). 2016;7:pii: E22.
Fischer K, Bahlo J, Fink AM, Goede V, Herling CD, Cramer P, et al. Long-term remissions after FCR chemoimmunotherapy in previously untreated patients with CLL: updated results of the CLL8 trial. Blood. 2016;127:208–15.
Eichhorst BF, Busch R, Hopfinger G, Pasold R, Hensel M, Steinbrecher C, et al. Fludarabine plus cyclophosphamide versus fludarabine alone in first-line therapy of younger patients with chronic lymphocytic leukemia. Blood. 2006;107:885–91.
Hallek M, Fischer K, Fingerle-Rowson G, Fink AM, Busch R, Mayer J, et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 2010;376:1164–74.
Cawthon RM. Telomere measurement by quantitative PCR. Nucleic Acids Res. 2002;30:e47.
O’Callaghan N, Dhillon V, Thomas P, Fenech M. A quantitative real-time PCR method for absolute telomere length. Biotechniques. 2008;44:807–9.
Kruk PA, Rampino NJ, Bohr VA. DNA damage and repair in telomeres: relation to aging. Proc Natl Acad Sci USA. 1995;92:258–62.
Döhner H, Stilgenbauer S, Benner A, Leupolt E, Kröber A, Bullinger L, et al. Genomic aberrations and survival in chronic lymphocytic leukemia. N Engl J Med. 2000;343:1910–6.
Kröber A, Seiler T, Benner A, Bullinger L, Brückle E, Lichter P, et al. V(H) mutation status, CD38 expression level, genomic aberrations, and survival in chronic lymphocytic leukemia. Blood. 2002;100:1410–6.
Stilgenbauer S, Schnaiter A, Paschka P, Zenz T, Rossi M, Döhner K, et al. Gene mutations and treatment outcome in chronic lymphocytic leukemia: results from the CLL8 trial. Blood. 2014;123:3247–54.
Edelmann J, Holzmann K, Miller F, Winkler D, Bühler A, Zenz T, et al. High-resolution genomic profiling of chronic lymphocytic leukemia reveals new recurrent genomic alterations. Blood. 2012;120:4783–94.
Landau DA, Tausch E, Taylor-Weiner AN, Stewart C, Reiter JG, Bahlo J, et al. Mutations driving CLL and their evolution in progression and relapse. Nature. 2015;526:525–30.
Spivak IM, Mikhelson VM, Spivak DL. Telomere length, telomerase activity, stress, and aging. Adv Gerontol. 2016;6:29–35.
Röth A, de Beer D, Nückel H, Sellmann L, Dührsen U, Dürig J, et al. Significantly shorter telomeres in T-cells of patients with ZAP-70+ /CD38+ chronic lymphocytic leukaemia. Br J Haematol. 2008;143:383–6.
Seifert M, Sellmann L, Bloehdorn J, Wein F, Stilgenbauer S, Dürig J, et al. Cellular origin and pathophysiology of chronic lymphocytic leukemia. J Exp Med. 2012;209:2183–98.
Weng NP, Granger L, Hodes RJ. Telomere lengthening and telomerase activation during human B cell differentiation. Proc Natl Acad Sci USA. 1997;94:10827–32.
Jeromin S, Weissmann S, Dicker F, Kern W, Schnittger S, Kohlmann A, et al. IGHV mutation status does not add prognostic information in the background of mutations in TP53 and SF3B1, and deletions of 17p and 11q, which are independent adverse prognostic parameters In CLL. Blood. 2013;122:4110.
Herbig U, Jobling WA, Chen BPC, Chen DJ, Sedivy JM. Telomere shortening triggers senescence of human cells through a pathway involving ATM, p53, and p21(CIP1), but not p16(INK4a). Mol Cell. 2004;14:501–13.
Stilgenbauer S. Prognostic markers and standard management of chronic lymphocytic leukemia. Hematol Am Soc Hematol Educ Program. 2015;2015:368–77.
Thompson PA, O’Brien SM, Wierda WG, Ferrajoli A, Stingo F, Smith SC, et al. Complex karyotype is a stronger predictor than del(17p) for an inferior outcome in relapsed or refractory chronic lymphocytic leukemia patients treated with ibrutinib-based regimens. Cancer. 2015;121:3612–21.
Acknowledgements
We thank all patients and their physicians for CLL4 and CLL8 trial participation and donation of samples; Myriam Mendila, Nancy Valente, Stephan Zurfluh, and Jamie Wingate for their support in conception and conduct of the CLL8 trial. This work was supported by the Else Kröner-Fresenius-Stiftung (2010_Kolleg24), EC (01KT1601, FIRE CLL), BMBF (031L0076C PRECISe), and Deutsche Forschungsgemeinschaft (SFB 1074 projects B1, B2). Genetic analyses in CLL8 were supported by F. Hoffmann-La Roche.
Author contributions
B.M.C.J. designed and performed experiments, analyzed and interpreted data and wrote the manuscript; E.T., D.A.L., A.N.T.-W., and J.B. performed experiments, interpreted data and edited the manuscript; J.B. and S.R. analyzed the data and edited the manuscript; S.S. conceived study, designed experiments, interpreted data and wrote the manuscript. The remaining authors collected, analyzed, and interpreted data, and contributed to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.K.W. and G.F.-R.: employment at F. Hoffmann-La Roche; C.W.: consultancy, membership in board of directors or advisory committees, research funding from Hoffmann-La Roche; K.F.: travel grants from Roche; M.K., U.J., M.H., and S.S.: consultancy, honoraria, and research funding from Roche. The remaining authors declare no conflict of interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jebaraj, B.M.C., Tausch, E., Landau, D.A. et al. Short telomeres are associated with inferior outcome, genomic complexity, and clonal evolution in chronic lymphocytic leukemia. Leukemia 33, 2183–2194 (2019). https://doi.org/10.1038/s41375-019-0446-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0446-4
This article is cited by
-
Imetelstat-mediated alterations in fatty acid metabolism to induce ferroptosis as a therapeutic strategy for acute myeloid leukemia
Nature Cancer (2023)
-
Evolution of TP53 abnormalities during CLL disease course is associated with telomere length changes
BMC Cancer (2022)
-
Combined analysis of IGHV mutations, telomere length and CD49d identifies long-term progression-free survivors in TP53 wild-type CLL treated with FCR-based therapies
Leukemia (2022)
-
The combination of complex karyotype subtypes and IGHV mutational status identifies new prognostic and predictive groups in chronic lymphocytic leukaemia
British Journal of Cancer (2019)