Abstract
Objective
To compare the cognitive, language and motor scores of infants with severe BPD exposed to postnatal corticosteroids (PCS) and had early (ET), late (LT) or no tracheostomy (NT).
Methods
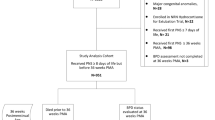
Retrospective study was designed to compare the developmental outcomes of 71 infants born between 2010 and 2017 with severe BPD exposed to PCS and had ET (≤122 days), LT (>122 days), or NT.
Results
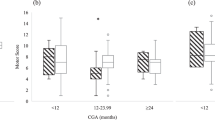
Cognitive scores were lower in LT versus NT and ET (p = 0.050); motor scores were worse in LT versus NT and ET (p = 0.004). Dexamethasone use was higher in LT versus NT and ET (p = 0.040). Adjusted for PCS, odds for major cognitive impairment were 90% less in ET versus LT. Trend for improved language and motor outcomes was seen in ET versus LT.
Conclusion
Infants with severe BPD exposed to PCS and had ET had significantly better cognitive, and trend toward improved language and motor outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med. 2017;376:617–28.
Murthy K, Porta NFM, Lagatta JM, Zaniletti I, Truog WE, Grover TR, et al. Inter-center variation in death or tracheostomy placement in infants with severe bronchopulmonary dysplasia. J Perinatol. 2017;37:723–7.
Guaman MC, Pishevar N, Abman SH, Keszler M, Truog WE, Panitch H, et al. Invasive mechanical ventilation at 36 weeks post-menstrual age, adverse outcomes with a comparison of recent definitions of bronchopulmonary dysplasia. J Perinatol. 2021;41:1936–42.
DeMauro SB. Neurodevelopmental outcomes of infants with bronchopulmonary dysplasia. Pediatr Pulmonol. 2021;56:3509–17.
Gou X, Yang L, Pan L, Xiao D. Association between bronchopulmonary dysplasia and cerebral palsy in children: a meta-analysis. BMJ Open. 2018;8:e020735.
Twilhaar ES, Wade RM, De Kieviet JF, Van Goudoever JB, Van Elburg RM, Oosterlaan J. Cognitive outcomes of children born extremely or very preterm since the 1990s and associated risk factors: a meta-analysis and meta-regression. JAMA Pediatr. 2018;172:361–7.
Overman AE, Liu M, Kurachek SC, Shreve MR, Maynard RC, Mammel MC, et al. Tracheostomy for infants requiring prolonged mechanical ventilation: 10 years’ experience. Pediatrics. 2013;131:e1491–6.
Luo J, Shepard S, Nilan K, Wood A, Monk HM, Jensen EA, et al. Improved growth and developmental activity post tracheostomy in preterm infants with severe BPD. Pediatr Pulmonol. 2018;53:1237–44.
DeMauro SB, D’Agostino JA, Bann C, Bernbaum J, Gerdes M, Bell EF, et al. Developmental outcomes of very preterm infants with tracheostomies. J Pediatr. 2014;164:1303–10.e2.
Annesi CA, Levin JC, Litt JS, Sheils CA, Hayden LP. Long-term respiratory and developmental outcomes in children with bronchopulmonary dysplasia and history of tracheostomy. J Perinatol. 2021;41:2645–50.
Cammack B, Noel-MacDonnell J, Cuna A, Manimtim W. Impact of tracheostomy on language and cognitive development in infants with severe bronchopulmonary dysplasia. J Perinatol. 2020;40:299–305.
Filippone M, Nardo D, Bonadies L, Salvadori S, Baraldi E. Update on postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Am J Perinatol. 2019;36:S58–62.
Yeh TF, Lin YJ, Lin HC, Huang CC, Hsieh WS, Lin CH, et al. Outcomes at school age after postnatal dexamethasone therapy for lung disease of prematurity. N Engl J Med. 2004;350:1304–13.
Luttikhuizen dos Santos ES, de Kieviet JF, Königs M, van Elburg RM, Oosterlaan J. Predictive value of the Bayley scales of infant development on development of very preterm/very low birth weight children: a meta-analysis. Early Hum Dev. 2013;89:487–96.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Akangire G, Lachica C, Noel-MacDonnell J, Begley A, Sampath V, Truog W, et al. Outcomes of infants with severe bronchopulmonary dysplasia who received tracheostomy and home ventilation. Pediatr Pulmonol. 2023;58:753–62.
Akangire G, Taylor JB, McAnany S, Noel-MacDonnell J, Lachica C, Sampath V, et al. Respiratory, growth, and survival outcomes of infants with tracheostomy and ventilator dependence. Pediatr Res. 2021;90:381–9.
House M, Nathan A, Bhuiyan MAN, Ahlfeld SK. Morbidity and respiratory outcomes in infants requiring tracheostomy for severe bronchopulmonary dysplasia. Pediatr Pulmonol. 2021;56:2589–96.
Hansen TP, Noel-MacDonnell J, Kuckelman S, Norberg M, Truog W, Manimtim W. A multidisciplinary chronic lung disease team in a neonatal intensive care unit is associated with increased survival to discharge of infants with tracheostomy. J Perinatol. 2021;41:1963–71.
Mandy G, Malkar M, Welty SE, Brown R, Shepherd E, Gardner W, et al. Tracheostomy placement in infants with bronchopulmonary dysplasia: safety and outcomes. Pediatr Pulmonol. 2013;48:245–9.
Upadhyay K, Vallarino DA, Talati AJ. Outcomes of neonates with tracheostomy secondary to bronchopulmonary dysplasia. BMC Pediatr. 2020;20:414.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J Pediatr. 2014;165:1258–60.
Puia-Dumitrescu M, Wood TR, Comstock BA, Law JB, German K, Perez KM, et al. Dexamethasone, prednisolone, and methylprednisolone use and 2-year neurodevelopmental outcomes in extremely preterm infants. JAMA Netw Open. 2022;5:e221947.
Ramaswamy VV, Bandyopadhyay T, Nanda D, Bandiya P, Ahmed J, Garg A, et al. Assessment of postnatal corticosteroids for the prevention of bronchopulmonary dysplasia in preterm neonates: a systematic review and network meta-analysis. JAMA Pediatr. 2021;175:e206826.
Harmon HM, Jensen EA, Tan S, Chaudhary AS, Slaughter JL, Bell EF, et al. Timing of postnatal steroids for bronchopulmonary dysplasia: association with pulmonary and neurodevelopmental outcomes. J Perinatol. 2020;40:616–27.
Watterberg KL, Walsh MC, Li L, Chawla S, D’Angio CT, Goldberg RN, et al. Hydrocortisone to improve survival without bronchopulmonary dysplasia. N Engl J Med. 2022;386:1121–31.
Linafelter A, Cuna A, Liu C, Quigley A, Truog WE, Sampath V, et al. Extended course of prednisolone in infants with severe bronchopulmonary dysplasia. Early Hum Dev. 2019;136:1–6.
Liviskie C, Vesoulis Z, Zeller B, Rao R, McPherson C. Respiratory effects of prolonged prednisolone use in infants with evolving and established bronchopulmonary dysplasia. Early Hum Dev. 2021;156:105344.
Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, Kirpalani H, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. an evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Donda K, Agyemang CO, Adjetey NA, Agyekum A, Princewill N, Ayensu M, et al. Tracheostomy trends in preterm infants with bronchopulmonary dysplasia in the United States: 2008-2017. Pediatr Pulmonol. 2021;56:1008–17.
Acknowledgements
The authors thank the Medical Writing Center at Children’s Mercy Kansas City for their help in editing the manuscript.
Author information
Authors and Affiliations
Contributions
AT, GA and WM conceptualized and designed the study. AT collected the data. AT, GA, TG, JN and WM analyzed the data. AT wrote the first draft. GA, JN, TG and WM revised the manuscript. All authors approved the final manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taha, A., Akangire, G., Noel-Macdonnell, J. et al. The impact of early tracheostomy on neurodevelopmental outcomes of infants with severe bronchopulmonary dysplasia exposed to postnatal corticosteroids. J Perinatol (2023). https://doi.org/10.1038/s41372-023-01864-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-023-01864-5