Abstract
Objective
Initiatives, “Every Newborn Action Plans” and “Sustainable Developmental Goals,” are profoundly shaping global infant mortality trends. Concurrently, professional organizations recommended curricula to prevent extreme hyperbilirubinemia (EHB) sequelae. Therefore we assessed if these efforts have successfully decreased EHB-related mortality over time.
Study Design
We used the Global Burden of Diseases 2019 database to determine neonatal and infant mortality and the burden of kernicterus from 1990–2019.
Results
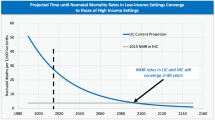
Globally, kernicterus accounted for 2.8 million infant deaths and trended downwards significantly from 1990 to 2019. By 2019, kernicterus-related mortality was 4 and 293 per million livebirths in high (HICs) and low income countries (LICs), respectively. 82% of deaths occurred in LICs and lower-middle income-countries. Average declines of mortality rates were 6.2% and 3.0% for HICs and LICs, respectively.
Conclusions
Kernicterus-related mortality has been effectively reduced to <5 per million in HICs. Skills and knowledge transfer can potentially transform frontline services to bridge discordant kernicteric outcomes worldwide.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study will be available upon requests to the corresponding author. GBD 2019 database is open to public via the Global Health Data Exchange (GHDx) (http://ghdx.healthdata.org). which is supported by the Institute for Health Metrics and Evaluation (IHME), University of Washington, USA.
Change history
21 February 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41372-024-01903-9
References
Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, et al. Neonatal hyperbilirubinemia, and Rhesus disease of the newborn: incidence and impairment estimate for 2010 at regional and global levels. Pediatr Res. 2013;74:86–100.
Johnson L, Bhutani VK, Karp K, Sivieri EM, Shapiro SM. Clinical report from the pilot USA Kernicterus Registry (1992 to 2004). J Perinatol. 2009;29:S25–45.
Johnson LH, Bhutani VK, Brown AK. System-based approach to management of neonatal jaundice and prevention of kernicterus. J Pediatr. 2002;140:396–403.
American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.
American Academy of Pediatrics. Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Practice parameter: management of hyperbilirubinemia in the healthy term newborn. Pediatrics. 1994;94:558–65.
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Stark AR, Watchko JF. Hyperbilirubinemia in the newborn infant > or =35 weeks’ gestation: an update with clarifications. Pediatrics. 2009;124:1193–8.
National Collaborating Centre for Women’s and Children’s Health. Neonatal jaundice. NICE, London 2010. http://guidance.nice.org.uk/CG98.
Rennie J, Burman-Roy S, Murphy MS, Guideline Development Group. Neonatal jaundice: summary of NICE guidance. BMJ. 2010;340:c2409.
Ip S, Chung M, Kulig J, O’Brien R, Sege R, Glicken S, et al. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004;114:e130–53.
Bratlid D, Nakstad B, Hansen TWR. National guidelines for treatment of jaundice in the newborn. Acta Paediatr. 2011;100:499–505.
Slusher TM, Zipursky A, Bhutani VK. A global need for affordable neonatal jaundice technologies. Semin Perinatol. 2011;35:185–91.
Bhutani VK, Maisels MJ, Stark AR, Buonocore G, Expert Committee for Severe Neonatal Hyperbilirubinemia, European Society for Pediatric Research. et al. Management of jaundice and prevention of severe neonatal hyperbilirubinemia in infants >or = 35 weeks gestation. Neonatology. 2008;94:63–7.
Kaplan M, Merlob P, Regev R. Israel guidelines for the management of neonatal hyperbilirubinemia and prevention of kernicterus. J Perinatol. 2008;28:389–97.
Hansen TWR, Maisels MJ, Ebbesen F, Vreman HJ, Stevenson DK, Wong RJ, et al. Sixty years of phototherapy for neonatal jaundice – from serendipitous observation to standardized treatment and rescue for millions. J Perinatol. 2020;40:180–93.
Olusanya BO, Kaplan M, Hansen TWR. Neonatal hyperbilirubinemia: a global perspective. Lancet Child Adolesc Health. 2018;2:610–20.
Ebbesen F. Recurrence of kernicterus in term and near-term infants in Denmark. Acta Paediatr. 2000;89:1213–7.
Iskander I, Gamaleldin R, Kabbani M. Root causes for late presentation of severe neonatal hyperbilirubinaemia in Egypt. East Mediterr Health J. 2012;18:882–7.
Olusanya BO, Ogunlesi TA, Kumar P, Boo NY, Iskander IF, de Almeida MF, et al. Management of late-preterm and term infants with hyperbilirubinaemia in resource-constrained settings. BMC Pediatr. 2015;15:39.
Satrom KM, Farouk ZL, Slusher TM. Management challenges in the treatment of severe hyperbilirubinemia in low- and middle-income countries: encouraging advancements, remaining gaps, and future opportunities. Front Pediatr. 2023;11:1001141.
Slusher TM, Zamora TG, Appiah D, Stanke JU, Strand MA, Lee BW, et al. Burden of severe neonatal jaundice: a systematic review and meta-analysis. BMJ Paediatr Open. 2017;1:e000105.
Kemper AR, Newman TB, Slaughter JL, Maisels MJ, Watchko JF, Downs SM, et al. Clinical Practice Guideline Revision: management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2022;150:e2022058859.
Mason E, McDougall L, Lawn JE, Gupta A, Claeson M, Pillay Y, et al. From evidence to action to deliver a healthy start for the next generation. Lancet. 2014;384:455–67.
Dickson KE, Simen-Kapeu A, Kinney MV, Huicho L, Vesel L, Lackritz E, et al. Every Newborn: health-systems bottlenecks and strategies to accelerate scale-up in countries. Lancet. 2014;384:438–54.
Akseer N, Lawn JE, Keenan W, Konstantopoulos A, Cooper P, Ismail Z, et al. Ending preventable newborn deaths in a generation. Int J Gynaecol Obstet. 2015;131:S43–48.
Kerber KJ, Mathai M, Lewis G, Flenady V, Erwich JJ, Segun T, et al. Counting every stillbirth and neonatal death through mortality audit to improve quality of care for every pregnant woman and her baby. BMC Pregnancy Childbirth. 2015;15:S9.
Bhutani VK, Stevenson DK. The need for technologies to prevent bilirubin-induced neurologic dysfunction syndrome. Semin Perinatol. 2011;35:97–100.
Lopez A. Global burden of disease and risk factors. Disease Control Priorities Project, editor. New York: Oxford University Press, 2006.
Kinney MV, Cocoman O, Dickson KE, Daelmans B, Zaka N, Rhoda NR, et al. Implementation of the Every Newborn Action Plan: progress and lessons learned. Semin Perinatol. 2015;39:326–37.
Blencowe H, Vos T, Lee ACC, Daelmans B, Zaka N, Rhoda NR, et al. Estimates of neonatal morbidities and disabilities at regional and global levels for 2010: introduction, methods overview, and relevant findings from the Global Burden of Disease study. Pediatr Res. 2013;74:4–16.
Moxon SG, Lawn JE, Dickson KE, Simen-Kapeu A, Gupta G, Deorari A, et al. Inpatient care of small and sick newborns: a multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy Childbirth. 2015;15:S7.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Disability Weights. 2020. https://doi.org/10.6069/1W19-VX76.
Hemolytic disease and other neonatal jaundice — Level 4 cause. Institute for Health Metrics and Evaluation. 2020; published online Oct 15. https://www.healthdata.org/results/gbd_summaries/2019/hemolytic-disease-and-other-neonatal-jaundice-level-4-cause (accessed June 20, 2023).
How are the income group thresholds determined? – World Bank Data Help Desk. https://datahelpdesk.worldbank.org/knowledgebase/articles/378833-how-are-the-income-group-thresholds-determined. Accessed 20 June 2023.
New country classifications by income level: 2018-2019. 2018; published online July 1. https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2018-2019 (accessed June 20, 2023).
World Population Prospects – Population Division – United Nations. https://population.un.org/wpp/ (accessed June 20, 2023).
Bhutani VK, Cline BK, Donaldson KM, Vreman HJ. The need to implement effective phototherapy in resource-constrained settings. Semin Perinatol. 2011;35:192–7.
Acknowledgements
We thank Professor Claudio Tiribelli, MD, Ph.D. (Trieste, Italy); Iman Iskander, MD (Cairo, Egypt); Praveen Kumar, MD (Chandigarh, India); Lizhong Du, MD (Hangzhou, China); Monica Villa Guillen, MD (Mexico City, Mexico); Zubaida Farouk, MD (Kano, Nigeria); Esterlita Uy, MD (Manila, Philippines), and Numan N. Hameed, MD (Baghdad, Iraq) for their insightful comments and guidance.
Author information
Authors and Affiliations
Contributions
VKB and RV conceptualized, designed, and developed the study, and drafted the initial manuscript, supervised, and performed data collection, analysis, and validation, revised the manuscript, developed Tables and Figures, and approved the final version. RJW critically reviewed the manuscript, revised the manuscript, and approved the final version as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Table 1 including the legend has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhutani, V.K., Vidavalur, R. & Wong, R.J. Advances to diminish global newborn kernicterus mortality. J Perinatol 44, 493–500 (2024). https://doi.org/10.1038/s41372-023-01862-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01862-7