Abstract
Objective
We hypothesize that the time, number of attempts, and physiologic stability of placement of an LMA would be superior compared to ETT.
Study design
Videotape and physiologic parameters of LMA (n = 36) and ETT (n = 31) placement procedures for infants 28–36 weeks gestation were reviewed.
Results
Duration of attempts (32 vs 66 s, p < 0.001) and mean total airway insertion time (88 vs 153 s, p = 0.06) was shorter for LMA compared to ETT. Mean number of attempts for successful placement was fewer for LMA (1.5 vs 1.9, p = 0.11). Physiologic parameters remained near baseline in both groups despite very different degrees of premedication.
Conclusion
Placement of an LMA required less time and fewer number of attempts compared to ETT. Physiologic stability of an LMA was maintained without the use of an analgesic and muscle relaxant. Use of an LMA is a favorable alternative to ETT placement for surfactant delivery in neonates.
Trial Registration
NCT01116921.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Descriptive analysis of placement of the LMA has been published in Neonatology 2017; 111(3): 222-227. https://doi.org/10.1159/00045069. Deidentified individual participant data (including data dictionaries) for LMA and ETT data will be made available, in addition to study protocol, the statistical analysis plan, and the informed consent form. The data will be made available upon publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal. Proposals should be submitted to rober694@umn.edu.
References
Marshall TA, Deeder R, Pai S, Berkowitz GP, Austin TL. Physiologic changes associated with endotracheal intubation in preterm infants. Crit Care Med. 1984;12:501–3.
Kelly MA, Finer NN. Nasotracheal intubation in the neonate: physiologic responses and effects of atropine and pancuronium. J Pediatr. 1984;105:303–9.
Friesen RH, Honda AT, Thieme RE. Changes in anterior fontanel pressure in preterm neonates during tracheal intubation. Anesth Analg. 1987;66:874–8.
Khammash HM, O BK, Dunn MS, Jefferies AL, Perlman M. Blunting of hypertensive response to endotracheal intubation in neonates by premedication. Paed Res. 1993;33:218A.
Millar C, Bissonnette B. Awake intubation increases intracranial pressure without affecting cerebral blood flow velocity in infants. Can J Anaesth. 1994;41:281–7.
Pokela ML, Koivisto M. Physiological changes, plasma beta-endorphin and cortisol responses to tracheal intubation in neonates. Acta Paediatr. 1994;83:151–6.
Barrington KJ, Finer NN, Etches PC. Succinylcholine and atropine for premedication of the newborn infant before nasotracheal intubation: a randomized, controlled trial. Crit Care Med. 1989;17:1293–6.
Kong AS, Brennan L, Bingham R, Morgan-Hughes J. An audit of induction of anaesthesia in neonates and small infants using pulse oximetry. Anaesthesia. 1992;47:896–9.
Gibbons PA, S D. Changes in oxygen saturation during elective tracheal intubation in infants. Anesth Analg. 1986;65:S58.
Bhutada A, Sahni R, Rastogi S, Wung JT. Randomised controlled trial of thiopental for intubation in neonates. Arch Dis Child Fetal Neonatal Ed. 2000;82:F34–7.
Raju TN, Vidyasagar D, Torres C, Grundy D, Bennett EJ. Intracranial pressure during intubation and anesthesia in infants. J Pediatr. 1980;96:860–2.
Stow PJ, McLeod ME, Burrows FA, Creighton RE. Anterior fontanelle pressure responses to tracheal intubation in the awake and anaesthetized infant. Br J Anaesth. 1988;60:167–70.
Roberts KD, Brown R, Lampland AL, Leone TA, Rudser KD, Finer NN, et al. Laryngeal mask airway for surfactant administration in neonates: a randomized, controlled trial. J Pediatr. 2018;193:40–6.
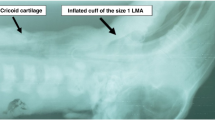
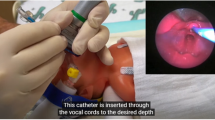
Wanous AA, Wey A, Rudser KD, Roberts KD. Feasibility of laryngeal mask airway device placement in neonates. Neonatology. 2017;111:222–7.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria. http://www.R-project.org/.
Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–9.
Hatch LD, Grubb PH, Lea AS, Walsh WF, Markham MH, Whitney GM, et al. Endotracheal intubation in neonates: a prospective study of adverse safety events in 162 infants. J Pediatr. 2016;168:62–6.
Foglia EE, Ades A, Sawyer T, Glass KM, Singh N, Jung P, et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics. 2019;143:e20180902.
Hatch LD, Grubb PH, Lea AS, Walsh WF, Markham MH, Maynord PO, et al. Interventions to improve patient safety during intubation in the neonatal intensive care unit. Pediatrics. 2016;138:e20160069.
Roberts KD, Leone TA, Edwards WH, Rich WD, Finer NN. Premedication for nonemergent neonatal intubations: a randomized, controlled trial comparing atropine and fentanyl to atropine, fentanyl, and mivacurium. Pediatrics. 2006;118:1583–91.
Sawyer T, Foglia E, Hatch LD, Moussa A, Ades A, Johnston L, et al. Improving neonatal intubation safety: a journey of a thousand miles. J Neonatal-Perinat Med. 2017;10:125–31.
Attridge JT, Stewart C, Stukenborg GJ, Kattwinkel J. Administration of rescue surfactant by laryngeal mask airway: lessons from a pilot trial. Am J Perinatol. 2013;30:201–6.
Sadeghnia A, Tanhaei M, Mohammadizadeh M, Nemati M. A comparison of surfactant administration through igel and ET-tube in the treatment of respiratory distress syndrome in newborns weighing more than 2000 g. Adv Biomed Res. 2014;3:160.
Pinheiro JMB, Santana-Rivas Q, Pezzano C. Randomized trial of laryngeal mask airway versus endotracheal intubation for surfactant delivery. J Perinatol. 2016;36:196–201.
Barbosa RF, Simões E Silva AC, Silva YP. A randomized controlled trial of the laryngeal mask airway for surfactant administration in neonates. J Pediatr. 2017;93:343–50.
Gharehbaghi M, Moghaddam YJ, Radfar R. Comparing the efficacy of surfactant administration by laryngeal mask airway and endotracheal intubation in neonatal respiratory distress syndrome. Crescent J Med Biol Sci. 2018;5:222–7.
Amini E, Sheikh M, Shariat M, Dalili H, Azadi N, Nourollahi S. Surfactant administration in preterm neonates using laryngeal mask airway: a randomized clinical trial. Acta Med Iran. 2019;57:348–54.
Singh R, Mohan CVR, Taxak S. Controlled trial to evaluate the use of LMA for neonatal resuscitation. J Anaesth Clin Pharm. 2005;21:303–6.
Zhu XY, Lin BC, Zhang QS, Ye HM, Yu RJ. A prospective evaluation of the efficacy of the laryngeal mask airway during neonatal resuscitation. Resuscitation. 2011;82:1405–9.
Trevisanuto D, Cavallin F, Nguyen LN, Nguyen TV, Tran LD, Tran CD, et al. Supreme laryngeal mask airway versus face mask during neonatal resuscitation: a randomized controlled trial. J Pediatr. 2015;167:286–91.
Pejovic NJ, Trevisanuto D, Lubulwa C, Hook SM, Cavallin F, Byamugisha J, et al. Neonatal resuscitation using a laryngeal mask airway: a randomised trial in Uganda. Arch Dis Child. 2018;103:255–60.
Feroze F, Khuwaja A, Masood N, Malik M. Neonatal resuscitation: the use of laryngeal mask airway. Prof Med J. 2008;15:148–52.
Esmail N, Saleh M, Ali A. Laryngeal mask airway versus endotracheal intubation for Apgar score improvement in neonatal resuscitation. Eg J Anesth. 2002;18:115–21.
Yang C, Zhu X, Lin W, Zhang Q, Su J, Lin B, et al. Randomized, controlled trial comparing laryngeal mask versus endotracheal intubation during neonatal resuscitation–a secondary publication. BMC Pediatr. 2016;16:17.
El-Ahmadi MB, El-Shimi MS, Abusaif IS, Khafagy SM, Mohamed RM. Efficacy of laryngeal mask airway in neonatal resuscitation. Egypt J Hosp Med. 2018;70:1767–72.
Sawyer T, Foglia EE, Ades A, Moussa A, Napolitano N, Glass K, et al. Incidence, impact and indicators of difficult intubations in the neonatal intensive care unit: a report from the National Emergency Airway Registry for Neonates. Arch Dis Child Fetal Neonatal Ed. 2019;104:F1–F6.
Funding
This work was supported by grants from the Minnesota Medical Foundation, Children’s Hospital Association, supporting Children’s Minnesota, and the Clinical and Translational Sciences Institute- University of Minnesota NCATS award UL1TR000114. Product support provided by LMA North America, Inc. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Roberts. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Wanous, Roberts. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Brown, Rudser. Administrative, technical, or material support: Roberts. Supervision: Rudser, Roberts.
Corresponding author
Ethics declarations
Competing interests
K Roberts is a paid consultant for ONY Biotech. All other authors have indicated they have no potential conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wanous, A.A., Brown, R., Rudser, K.D. et al. Comparison of laryngeal mask airway and endotracheal tube placement in neonates. J Perinatol 44, 239–243 (2024). https://doi.org/10.1038/s41372-023-01818-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01818-x