Abstract
Objective
To assess the reliability of pulmonary artery (PA) parameters as a prognostic marker in neonates with isolated left-sided congenital diaphragmatic hernia (IL-CDH).
Study design
A retrospective cohort study conducted by the Japanese CDH Study Group (JCDHSG).
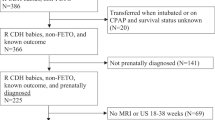
Results
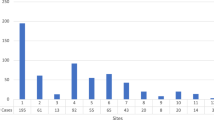
323 IL-CDH patients registered with the JCDHSG were included. 272 patients survived to 90 days of age. Right PA (RPA) and left PA (LPA) diameters and pulmonary artery index (PAIndex) at birth were significantly larger in survivors. The cutoff values of RPA and LPA diameters and PAIndex for survival up to 90 days were 3.2 mm, 2.8 mm and 83.7, respectively, and logistic regression analysis showed that these were significantly related to survival. Multiple logistic regression analysis showed that both the PA parameters and liver herniation were significantly related to survival.
Conclusions
The three PA parameters at birth can predict clinical outcomes and are considered as independent risk factors of liver herniation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and/analyzed during current study are available from the corresponding author on reasonable request.
References
Bagolan P, Morini F. Long-term follow up of infants with congenital diaphragmatic hernia. Semin Pediatr Surg. 2007;16:134–44.
Grover TR, Murthy K, Brozanski B, Gien J, Rintoul N, Keene S, et al. Children’s Hospitals Neonatal Consortium: Short-term outcomes and medical and surgical interventions in infants with congenital diaphragmatic hernia. Am J Perinatol. 2015;32:1038–44.
Boloker J, Bateman DA, Wung JT, Stolar CJ. Congenital diaphragmatic hernia in 120 infants treated consecutively with permissive hypercapnia/spontaneous respiration/elective repair. J Pediatr Surg. 2002;37:357–66.
Kitano Y, Nakagawa S, Kuroda T, Honna T, Ito Y, Nakamura T, et al. Liver position in fetal congenital diaphragmatic hernia retains a prognostic value in the era of lung-protective strategy. J Pediatr Surg. 2005;40:1827–32.
Lusk LA, Wai KC, Moon-Grady AJ, Basta AM, Filly R, Keller RL. Fetal ultrasound markers of severity predict resolution of pulmonary hypertension in congenital diaphragmatic hernia. Am J Obstet Gynecol. 2015;213:e211–e218.
Jani JC, Benachi A, Nicolaides KH, Allegaert K, Gratacos E, Mazkereth R, et al. Antenatal-CDH-Registry Group: Prenatal prediction of neonatal morbidity in survivors with congenital diaphragmatic hernia: a multicenter study. Ultrasound Obstet Gynecol. 2009;33:64–9.
Fauza DO, Wilson JM. Congenital diaphragmatic hernia and associated anomalies: their incidence, identification, and impact on prognosis. J Pediatr Surg. 1994;29:1113–7.
Kitagawa M, Hislop A, Boyden EA, Reid L. Lung hypoplasia in congenital diaphragmatic hernia: a quantitative study of airway, artery, and alveolar development. Br J Surg. 1971;58:342–6.
Kluth D, Keijer R, Hertl M, Tibboel D. Embryology of congenital diaphragmatic hernia. Semin Pediatr Surg. 1996;5:224–33.
Sokol J, Bohn D, Lacro RV, Ryan G, Stephens D, Rabinovitch M, et al. Fetal pulmonary artery diameters and their association with lung hypoplasia and postnatal outcome congenital diaphragmatic hernia. Am J Ostet Gynecol. 2002;186:1085–90.
Sokol J, Shimizu N, Bohn D, Doherty D, Ryan G, Hornberger LK. Fetal pulmonary artery diameter measurements as a predictor of morbidity in antenatally diagnosed congenital diaphragmatic hernia: A prospective study. Am J Obstet Gynecol. 2006;195:470–7.
Okazaki T, Okawada M, Shiyanagi S, Shoji H, Shimizu T, Tanaka T, et al. Significance of pulmonary artery size and blood flow as a predictor of outcome in congenital diaphragmatic hernia. Pediatr Surg Int. 2008;24:1369–73.
Yamoto M, Inamura N, Terui K, Nagata K, Kanamori Y, Hayakawa M, et al. Echocardiographic predictors of poor prognosis in congenital diaphragmatic Hernia. J Pediatr Surg. 2016;51:1926–30.
Takahashi S, Oishi Y, Ito N, Nanba Y, Tsukamoto K, Nakamura T, et al. Evaluating mortality and disease severity in congenital diaphragmatic hernia using the McGoon and pulmonary artery indices. J Pediatr Surg. 2009;44:2101–6.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36.
Hasegawa S, Kohno S, Sugiyama T, Sato Y, Seki S, Yagyu M, et al. Usefulness of echocardiographic measurement of bilateral pulmonary artery dimensions in congenital diaphragmatic hernia. J Pediatr Surg. 1994;29:622–4.
Okazaki T, Kohno S, Hasegawa S, Urushihara N, Yoshida A, Kawano S, et al. Congenital diaphragmatic hernia: efficacy of ultrasound examination in its management. Pediatr Surg Int. 2003;19:176–9.
Okazaki T, Nakazawa N, Ogasawara Y, Shoji H, Shimizu T, Makino S, et al. Increase in fetal pulmonary artery diameters during late gestation is a predictor of outcome in congenital diaphragmatic hernia with liver herniation. J Pediatr Surg. 2011;46:2254–9.
Piehlaer JM, Danielson GK, McGoon DC, Wallace RB, Fulton RE, Mair DD. Management of pulmonary artery with ventricular septal defect and hypoplastic pulmonary arteries by right ventricular outflow construction. J Thorac Cardiovasc Surg. 1980;80:552–67.
Nakata S, Imai Y, Takanashi Y, Kurosawa H, Tezuka K, Nakazawa M, et al. A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart disease with decreased pulmonary blood flow. J Thorac Cardiovasc Surg. 1984;88:610–9.
Suda K, Bigras JL, Bohn D, Hornberger LK, McCrindle BW. Echocardiographic predictors of outcome in newborns with congenital diaphragmatic hernia. Pediatrics. 2000;105:1106–9.
Casaccia G, Crescenzi F, Dotta A, Capolupo I, Braguglia A, Danhaive O, et al. Birth weight and McGoon Index predict mortality in newborns with congenital diaphragmatic hernia. J Pediatr Surg. 2006;41:25–8.
Acknowledgements
We would like to thank all members of JCDHSG for managements of patients and registrations to the database of JCDHSG. Funding: This study was funded by the Ministry of Health, Labour, and Welfare of Japan (Grant/Award Number: H24-Ninchi-Ippan-034).
Author information
Authors and Affiliations
Contributions
TO, KT, OH, SA, and NI made substantial contributions to the study conception and design. All authors performed clinical data collection. SN, YN, and NY made substantial contributions to statistical analysis and data interpretation. TO drafted the manuscript, and KT, MH, OH, KN, and NU reviewed the manuscript and provided critical feedback. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The protocol of this study was approved by the Ethics Committee of Osaka University Hospital (approval number 11017) and the committees at all participating institutions. The investigation was performed in accordance with the principles of the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okazaki, T., Terui, K., Nagata, K. et al. Assessment of pulmonary artery size at birth as a prognostic factor in congenital diaphragmatic hernia: results of a multicenter study in Japan. J Perinatol 43, 1295–1300 (2023). https://doi.org/10.1038/s41372-023-01750-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01750-0