Abstract
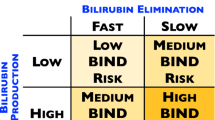
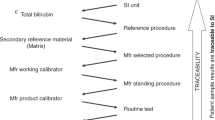
Identifying “gold standard” diagnostic tests can promote evidence-based neonatology practice. Hemolysis is a pathological shortening of the erythrocyte lifespan, differing from erythrocyte senescence in responsible mechanisms and clinical implications. Diagnosing hemolysis goes beyond a binary (yes vs. no) determination. It is characterized according to magnitude, and as acute vs. chronic, and genetically based vs. not. For neonates with significant hyperbilirubinemia or anemia, detecting hemolysis and quantifying its magnitude provides diagnostic clarity. The 2022 American Academy of Pediatrics (AAP) Clinical Practice Guideline on management of hyperbilirubinemia in the newborn states that hemolysis is a risk factor for developing significant hyperbilirubinemia and neurotoxicity. The guideline recommends identifying hemolysis from any cause, but specific guidance is not provided. A spectrum of laboratory tests has been endorsed as diagnostic methods for hemolysis. Herein we examine these laboratory tests and recommend one as the “gold standard” for diagnosing and quantifying hemolysis in neonates and infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Ann Intern Med. 2003;138:40–44.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527.
Lantos JD. Ethical problems in decision making in the neonatal ICU. N Engl J Med. 2018;379:1851–60.
Lantos JD. The Belmont Report and innovative clinical research. Perspect Biol Med. 2020;63:389–400.
Means RT Jr, Glader BE. Anemia: general considerations. In: Greer JP, Arber DA, Appelbaum FR, Rogers GM, Glader B, List AF, et al. editors. Wintrobe’s clinical hematology. 14th ed. Philadelphia, PA: Wolters Kluwer; 2019. p. 603–12.
Thiagarajan P, Parker CJ, Prchal JT. How do red blood cells die? Front Physiol. 2021;12:655393. https://doi.org/10.3389/fphys.2021.655393.
Johnson L, Bhutani VK, Karp K, Sivieri EM, Shapiro SM. Clinical report from the pilot USA Kernicterus Registry (1992 to 2004). J Perinatol. 2009;29:S25–45.
Bhutani VK, Wong RJ. A global approach to prevent kernicterus: a dedication to Lois Johnson-Hamerman (Sep. 14, 1927, to Aug. 11, 2019). Semin Perinatol. 2021;45:151350.
Christensen RD, Agarwal AM, George TI, Bhutani VK, Yaish HM. Acute neonatal bilirubin encephalopathy in the State of Utah 2009-2018. Blood Cells Mol Dis. 2018;72:10–13.
Bhutani VK, Johnson-Hamerman L. The clinical syndrome of bilirubin-induced neurologic dysfunction. Semin Fetal Neonatal Med. 2015;20:6–13.
Christensen RD, Yaish HM. Hemolytic disorders causing severe neonatal hyperbilirubinemia. Clin Perinatol. 2015;42:515–27.
Christensen RD, Nussenzveig RH, Yaish HM, Henry E, Eggert LD, Agarwal AM. Causes of hemolysis in neonates with extreme hyperbilirubinemia. J Perinatol. 2014;34:616–9.
Christensen RD, Lambert DK, Henry E, Eggert LD, Yaish HM, Reading NS, et al. Unexplained extreme hyperbilirubinemia among neonates in a multihospital healthcare system. Blood Cells Mol Dis. 2013;50:105–9.
Bhutani VK, Stevenson DK. The need for technologies to prevent bilirubin-induced neurologic dysfunction syndrome. Semin Perinatol. 2011;35:97–100.
Maisels MJ, Newman TB. Kernicterus in otherwise health, breast-fed term newborns. Pediatrics. 1995;96:730–3.
Bhandari J, Thada PK, Yadav D. Crigler najjar syndrome. Treasure Island, FL: StatPearls Publishing; 2023.
Strauss KA, Robinson DL, Vreman HJ, Puffenberger EG, Hart G, Morton DH. Management of hyperbilirubinemia and prevention of kernicterus in 20 patients with Crigler-Najjar disease. Eur J Pediatr. 2006;165:306–19.
Valsami S, Politou M, Boutsikou Τ, Briana D, Papatesta M, Malamitsi-Puchner A. Importance of direct antiglobulin test (DAT) in cord blood: causes of DAT (+) in a cohort study. Pediatr Neonatol. 2015;56:256–60.
Kaplan M, Hammerman C, Vreman HJ, Wong RJ, Stevenson DK. Direct antiglobulin titer strength and hyperbilirubinemia. Pediatrics. 2014;134:e1340–4.
Ross ME, Emery SP, de Alarcon PA, Watchko JF. Hemolytic disease of the fetus and newborn. maternal antibody mediated hemolysis. In: de Alarcon PA, Werner EJ, Christensen RD, Sola-Visner MC, editors. Neonatal hematology. Pathogenesis, diagnosis, and management of hematologic problems. 3rd ed. Cambridge: Cambridge University Press; 2021. p. 133–54.
Moise KJ. Hemolytic disease of the fetus and newborn. In: Creasy RK, Resnik R, editors. Maternal-fetal medicine: principles and practice. 6th ed. Philadelphia, PA: WB Saunders; 2008. p. 477–503.
Watchko JF. ABO hemolytic disease of the newborn: a need for clarity and consistency in diagnosis. J Perinatol. 2023;43:242–7.
Elsaie AL, Taleb M, Nicosia A, Zangaladze A, Pease ME, Newton K, et al. Comparison of end-tidal carbon monoxide measurements with direct antiglobulin tests in the management of neonatal hyperbilirubinemia. J Perinatol. 2020;40:1513–7.
Bahr TM, Shakib JH, Stipelman CH, Kawamoto K, Lauer S, Christensen RD. Improvement Initiative: end-tidal carbon monoxide measurement in newborns receiving phototherapy. J Pediatr. 2021;238:168–173.e2.
Christensen RD, Henry E, Bennett ST, Yaish HM. Reference intervals for reticulocyte parameters of infants during their first 90 days after birth. J Perinatol. 2016;36:61–6.
Hansen TWR, Wong RJ, Stevenson DK. Molecular physiology and pathophysiology of bilirubin handling by the blood, liver, intestine, and brain in the newborn. Physiol Rev. 2020;100:1291–346.
Bhutani VK, Wong RJ, Vreman HJ, Stevenson DK. Bilirubin production and hour-specific bilirubin levels. J Perinatol. 2015;35:735–8.
Petersen JR, Smith E, Okorodudu AO, Valbuena G, Bissell MG. Utilization of LDH isoenzymes in the diagnosis of myocardial infarction. Clin Lab Manage Rev. 1997;11:103–6.
Yaish HM, Christensen RD, Lemons RS. Neonatal nonimmune hemolytic anemia. Curr Opin Pediatr. 2017;29:12–9.
Bahr TM, Judkins AJ, Christensen RD, Baer VL, Henry E, Minton SD, et al. Neonates with suspected microangiopathic disorders: performance of standard manual schistocyte enumeration the automated fragmented red cell count. J Perinatol. 2019;39:1555–61.
Bahr TM, Christensen TR, Henry E, Judkins AJ, Bennett ST, Pysher TJ, et al. Fragmented red blood cell counts of neonates with new-onset gastrointestinal disturbances. J Perinatol. 2022. https://doi.org/10.1038/s41372-022-01587-z.
Christensen RD, Yaish HM, Lemons RS. Neonatal hemolytic jaundice: morphologic features of erythrocytes that will help you diagnose the underlying condition. Neonatology. 2014;105:243–9.
Gallagher PG. Diagnosis and management of rare congenital nonimmune hemolytic disease. Hematol Am Soc Hematol Educ Program. 2015;2015:392–9.
Vreman HJ, Kwong LK, Stevenson DK. Carbon monoxide in blood: an improved microliter blood-sample collection system, with rapid analysis by gas chromatography. Clin Chem. 1984;30:1382–6.
Maisels MJ, Pathak A, Nelson NM, Nathan DG, Smith CA. Endogenous production of carbon monoxide in normal and erythroblastotic newborn infants. J Clin Invest. 1971;50:1–8.
Tidmarsh GF, Wong RJ, Stevenson DK. End-tidal carbon monoxide and hemolysis. J Perinatol. 2014;34:577–81.
Vreman HJ, Mahoney JJ, Stevenson DK. Carbon monoxide and carboxyhemoglobin. Adv Pediatr. 1995;42:303–4.
Vreman HJ, Stevenson DK, Oh W, Fanaroff AA, Wright LL, Lemons JA, et al. Semiportable electrochemical instrument for determining carbon monoxide in breath. Clin Chem. 1994;40:1927–33.
Stevenson DK, Vreman HJ, Oh W, Fanaroff AA, Wright LL, Lemons JA, et al. Bilirubin production in healthy term infants as measured by carbon monoxide in breath. Clin Chem. 1994;40:1934–39.
Vreman HJ, Baxter LM, Stone RT, Stevenson DK. Evaluation of a fully automated end-tidal carbon monoxide instrument for breath analysis. Clin Chem. 1996;42:50–6.
Stevenson DK, Vreman HJ. Carbon monoxide and bilirubin production in neonates. Pediatrics. 1997;100:252–4.
Stevenson DK, Vreman HJ, Wong RJ, Contag CH. Carbon monoxide and bilirubin production in neonates. Semin Perinatol. 2001;25:85–93.
Vreman HJ, Wong RJ, Harmatz P, Fanaroff AA, Berman B, Stevenson DK. Validation of the Natus CO-Stat End Tidal Breath analyzer in children and adults. J Clin Monit Comput. 1999;15:421–7.
Krediet TG, Cirkel GA, Vreman HJ, Wong RJ, Stevenson DK, Groenendaal F, et al. End-tidal carbon monoxide measurements in infant respiratory distress syndrome. Acta Paediatr. 2006;95:1075–82.
Stevenson DK, Fanaroff AA, Maisels MJ, Young BW, Wong RJ, Vreman HJ, et al. Prediction of hyperbilirubinemia in near-term and term infants. Pediatrics. 2001;108:31–9.
American Academy of Pediatrics. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–16.
James EB, Vreman HJ, Wong RJ, Stevenson DK, Vichinsky E, Schumacher L, et al. Elevated exhaled carbon monoxide concentration in hemoglobinopathies and its relation to red blood cell transfusion therapy. Pediatr Hematol Oncol. 2010;27:112–21.
Castillo Cuadrado ME, Bhutani VK, Aby JL, Vreman HJ, Wong RJ, Stevenson DK. Evaluation of a new end-tidal carbon monoxide monitor from the bench to the bedside. Acta Paediatr. 2015;104:e279–82.
Bhutani VK, Wong RJ, Vreman HJ, Stevenson DK, Jaundice Multinational Study Group. Bilirubin production and hour-specific bilirubin levels. J Perinatol. 2015;35:735–8.
Christensen RD, Lambert DK, Henry E, Yaish HM, Prchal JT. End-tidal carbon monoxide as an indicator of the hemolytic rate. Blood Cells Mol Dis. 2015;54:292–6.
Bhutani VK, Srinivas S, Castillo Cuadrado ME, Aby JL, Wong RJ, Stevenson DK. Identification of neonatal haemolysis: an approach to predischarge management of neonatal hyperbilirubinemia. Acta Paediatr. 2016;105:e189–94.
Christensen RD, Malleske DT, Lambert DK, Baer VL, Prchal JT, Denson LE, et al. Measuring end-tidal carbon monoxide of jaundiced neonates in the birth hospital to identify those with hemolysis. Neonatology. 2016;109:1–5.
Wong RJ, Bhutani VK, Stevenson DK. The importance of hemolysis and its clinical detection in neonates with hyperbilirubinemia. Curr Pediatr Rev. 2017;13:193–8.
Bhutani VK, Maisels MJ, Schutzman DL, Castillo Cuadrado ME, Aby JL, Bogen DL, et al. Identification of risk for neonatal haemolysis. Acta Paediatr. 2018;107:1350–6.
Bhatia A, Chua MC, Dela Puerta R, Rajadurai VS. Noninvasive detection of hemolysis with ETCOc measurement in neonates at risk for significant hyperbilirubinemia. Neonatology. 2020;117:612–8.
Du L, Ma X, Shen X, Bao Y, Chen L, Bhutani VK. Neonatal hyperbilirubinemia management: clinical assessment of bilirubin production. Semin Perinatol. 2021;45:151351.
Pakdeeto S, Christensen TR, Bahr TM, Gerday E, Sheffield MJ, Christensen KS, et al. Reference intervals for end-tidal carbon monoxide of preterm neonates. J Perinatol. 2022;42:116–20.
Bao Y, Zhu J, Ma L, Zhang H, Sun L, Xu C, et al. An end-tidal carbon monoxide nomogram for term and late-preterm chinese newborns. J Pediatr. 2022;250:16–21.e3.
Christensen RD, Bahr TM, Pakdeeto S, Supapannachart S, Zhang H. Perinatal hemolytic disorders, and identification using end tidal breath carbon monoxide. Curr Pediatr Rev. 2023;19:376–87.
Kemper AR, Newman TB, Slaughter JL, Maisels MJ, Watchko JF, Downs SM, et al. Clinical practice guideline revision: management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2022;150:e2022058859.
Author information
Authors and Affiliations
Contributions
Conception and design: RDC and TMB. RDC wrote the initial draft of the manuscript. TMB, RJW, HJV, VKB, DKS reviewed all versions of the article and contributed to revising and improving the manuscript. All authors approved the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christensen, R.D., Bahr, T.M., Wong, R.J. et al. A “Gold Standard” Test for Diagnosing and Quantifying Hemolysis in Neonates and Infants. J Perinatol 43, 1541–1547 (2023). https://doi.org/10.1038/s41372-023-01730-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01730-4
This article is cited by
-
Is it time for a precision health approach to the management of newborn hyperbilirubinemia?
Journal of Perinatology (2024)
-
Erythrokinetic mechanism(s) causing the “late anemia” of hemolytic disease of the fetus and newborn
Journal of Perinatology (2024)
-
Alloimmune hemolytic disease of the fetus and newborn: genetics, structure, and function of the commonly involved erythrocyte antigens
Journal of Perinatology (2023)