Abstract
Objective
To evaluate the effects of guideline-driven prophylactic supplementation of a multi-strain neonatal intensive care unit-specific probiotic product on infants born very preterm (VP) or very low birth weight (VLBW).
Study design
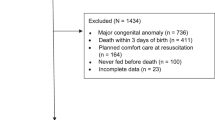
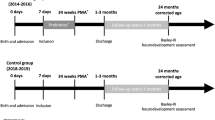
A prospective cohort of 125 infants born in one year after implementation who received probiotics were compared to a retrospective cohort of eligible 126 VP or VLBW infants who did not receive probiotics. The primary outcome of interest was necrotizing enterocolitis (NEC).
Result
The incidence of NEC decreased from 6.3 to 1.6%. After adjusting for multiple variables, there were no significant differences in primary or other outcomes of interest; odds ratio (95% confidence interval) NEC 0.27 (0.05–1.33), death 0.76 (0.26–2.21) and late-onset sepsis 0.54 (0.18–1.63). No adverse effects related to probiotics supplementation were observed.
Conclusion
Although nonsignificant, prophylactic probiotics supplementation in infants born VP or VLBW was associated with reduction of NEC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The de-identified dataset generated from the study is available on reasonable request and upon approval by the Institutional Review Board of Baylor Scott & White Health.
References
Jacob J, Kamitsuka M, Clark RH, Kelleher AS, Spitzer AR. Etiologies of NICU deaths. Pediatrics. 2015;135:e59–65.
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Mortality, In-Hospital Morbidity, Care Practices, and 2-Year Outcomes for Extremely Preterm Infants in the US, 2013-2018. JAMA. 2022;327:248–63.
Claud EC, Walker WA. Hypothesis: inappropriate colonization of the premature intestine can cause neonatal necrotizing enterocolitis. FASEB J. 2001;15:1398–403.
Hunter CJ, Upperman JS, Ford HR, Camerini V. Understanding the susceptibility of the premature infant to necrotizing enterocolitis (NEC). Pediatr Res. 2008;63:117–23.
Wang Y, Hoenig JD, Malin KJ, Qamar S, Petrof EO, Sun J, et al. 16S rRNA gene-based analysis of fecal microbiota from preterm infants with and without necrotizing enterocolitis. ISME J. 2009;3:944–54.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11:506–14.
Halloran K, Underwood MA. Probiotic mechanisms of action. Early Hum Dev. 2019;135:58–65.
Patel RM, Underwood MA. Probiotics and necrotizing enterocolitis. Semin Pediatr Surg. 2018;27:39–46.
Xiong T, Maheshwari A, Neu J, Ei-Saie A, Pammi M. An Overview of Systematic Reviews of Randomized-Controlled Trials for Preventing Necrotizing Enterocolitis in Preterm Infants. Neonatology. 2020;117:46–56.
Sawh SC, Deshpande S, Jansen S, Reynaert CJ, Jones PM. Prevention of necrotizing enterocolitis with probiotics: a systematic review and meta-analysis. PeerJ. 2016;4:e2429.
Sharif S, Meader N, Oddie SJ, Rojas-Reyes MX, McGuire W. Probiotics to prevent necrotising enterocolitis in very preterm or very low birth weight infants. Cochrane Database Syst Rev. 2020;10:CD005496.
Razak A, Patel RM, Gautham KS. Use of Probiotics to Prevent Necrotizing Enterocolitis: Evidence to Clinical Practice. JAMA Pediatr. 2021;175:773–4.
Viswanathan S, Lau C, Akbari H, Hoyen C, Walsh MC. Survey and evidence-based review of probiotics used in very low birth weight preterm infants within the United States. J Perinatol. 2016;36:1106–11.
Gray KD, Messina JA, Cortina C, Owens T, Fowler M, Foster M, et al. Probiotic Use and Safety in the Neonatal Intensive Care Unit: A Matched Cohort Study. J Pediatr. 2020;222:59–64.e1.
Barbian ME, Buckle R, Denning PW, Patel RM. To start or not: Factors to consider when implementing routine probiotic use in the NICU. Early Hum Dev. 2019;135:66–71.
Patel AL, Engstrom JL, Meier PP, Kimura RE. Accuracy of methods for calculating postnatal growth velocity for extremely low birth weight infants. Pediatrics. 2005;116:1466–73.
Vermont Oxford Network. 2021 Manual of Operations, Part 2, Release 25.0. 2021. https://vtoxford.zendesk.com/hc/en-us/articles/360056768093-2021-Manual-of-Operations-Part-2-Release-25-0-PDF.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. National Institutes of Child Health and Human Development Neonatal Research Network. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, et al. International Classification of Retinopathy of Prematurity, Third Edition. Ophthalmology. 2021;128:e51–68.
Papile L-A, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92:529–34.
Deshmukh M, Patole S. Prophylactic Probiotic Supplementation for Preterm Neonates-A Systematic Review and Meta-Analysis of Nonrandomized Studies. Adv Nutr. 2021;12:1411–23.
Swanson JR, Hair A, Clark RH, Gordon PV. Spontaneous intestinal perforation (SIP) will soon become the most common form of surgical bowel disease in the extremely low birth weight (ELBW) infant. J Perinatol. 2022;42:423–9.
Neu J. Necrotizing Enterocolitis: The Future. Neonatology. 2020;117:240–4.
Patel RM, Ferguson J, McElroy SJ, Khashu M, Caplan MS. Defining necrotizing enterocolitis: current difficulties and future opportunities. Pediatr Res. 2020;88:10–5.
Bin-Nun A, Bromiker R, Wilschanski M, Kaplan M, Rudensky B, Caplan M, et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight neonates. J Pediatr. 2005;147:192–6.
Jacobs SE, Tobin JM, Opie GF, Donath S, Tabrizi SN, Pirotta M, et al. ProPrems Study Group. Probiotic effects on late-onset sepsis in very preterm infants: a randomized controlled trial. Pediatrics. 2013;132:1055–62.
Jacobs SE, Hickey L, Donath S, Opie GF, Anderson PJ, Garland SM, et al. ProPremsStudy Groups. Probiotics, prematurity and neurodevelopment: follow-up of a randomised trial. BMJ Paediatr Open. 2017;1:e000176.
van den Akker CHP, van Goudoever JB, Shamir R, Domellöf M, Embleton ND, Hojsak I, et al. Probiotics and Preterm Infants: A Position Paper by the European Society for Paediatric Gastroenterology Hepatology and Nutrition Committee on Nutrition and the European Society for Paediatric Gastroenterology Hepatology and Nutrition Working Group for Probiotics and Prebiotics. J Pediatr Gastroenterol Nutr. 2020;70:664–80.
Morgan RL, Preidis GA, Kashyap PC, Weizman AV, Sadeghirad B, McMaster Probiotic, Prebiotic, and Synbiotic Work Group. Probiotics Reduce Mortality and Morbidity in Preterm, Low-Birth-Weight Infants: A Systematic Review and Network Meta-analysis of Randomized Trials. Gastroenterology. 2020;159:467–80.
van den Akker CHP, van Goudoever JB, Szajewska H, Embleton ND, Hojsak I, Reid D, et al. ESPGHAN Working Group for Probiotics, Prebiotics & Committee on Nutrition. Probiotics for Preterm Infants: A Strain-Specific Systematic Review and Network Meta-analysis. J Pediatr Gastroenterol Nutr. 2018;67:103–22.
Jungersen M, Wind A, Johansen E, Christensen JE, Stuer-Lauridsen B, Eskesen D. The Science behind the Probiotic Strain Bifidobacterium animalis subsp. lactis BB-12(®). Microorganisms. 2014;2:92–110.
Data on file. Abbott Nutrition. 2020. https://static.abbottnutrition.com/cms-prod/abbottnutrition-2016.com/img/Similac-Probiotic-Tri-Blend.pdf.
Poindexter B. COMMITTEE ON FETUS AND NEWBORN. Use of Probiotics in Preterm Infants. Pediatrics. 2021;147:e2021051485.
Marchand V. Using probiotics in the paediatric population. Paediatr Child Health. 2012;17:575–6.
Martin R, Nauta AJ, Ben Amor K, Knippels LM, Knol J, Garssen J. Early life: gut microbiota and immune development in infancy. Benef Microbes. 2010;1:367–82.
Torrazza RM, Neu J. The altered gut microbiome and necrotizing enterocolitis. Clin Perinatol. 2013;40:93–108.
Hackam DJ, Sodhi CP. Toll-Like Receptor-Mediated Intestinal Inflammatory Imbalance in the Pathogenesis of Necrotizing Enterocolitis. Cell Mol Gastroenterol Hepatol. 2018;6:229–38.e1.
Gritz EC, Bhandari V. The human neonatal gut microbiome: a brief review. Front Pediatr. 2015;3:17.
Groer MW, Luciano AA, Dishaw LJ, Ashmeade TL, Miller E, Gilbert JA. Development of the preterm infant gut microbiome: a research priority. Microbiome. 2014;2:38.
Hays S, Jacquot A, Gauthier H, Kempf C, Beissel A, Pidoux O, et al. Probiotics and growth in preterm infants: A randomized controlled trial, PREMAPRO study. Clin Nutr. 2016;35:802–11.
Million M, Angelakis E, Paul M, Armougom F, Leibovici L, Raoult D. Comparative meta-analysis of the effect of lactobacillus species on weight gain in humans and animals. Micro Pathog. 2012;53:100e8.
Vallabhaneni S, Walker TA, Lockhart SR, Ng D, Chiller T, Melchreit R, et al. Centers for Disease Control and Prevention (CDC). Notes from the field: Fatal gastrointestinal mucormycosis in a premature infant associated with a contaminated dietary supplement—Connecticut, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:155–6.
Kulkarni T, Majarikar S, Deshmukh M, Ananthan A, Balasubramanian H, Keil A, et al. Probiotic sepsis in preterm neonates-a systematic review. Eur J Pediatr. 2022;181:2249–62.
Jena PK, Sheng L, Nagar N, Wu C, Barile D, Mills DA, et al. The effect of synbiotics Bifidobacterium infantis and milk oligosaccharides on shaping gut microbiota community structure and NASH treatment. Data Brief. 2018;19:1025–9.
Chi C, Li C, Buys N, Wang W, Yin C, Sun J. Effects of Probiotics in Preterm Infants: A Network Meta-analysis. Pediatrics. 2021;147:e20200706.
Author information
Authors and Affiliations
Contributions
AC contributed to conceptualization/design, methodology, data curation, formal analysis and drafted the paper. HH and RH contributed to the methodology, data curation, formal analysis and drafted the paper. AR and JR contributed to the methodology, data curation and reviewed the manuscript. SD contributed to the methodology, formal analysis and reviewed the paper. MS contributed to conceptualization/design, methodology and reviewed the paper.
Corresponding author
Ethics declarations
Competing interests
AC has received speaking honoraria from Abbott nutrition. The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chiruvolu, A., Hendrikson, H., Hanson, R. et al. Effects of prophylactic probiotics supplementation on infants born very preterm or very low birth weight. J Perinatol 43, 635–641 (2023). https://doi.org/10.1038/s41372-023-01657-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01657-w
This article is cited by
-
Probiotics for Preterm Infants—Update 2024
Current Treatment Options in Pediatrics (2024)