Abstract
Objectives
To estimate national prevalence of household hardships (food insufficiency, financial hardship, and difficulty paying medical bills) among children born term and preterm; and examine associations of household hardships with preterm children’s outcomes (health status, emergency room visits, and unmet healthcare needs).
Methods
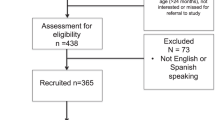
We studied 24,026 children aged 0–3 years born term, preterm with moderately low birth weight (1501–2499 grams) and preterm with very low birth weight (VLBW; ≤1500 grams). Using propensity score matching to control for correlates of poverty, we examined associations of hardships and child outcomes.
Results
Compared with term, households with preterm VLBW children had >2-fold higher odds of financial hardship (aOR:2.63; 95% CI: 1.26–5.46) and >5-fold higher odds of difficulty paying bills (aOR:5.60; 95% CI: 2.35–10.35). Matching for sociodemographics, special healthcare needs, income and receipt of public benefits, hardships were independently associated with adverse preterm children’s outcomes.
Conclusions
Addressing household hardships is needed to optimize preterm child outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Dataset and codebooks for the National Survey of Children’s Health are publicly available in the Data Resource Center for Child & Adolescent Health at https://www.childhealthdata.org/.
References
Institute of Medicine Committee on Understanding Premature B, Assuring Healthy O. The National Academies Collection: Reports funded by National Institutes of Health. In: Behrman RE, Butler AS, editors. Preterm Birth: Causes, Consequences, and Prevention. Washington (DC): National Academies Press (US) Copyright © 2007, National Academy of Sciences.; 2007.
COUNCIL ON COMMUNITY PEDIATRICS. Poverty and Child Health in the United States. Pediatrics. 2016;137:e20160339. https://doi.org/10.1542/peds.2016-0339.
Brocht C, Boushey H, Bernstein J. In: Institute EP, editor. Hardships in America: the real story of working families 2001. p. 19–42.
Rodems R, Shaefer L. Many of the kids are not alright: material hardships among children in the United States. University of Michigan; 2019.
Wallace ME, Mendola P, Chen Z, Hwang BS, Grantz KL. Preterm birth in the context of increasing income inequality. Matern Child Health J. 2016;20:164–71.
Gershoff ET, Aber JL, Raver CC, Lennon MC. Income is not enough: incorporating material hardship into models of income associations with parenting and child development. Child Dev. 2007;78:70–95.
Cutts DB, Coleman S, Black MM, Chilton MM, Cook JT, de Cuba SE, et al. Homelessness during pregnancy: a unique, time-dependent risk factor of birth outcomes. Matern Child Health J. 2015;19:1276–83.
Dolatian M, Sharifi N, Mahmoodi Z. Relationship of socioeconomic status, psychosocial factors, and food insecurity with preterm labor: A longitudinal study. Int J Reprod Biomed. 2018;16:563–70.
Stein RE, Siegel MJ, Bauman LJ. Double jeopardy: what social risk adds to biomedical risk in understanding child health and health care utilization. Acad Pediatr. 2010;10:165–71.
Child and Adolescent Health Measurement Initiative. The National Survey of Children’s Health. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). 2016–2018.
Ghandour RM, Jones JR, Lebrun-Harris LA, Minnaert J, Blumberg SJ, Fields J, et al. The design and implementation of the 2016 national survey of children’s health. Matern Child Health J. 2018;22:1093–102.
Chaudry A, Wimer C. Poverty is not just an indicator: the relationship between income, poverty, and child well-being. Acad Pediatr. 2016;16:S23–9.
Litt JS, McCormick MC. Preterm infants are less likely to have a family-centered medical home than term-born peers. J Perinatol. 2018;38:1391–7.
Mandy G. Uptodate. Incidence and mortality of the preterm infant 2021 [updated April 23, 2021]. Available from: https://www.uptodate.com/contents/incidence-and-mortality-of-the-preterm-infant?search=Classification%20of%20prematurity%20categorized%20by%20birth%20weight%20or%20gestational%20age&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3#H1018659388.
U.S. Department of Agriculture. What is food insufficiency? Available from: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/measurement.aspx#insufficiency.
Schanzenbach D, Pitts A. How much has food insecurity risen? Evidence from the census household pulse survey. Institute for Policy Research, Northwestern University. 2020;10.
Fuller AE, Garg A, Brown NM, Tripodis Y, Oyeku SO, Gross RS. Relationships between material hardship, resilience, and health care use. Pediatrics. 2020;145:e20191975.
Cunningham PJ. Trade-offs getting tougher: problems paying medical bills increase for U.S. families, 2003–2007. Track Rep. 2008;21:1–5.
Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121:337–44.
Webb R, Whitham A, Tripodis Y, Long WE, Garg A. Does parental report of having a medical home attenuate the negative association between unmet basic needs and health for low-income children? Glob Pediatr Health. 2020;7:2333794x20985805.
Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:e286–98.
Boyd RW, Lindo EG, Weeks LD, McLemore MR. Health Affairs [Internet]2020. [cited 2020]. Available from: https://www.healthaffairs.org/do/10.1377/forefront.20200630.939347/.
US Census Bureau. 2018 National Survey of Children’s Health. Guide to Multi-Year Estimates., Commerce. USDo; 2019.
D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–81.
Lewis TP, Andrews KG, Shenberger E, Betancourt TS, Fink G, Pereira S, et al. Caregiving can be costly: a qualitative study of barriers and facilitators to conducting kangaroo mother care in a US tertiary hospital neonatal intensive care unit. BMC Pregnancy Childbirth. 2019;19:227.
Linares DE, Azuine RE, Singh GK. Social determinants of health associated with mental health among U.S. mothers with children aged 0–5 years. J Women’s Health (Larchmt). 2020;29:1039–51.
Goldstein RF, Malcolm WF. Care of the Neonatal Intensive Care Unit Graduate after Discharge. Pediatr Clin North Am. 2019;66:489–508.
Lakshmanan A, Song AY, Belfort MB, Yieh L, Dukhovny D, Friedlich PS, et al. The financial burden experienced by families of preterm infants after NICU discharge. J Perinatol. 2021;42:1–8.
Kuhlthau K, Hill KS, Yucel R, Perrin JM. Financial burden for families of children with special health care needs. Matern Child Health J. 2005;9:207–18.
Parish SL, Rose RA, Grinstein-Weiss M, Richman EL, Andrews ME. Material hardship in U.S. families raising children with disabilities. Exceptional Child. 2008;75:71–92.
Cook JT, Frank DA, Berkowitz C, Black MM, Casey PH, Cutts DB, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134:1432–8.
Drennen CR, Coleman SM, Ettinger de Cuba S, Frank DA, Chilton M, Cook JT, et al. Food insecurity, health, and development in children under age four years. Pediatrics. 2019;144:e20190824.
Rose-Jacobs R, Black MM, Casey PH, Cook JT, Cutts DB, Chilton M, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121:65–72.
Casey PH, Szeto K, Lensing S, Bogle M, Weber J. Children in food-insufficient, low-income families: prevalence, health, and nutrition status. Arch Pediatr Adolesc Med. 2001;155:508–14.
Frank DA, Neault NB, Skalicky A, Cook JT, Wilson JD, Levenson S, et al. Heat or eat: the Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics 2006;118:e1293–302.
Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, et al. US Housing insecurity and the health of very young children. Am J Public Health. 2011;101:1508–14.
Sandel M, Sheward R, Ettinger de Cuba S, Coleman SM, Frank DA, Chilton M, et al. Unstable Housing and Caregiver and Child Health in Renter Families. Pediatrics. 2018;141:e20172199.
Fuller AE, Brown NM, Grado L, Oyeku SO, Gross RS. Material hardships and health care utilization among low-income children with special health care needs. Acad Pediatr. 2019;19:733–9.
Patel AL, Johnson TJ, Meier PP. Racial and socioeconomic disparities in breast milk feedings in US neonatal intensive care units. Pediatr Res. 2021;89:344–52.
Melchior M, Caspi A, Howard LM, Ambler AP, Bolton H, Mountain N, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. 2009;124:e564–72.
Rice JL, McGrath-Morrow SA, Collaco JM. Indoor air pollution sources and respiratory symptoms in bronchopulmonary dysplasia. J Pediatr. 2020;222:85–90.e2.
Koball H, Moore A, Hernandez J. Basic Facts About Low-Income Children children under 18 years. National Center for Children in Poverty; 2021.
Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90:1212–5.
Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting black lives - the role of health professionals. N. Engl J Med. 2016;375:2113–5.
Parker MG, Garg A, McConnell MA. Addressing childhood poverty in pediatric clinical settings: the neonatal intensive care unit is a missed opportunity. JAMA Pediatr. 2020;174:1135–6.
Cordova-Ramos EG, Kerr S, Heeren T, Drainoni ML, Garg A, Parker MG. National Prevalence of Social Determinants of Health Screening Among US Neonatal Care Units. Hosp Pediatr. 2022;e2022006767. https://doi.org/10.1542/hpeds.2022-006767.
Lakshmanan A, Kubicek K, Williams R, Robles M, Vanderbilt DL, Mirzaian CB, et al. Viewpoints from families for improving transition from NICU-to-home for infants with medical complexity at a safety net hospital: a qualitative study. BMC Pediatr. 2019;19:223.
Funding
This work was supported by the Evans Center for Implementation and Improvement Sciences (Department of Medicine, Boston University School of Medicine). EGCR is supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through BU-CTSI Grant Number 1KL2TR001411. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
ECR and MGP contributed to conceptualization and design, analysis, and drafted and edited the manuscript. YT contribute to design and data analysis. AB, AG and YT contributed to data interpretation, and reviewed and edited the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cordova-Ramos, E.G., Brochier, A., Tripodis, Y. et al. Beyond income: material hardship and the health and healthcare of premature children. J Perinatol 43, 357–363 (2023). https://doi.org/10.1038/s41372-022-01560-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01560-w