Abstract
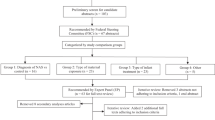
Prenatal opioid exposure has recently risen four-fold with limited data on the developmental effects on neonatal physiology. The objective of this systematic review is to develop an association between prenatal opioid exposure and fetal and neonatal cardiac and autonomic development and function. The review was conducted in accordance with PRISMA Guidelines, and searches were conducted using PubMed, Embase, CINAHL, and Web of Science between May 25 and October 27, 2020. Twenty studies fit inclusion criteria, in four categories: (1) fetal cardiac outcomes, (2) neonatal cardiac outcomes, (3) noninvasive autonomic outcomes, and (4) clinical and behavioral measures. For the meta-analysis, three studies (total of 210 subjects) were included. Effect sizes were measured as the mean difference in fetal heart rate between opioid-exposed and non-exposed groups. Mothers with prenatal opioid use had a significantly lower fetal heart rate as compared to mothers without prenatal opioid use, requiring further studies to determine clinical significance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ko JY, Wolicki S, Barfield WD, Patrick SW, Broussard CS, Yonkers KA, et al. CDC grand rounds: public health strategies to prevent neonatal abstinence syndrome. Mmwr Morbidity Mortal Wkly Rep. 2017;66:242.
Alinejad S, Kazemi T, Zamani N, Hoffman RS, Mehrpour O. A systematic review of the cardiotoxicity of methadone. EXCLI J. 2015;14:577–600. https://doi.org/10.17179/excli2015-553.
Finnegan LP, Connaughton JF Jr, Kron RE, Emich JP. Neonatal abstinence syndrome: assessment and management. Addictive Dis. 1975;2:141–58.
Hudak ML, Tan RC. Neonatal drug withdrawal. Pediatrics. 2012;129:e540–e560.
Oji-Mmuo CN, Gardner FC, Doheny KK. Heightened sympathetic arousal is demonstrated by skin conductance responsivity to auditory stimuli in a small cohort of neonates with opiate withdrawal. Brain Res Bull. 2018;138:106–11. https://doi.org/10.1016/j.brainresbull.2017.06.007.
Oji-Mmuo CN, Michael EJ, McLatchy J, Lewis MM, Becker JE, Doheny KK. Skin conductance at baseline and postheel lance reflects sympathetic activation in neonatal opiate withdrawal. Acta Paediatr. 2016;105:e99–e106. https://doi.org/10.1111/apa.13287.
Oji-Mmuo CN, Speer RR, Gardner FC, Marvin MM, Hozella AC, Doheny KK Prenatal opioid exposure heightens sympathetic arousal and facial expressions of pain/distress in term neonates at 24-48h post birth. J Matern Fetal Neonatal Med. 2019;1–8. https://doi.org/10.1080/14767058.2019.1588876.
Conradt E, Sheinkopf SJ, Lester BM, Tronick E, LeGasse LL, Shankaran S, et al. Prenatal substance exposure: neurobiologic organization at 1 month. J Pediatr. 2013;163:989–994 e981. https://doi.org/10.1016/j.jpeds.2013.04.033.
Reddy UM, Davis JM, Ren Z, Green MF. Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes: Executive Summary of a Joint Workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, American College of Obstetricians and Gynecologists, American Academy of Pediatrics, Society for Maternal-Fetal Medicine, Centers for Disease Control and Prevention, and the March of Dimes Foundation. Obstet Gynecol. 2017;130:10–28. https://doi.org/10.1097/AOG.0000000000002054.
Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307:1934–40.
Desmond M, Wilson G. Neonatal abstinence syndrome: recognition and diagnosis. Addictive Dis. 1975;2:113–21.
Wolf AR, Humphry AT. Limitations and vulnerabilities of the neonatal cardiovascular system: considerations for anesthetic management. Paediatr Anaesth. 2014;24:5–9. https://doi.org/10.1111/pan.12290.
Hattler J, Klimek M, Rossaint R, Heesen M. The effect of combined spinal–epidural versus epidural analgesia in laboring women on nonreassuring fetal heart rate tracings: systematic review and meta-analysis. Anesth Analg. 2016;123:955–64.
Mardirosoff C, Dumont L, Boulvain M, Tramèr MR. Fetal bradycardia due to intrathecal opioids for labour analgesia: a systematic review. BJOG. 2002;109:274–81.
Otis EM, Brent R. Equivalent ages in mouse and human embryos. Anat Rec. 1954;120:33–63.
Borenstein M, Cooper H, Hedges L, Valentine J. Effect sizes for continuous data. Handb Res Synth Meta-Anal. 2009;2:221–35.
V. Fetal heart rate and variability. Monogr Soc Res Child Dev. 2015;80:23–32. https://doi.org/10.1111/mono.12175.
National Heart Lung and Blood Institute, National Institutes of Health. 2021. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
Escalona‐Vargas D, Coker JL, Ray-Griffith S, Siegel ER, Lowery CL, Showe ZN, et al. Fetal assessment in buprenorphine‐maintained women using fetal magnetoencephalography: a pilot study. Addiction. 2018;113:1895–904.
Jansson LM, DiPietro J, Elko A. Fetal response to maternal methadone administration. Am J Obstet Gynecol. 2005;193:611–7.
Jansson L, Di Pietro JA, Elko A, Williams EL, Milio L, Velez M. Pregnancies exposed to methadone, methadone and other illicit substances, and poly-drugs without methadone: a comparison of fetal neurobehaviors and infant outcomes. Drug Alcohol Depend. 2012;122:213–9.
Leeman LM, Brown SA, Albright B, Skipper B, Hsi A, Rayburn WF. Association between intrapartum fetal heart rate patterns and neonatal abstinence syndrome in methadone exposed neonates. J Matern Fetal Neonatal Med. 2011;24:955–9.
Navaneethakrishnan R, Tutty S, Sinha C, Lindow S. The effect of maternal methadone use on the fetal heart pattern: a computerised CTG analysis. BJOG. 2006;113:948–50.
Salisbury AL, Coyle MG, O’Grady KE, Heil SH, Martin PR, Stine SM, et al. Fetal assessment before and after dosing with buprenorphine or methadone. Addiction. 2012;107:36–44.
Schmid M, Kuessel L, Klein K, Metz V, Fischer G, Krampl-Bettelheim E. First‐trimester fetal heart rate in mothers with opioid addiction. Addiction. 2010;105:1265–8.
Bolin BH, Escalona-Vargas D, Daily JA, Siegel ER, Lowery CL, Coker J, et al. Magnetocardiographic identification of prolonged fetal corrected QT interval in women receiving treatment for opioid use disorder. J Obstet Gynaecol Res. 2019;45:1989–96.
McLaughlin PJ. Exposure to the opioid antagonist naltrexone throughout gestation alters postnatal heart development. Neonatology. 2002;82:207–16.
Jansson LM, Dipietro JA, Velez M, Elko A, Williams E, Milio L, et al. Fetal neurobehavioral effects of exposure to methadone or buprenorphine. Neurotoxicology Teratol. 2011;33:240–3.
Hambleton MT, Reynolds EW, Sithisarn T, Traxel SJ, Patwardhan AR, Crawford TN, et al. Autonomic nervous system function following prenatal opiate exposure. Front Pediatr. 2013;1:27. https://doi.org/10.3389/fped.2013.00027.
Parikh R, Hussain T, Holder G, Bhoyar A, Ewer AK. Maternal methadone therapy increases QTc interval in newborn infants. Arch Dis Child Fetal Neonatal Ed. 2011;96:F141-3.
Jansson LM, DiPietro JA, Elko A, Velez M. Infant autonomic functioning and neonatal abstinence syndrome. Drug Alcohol Depend. 2010;109:198–204.
Schubach NE, Mehler K, Roth B, Korsch E, Laux R, Singer D, et al. Skin conductance in neonates suffering from abstinence syndrome and unexposed newborns. Eur J Pediatr. 2016;175:859–68.
Bada H, Bauer C, Shankaran S, Lester B, Wright L, Das A, et al. Central and autonomic system signs with in utero drug exposure. Arch Dis Child Fetal Neonatal Ed. 2002;87:F106–12.
Goldfarb SS, Stanwood GD, Flynn HA, Graham DL. Developmental opioid exposures: neurobiological underpinnings, behavioral impacts, and policy implications. Exp Biol Med (Maywood). 2020;245:131–7. https://doi.org/10.1177/1535370219883601.
Author information
Authors and Affiliations
Contributions
MPH wrote the systematic review protocol, supervised the search and data abstraction, and assisted with analysis, preparation, and critical review of the final manuscript. CAW and MZR executed the PRISMA search, primarily conducted included study data abstraction, and assisted with preparation and critical review of the final manuscript. WMY assisted with execution of PRISMA search and data abstraction, preparation, and critical review of the final manuscript. LAW assisted with systematic review protocol, conduction and supervision of all included databases, preparation and critical review of the final manuscript. SSO assisted by conducting meta-analysis of included studies, preparation and critical review of the final manuscript. BB and SI assisted with data abstraction of rodent studies, preparation and critical review of the final manuscript. TRK assisted by providing critical review of all extracted data, preparation and critical review of the final manuscript. SC and KKG assisted with data abstraction of studies, analysis of data extracted from included studies, preparation and critical review of the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Howell, M.P., Wiseman, C.A., Rosen, M.Z. et al. Impact of prenatal opioids on cardiac and autonomic development: systematic review and meta-analysis. J Perinatol 43, 259–270 (2023). https://doi.org/10.1038/s41372-022-01466-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01466-7