Abstract
Objective
To study the impact of an evidence-based neuroprotection care (NPC) bundle on long-term neurodevelopmental impairment (NDI) in infants born extremely premature.
Study design
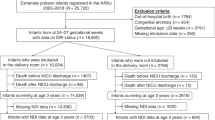
An NPC bundle targeting predefined risk factors for acute brain injury in extremely preterm infants was implemented. We compared the incidence of composite outcome of death or severe neurodevelopmental impairment (sNDI) at 21 months adjusted age pre and post bundle implementation.
Results
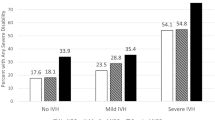
Adjusting for confounding factors, NPC bundle implementation associated with a significant reduction in death or sNDI (aOR, 0.34; 95% CI 0.17–0.68; P = 0.002), mortality (aOR, 0.31; 95% CI (0.12–0.79); P = 0.015), sNDI (aOR, 0.37; 95% CI: 0.12–0.94; P = 0.039), any motor, language, or cognitive composite score <70 (aOR, 0.48; 95% CI: 0.26–0.90; P = 0.021).
Conclusion
Implementation of NPC bundle targeting predefined risk factors is associated with a reduction in mortality or sNDI in extremely preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–F4.
Bolisetty S, Dhawan A, Abdel-Latif M, Bajuk B, Stack J, Lui K, et al. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics. 2014;133:55–62.
Gilard V, Tebani A, Bekri S, Marret S. Intraventricular hemorrhage in very preterm infants: a comprehensive review. J Clin Med. 2020;9:2447.
Ann WyP, Rettiganti M, Li J, Yap V, Barrett K, Whiteside-Mansell L, et al. Impact of intraventricular hemorrhage on cognitive and behavioral outcomes at 18 years of age in low birth weight preterm infants. J Perinatol. 2015;35:511–5.
Gilard V, Chadie A, Ferracci FX, Brasseur-Daudruy M, Proust F, Marret S, et al. Post hemorrhagic hydrocephalus and neurodevelopmental outcomes in a context of neonatal intraventricular hemorrhage: an institutional experience in 122 preterm children. BMC Pediatr. 2018;18:288.
Dolfin T, Skidmore MB, Fong KW, Hoskins EM, Shennan AT. Incidence, severity, and timing of subependymal and intraventricular hemorrhages in preterm infants born in a perinatal unit as detected by serial real-time ultrasound. Pediatrics. 1983;71:541–6.
Perlman JM, Volpe JJ. Intraventricular hemorrhage in extremely small premature infants. Am J Dis Child. 1986;140:1122–4.
Handley SC, Passarella M, Lee HC, Lorch SA. Incidence trends and risk factor variation in severe intraventricular hemorrhage across a population based cohort. J Pediatr. 2018;200:24–9.
Lee JY, Kim HS, Jung E, Kim ES, Shim GH, Lee HJ, et al. Risk factors for periventricular-intraventricular hemorrhage in premature infants. J Korean Med Sci. 2010;25:418–24.
Malusky S, Donze A. Neutral head positioning in premature infants for intraventricular hemorrhage prevention: an evidence-based review. Neonatal Netw. 2011;30:381–96.
Noori S, Anderson M, Soleymani S, Seri I. Effect of carbon dioxide on cerebral blood flow velocity in preterm infants during postnatal transition. Acta Paediatr. 2014;103:e334–9.
Puia-Dumitrescu M, Younge N, Benjamin DK, Lawson K, Hume C, Hill K, et al. Medications and in-hospital outcomes in infants born at 22-24 weeks of gestation. J Perinatol. 2020;40:781–9.
Gillam-Krakauer M, Slaughter JC, Cotton RB, Robinson BE, Reese J, Maitre NL. Outcomes in infants < 29 weeks of gestation following single-dose prophylactic indomethacin. J Perinatol. 2021;41:109–18.
Arnon S, Dolfin T, Reichman B, Regev RH, Lerner-Geva L, Boyko V, et al. Delivery room resuscitation and adverse outcomes among very low birth weight preterm infants. J Perinatol. 2017;37:1010–6.
Miller KE, Singh N. Association of multiple tracheal intubation attempts with clinical outcomes in extremely preterm infants: a retrospective single-center cohort study. J Perinatol. 2022. Online ahead of print.
Schmid MB, Reister F, Mayer B, Hopfner RJ, Fuchs H, Hummler HD. Prospective risk factor monitoring reduces intracranial hemorrhage rates in preterm infants. Dtsch Arztebl Int. 2013;110:489–96.
Pellicer A, Gaya F, Madero R, Quero J, Cabanas F. Noninvasive continuous monitoring of the effects of head position on brain hemodynamics in ventilated infants. Pediatrics. 2002;109:434–40.
de Bijl-Marcus K, Brouwer AJ, De Vries LS, Groenendaal F, Wezel-Meijler GV. Neonatal care bundles are associated with a reduction in the incidence of intraventricular haemorrhage in preterm infants: a multicentre cohort study. Arch Dis Child Fetal Neonatal Ed. 2020;105:419–24.
Gross M, Engel C, Trotter A. Evaluating the Effect of a Neonatal Care Bundle for the Prevention of Intraventricular Hemorrhage in Preterm Infants. Children (Basel). 2021;8:257.
Murthy P, Zein H, Thomas S, Scott JN, Abou Mehrem A, Esser MJ, et al. Neuroprotection care bundle implementation to decrease acute brain injury in preterm infants. Pediatr Neurol. 2020;110:42–8.
Fowlie PW, Davis PG, McGuire W. Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants. Cochrane Database Syst Rev. 2010;2010:CD000174.
Singh R, Gorstein SV, Bednarek F, Chou JH, McGowan EC, Visintainer PF. A predictive model for SIVH risk in preterm infants and targeted indomethacin therapy for prevention. Sci Rep. 2013;3:2539.
Su BH, Lin HY, Huang FK, Tsai ML, Huang YT. Circulatory management focusing on preventing intraventricular hemorrhage and pulmonary hemorrhage in preterm infants. Pediatr Neonatol. 2016;57:453–62.
Fanaroff JM, Wilson-Costello DE, Newman NS, Montpetite MM, Fanaroff AA. Treated hypotension is associated with neonatal morbidity and hearing loss in extremely low birth weight infants. Pediatrics. 2006;117:1131–5.
Greenough A, Cheeseman P, Kavvadia V, Dimitriou G, Morton M. Colloid infusion in the perinatal period and abnormal neurodevelopmental outcome in very low birth weight infants. Eur J Pediatr. 2002;161:319–23.
Abdul Aziz AN, Thomas S, Murthy P, Rabi Y, Soraisham A, Stritzke A, et al. Early inotropes use is associated with higher risk of death and/or severe brain injury in extremely premature infants. J Matern Fetal Neonatal Med. 2020;33:2751–8.
Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N. Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics. 2007;119:299–305.
Brown G. NICU noise and the preterm infant. Neonatal Netw. 2009;28:165–73.
Ranger M, Grunau RE. Early repetitive pain in preterm infants in relation to the developing brain. Pain Manag. 2014;4:57–67.
Mohammad K, Momin S, Murthy P, Zein H, Scott JN, Mehrem AA, et al. Impact of quality improvement outreach education on the incidence of acute brain injury in transported neonates born premature. J Perinatol. 2022. Online ahead of print.
Gurram Venkata SKR, Srivastava A, Murthy P, Scott JN, Zein H, Leijser L, et al. Hemodynamic quality improvement bundle to reduce the use of inotropes in extreme preterm neonates. Paediatr Drugs. 2022;24:259–67.
Lee SK, Shah PS, Singhal N, Aziz K, Synnes A, McMillan D, et al. Association of a quality improvement program with neonatal outcomes in extremely preterm infants: a prospective cohort study. CMAJ. 2014;186:E485–94.
Shah PS, Dunn M, Aziz K, Shah V, Deshpandey A, Mukerji A, et al. Sustained quality improvement in outcomes of preterm neonates with a gestational age less than 29 weeks: results from the Evidence-based Practice for Improving Quality Phase 3 (1). Can J Physiol Pharm. 2019;97:213–21.
Acknowledgements
The authors also acknowledge members of the multidisciplinary team at the Neonatal Follow-up Clinic who made this work possible.
Funding
The “Drive to Zero” IVH prevention project is a nationwide initiative funded by the Canadian Neonatal Network and Canadian Preterm Birth Network. The Neonatal Neuro-Critical Care program is funded and supported by the Alberta Children’s Hospital Research Foundation and Alberta Health Services.
Author information
Authors and Affiliations
Contributions
AB led the follow up part of the study and wrote the first draft of the manuscript, PM conceptualized and the co-led the study design and implementation, HZ conceptualized and co-led the study design and implementation, ST contributed to the study design and implementation, JNS reviewed and scored all brain images and developed the scoring system, AAM contributed to the study design and implementation, MJE contributed to the study design and implementation, AL contributed to the study design and implementation, JN contributed to the study design and implementation, ST analyzed the data, CM contributed to data collection, study design and implementation, DK contributed to the study design and implementation, LI contributed to the study design and implementation, JS to data collection and study implementation, LL contributed to the study design and implementation, KM Conceptualized and led the study design and implementation. All authors drafted manuscript, critically revised manuscript, gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benlamri, A., Murthy, P., Zein, H. et al. Neuroprotection care bundle implementation is associated with improved long-term neurodevelopmental outcomes in extremely premature infants. J Perinatol 42, 1380–1384 (2022). https://doi.org/10.1038/s41372-022-01443-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01443-0