Abstract
Objective
To assess whether either duration and magnitude of ductal shunt or medical treatment for patent ductus arteriosus (PDA) are related to spontaneous intestinal perforation (SIP).
Study design
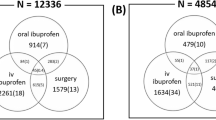
Clinical charts of infants <29 weeks’ gestation born from 2006 to 2018 were reviewed. Echocardiographic examinations were evaluated according to McNamara and Sehgal’s staging system.
Results
A higher percentage of patients with SIP had a hemodynamically significant PDA (HSPDA) and was treated with either NSAIDs or paracetamol (79% vs 53% and 81% vs 54%, respectively). Among non-treated patients, we found a 1.32 increase in the odds of SIP per day of persistence of HSPDA. In the cohort of patients treated despite the absence of HSPDA, we found a 2.35 increase in the odds of SIP per dose of drug administered.
Conclusion
Both treating a non-HSPDA and leaving a HSPDA to its natural history seem to be associated with SIP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Aschner JL, Deluga KS, Metlay LA, Emmens RW, Hendricks-Munoz KD. Spontaneous focal gastrointestinal perforation in very low birth weight infants. J Pediatr. 1988;113:364–7.
Gordon PV. Understanding intestinal vulnerability to perforation in the extremely low birth weight infant. Pediatr Res. 2009;65:138–44.
Buchheit JQ, Stewart DL. Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics. 1994;93:32–6.
Gordon PV, Attridge JT. Understanding clinical literature relevant to spontaneous intestinal perforations. Am J Perinatol. 2009;26:309–16.
Novack CM, Waffarn F, Sills JH, Pousti TJ, Warden MJ, Cunningham MD. Focal intestinal perforation in the extremely-low-birth-weight infant. J Perinatol. 1994;14:450–3.
Okuyama H, Kubota A, Oue T, Kuroda S, Ikegami R, Kamiyama M. A comparison of the clinical presentation and outcome of focal intestinal perforation and necrotizing enterocolitis in very-low-birth-weight neonates. Pediatr Surg Int. 2002;18:704–6.
Vongbhavit K, Underwood MA. Intestinal perforation in the premature infant. J Neonatal Perinat Med. 2017;10:281–9.
Pumberger W, Mayr M, Kohlhauser C, Weninger M. Spontaneous localized intestinal perforation in very-low-birth-weight infants: A distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg. 2002;195:796–803.
Wadhawan R, Oh W, Hintz SR, Blakely ML, Das A, Bell EF, et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol. 2014;34:64–70.
Wadhawan R, Oh W, Vohr BR, Saha S, Das A, Bell EF, et al. Spontaneous intestinal perforation in extremely low birth weight infants: association with indometacin therapy and effects on neurodevelopmental outcomes at 18-22 months corrected age. Arch Dis Child Fetal Neonatal Ed. 2013;98:F127–32.
Sehgal A, McNamara PJ. The ductus arteriosus: a refined approach! Semin Perinatol. 2012;36:105–13.
Benitz WE. Treatment of persistent patent ductus arteriosus in preterm infants: time to accept the null hypothesis. J Perinatol. 2010;30:241–52.
El-Khuffash A, Weisz DE, McNamara PJ. Reflections of the changes in patent ductus arteriosus management during the last 10 years. Arch Dis Child Fetal Neonatal Ed. 2016;101:F474–8.
Sehgal A, McNamara PJ. Does echocardiography facilitate determination of hemodynamic significance attributable to the ductus arteriosus? Eur J Pediatr. 2009;168:907–14.
Attridge JT, Clark R, Walker MW, Gordon PV. New insights into spontaneous intestinal perforation using a national data set: (1) SIP is associated with early indomethacin exposure. J Perinatol. 2006;26:93–9.
Bloom B. Attridge et al. present an analysis of a complex data set, which offers important confirmation of the differences between the clinical presentation of spontaneous intestinal perforations (SIP) and surgical necrotizing enterocolitis (NEC). J Perinatol. 2006;26:384–6.
Fujii AM, Brown E, Mirochnick M, O’Brien S, Kaufman G. Neonatal necrotizing enterocolitis with intestinal perforation in extremely premature infants receiving early indomethacin treatment for patent ductus arteriosus. J Perinatol. 2002;22:535–40.
Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S, et al. Long-term effects of indomethacin prophylaxis. N. Engl J Med. 2001;344:1966–72.
Sharma R, Hudak ML, Tepas JJ, Wludyka PS, Teng RJ, Hastings LK, et al. Prenatal or postnatal indomethacin exposure and neonatal gut injury associated with isolated intestinal perforation and necrotizing enterocolitis. J Perinatol. 2010;30:786–93.
Stark A, Carlo W, Tyson J, Papile L, Wright L, Shankaran S, et al. Adverse effects of early dexamethasone treatment in extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N. Engl J Med. 2001;344:95–101.
Watterberg KL, Gerdes JS, Cole CH, Aucott SW, Thilo EH, Mammel MC, et al. Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics. 2004;114:1649–57.
Gournay V, Roze JC, Kuster A, Daoud P, Cambonie G, Hascoet JM, et al. Prophylactic ibuprofen versus placebo in very premature infants: a randomised, double-blind, placebo-controlled trial. Lancet. 2004;364:1939–44.
Kelleher J, Salas AA, Bhat R, Ambalavanan N, Saha S, Stoll BJ, et al. Prophylactic indomethacin and intestinal perforation in extremely low birth weight infants. Pediatrics. 2014;134:e1369–77.
Mitra S, Florez ID, Tamayo ME, Mbuagbaw L, Vanniyasingam T, Veroniki AA, et al. Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm infants a systematic review and meta-analysis. JAMA. 2018;319:1221–38.
Marconi E, Bettiol A, Ambrosio G, Perduca V, Vannacci A, Troiani S, et al. Efficacy and safety of pharmacological treatments for patent ductus arteriosus closure: a systematic review and network meta-analysis of clinical trials and observational studies. Pharm Res. 2019;148:104418.
Ohlsson A, Shah PS. Paracetamol (acetaminophen) for patent ductus arteriosus in preterm or low-birth-weight infants. Cochrane Database Syst Rev. 2018;4:CD010061. https://doi.org/10.1002/14651858.CD010061.pub3.
Shepherd JL, Noori S. What is a hemodynamically significant PDA in preterm infants? Congenit Heart Dis. 2019;14:21–6.
McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed. 2007;92:424–7.
Schena F, Francescato G, Cappelleri A, Picciolli I, Mayer A, Mosca F, et al. Association between hemodynamically significant patent ductus arteriosus and bronchopulmonary dysplasia. J Pediatr. 2015;166:1488–92.
Rao R, Bryowsky K, Mao J, Bunton D, McPherson C, Mathur A. Gastrointestinal complications associated with ibuprofen therapy for patent ductus arteriosus. J Perinatol. 2011;31:465–70.
van Laere D, van Overmeire B, Gupta S, El Khuffash A, Savoia M, McNamara PJ, et al. Application of NPE in the assessment of a patent ductus arteriosus. Pediatr Res. 2018;84:46–56.
O’Rourke DJ, El-Khuffash A, Moody C, Walsh K, Molloy EJ. Patent ductus arteriosus evaluation by serial echocardiography in preterm infants. Acta Paediatr. 2008;97:574–8.
El-Khuffash A, Barry D, Walsh K, Davis PG, Molloy EJ. Biochemical markers may identify preterm infants with a patent ductus arteriosus at high risk of death or severe intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 2008;93:F407–12.
El-Khuffash AF, Amoruso M, Culliton M, Molloy EJ. N-terminal pro-B-type natriuretic peptide as a marker of ductal haemodynamic significance in preterm infants: a prospective observational study. Arch Dis Child Fetal Neonatal Ed. 2007;92:F421–2.
Chock VY, Rose LA, Mante JV, Punn R. Near-infrared spectroscopy for detection of a significant patent ductus arteriosus. Pediatr Res. 2016;80:675–80.
Arman D, Sancak S, Gürsoy T, Topcuoğlu S, Karatekin G, Ovalı F. The association between NIRS and Doppler ultrasonography in preterm infants with patent ductus arteriosus. J Matern Neonatal Med. 2020;33:1245–52.
Lee JA. Practice for preterm patent ductus arteriosus; focusing on the hemodynamic significance and the impact on the neonatal outcomes. Korean J Pediatr. 2019;62:245–51.
Gursoy T, Hayran M, Derin H, Ovali F. A clinical scoring system to predict the development of bronchopulmonary dysplasia. Am J Perinatol. 2014;32:659–65.
El-Khuffash AF, Slevin M, McNamara PJ, Molloy EJ. Troponin T, N-terminal pro natriuretic peptide and a patent ductus arteriosus scoring system predict death before discharge or neurodevelopmental outcome at 2 years in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2011;96:133–8.
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN, et al. A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr. 2015;167:1354–61.
Sehgal A, Paul E, Menahem S. Functional echocardiography in staging for ductal disease severity: role in predicting outcomes. Eur J Pediatr. 2013;172:179–84.
Wyllie JP, Gupta S. Prophylactic and early targeted treatment of patent ductus arteriosus. Semin Fetal Neonatal Med. 2018;23:250–4.
Jasani B, Weisz DE, McNamara PJ. Evidence-based use of acetaminophen for hemodynamically significant ductus arteriosus in preterm infants. Semin Perinatol. 2018;42:243–52.
Meyer CL, Payne NR, Roback SA. Spontaneous, isolated intestinal perforations in neonates with birth weight <1,000 g not associated with necrotizing enterocolitis. J Pediatr Surg. 1991;26:714–7.
Adderson EE, Pappin A, Pavia AT. Spontaneous intestinal perforation in premature infants: a distinct clinical entity associated with systemic candidiasis. J Pediatr Surg. 1998;33:1463–7.
Author information
Authors and Affiliations
Contributions
AM, GF, NP, FS and FM contributed to the conception and the design of the manuscript. AM collected the data retrospectively. AM, NP and FS performed statistical analysis. AM and GF wrote the first draft of the manuscript. All authors contributed to manuscript critical revision, read and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mayer, A., Francescato, G., Pesenti, N. et al. Patent ductus arteriosus and spontaneous intestinal perforation in a cohort of preterm infants. J Perinatol 42, 1649–1653 (2022). https://doi.org/10.1038/s41372-022-01403-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01403-8
This article is cited by
-
Transcatheter closure in preterm infants with patent ductus arteriosus: feasibility, results, hemodynamic monitoring and future prospectives
Italian Journal of Pediatrics (2023)
-
Nutrition of the preterm infant with persistent ductus arteriosus: existing evidence and practical implications
Pediatric Research (2023)
-
Fluid restriction in management of patent ductus arteriosus in Italy: a nationwide survey
European Journal of Pediatrics (2022)