Abstract
Objective
To compare treatment failure between: (1) infants treated with phenobarbital versus levetiracetam for first-line treatment and (2) infants treated with phenytoin versus levetiracetam for second-line treatment following phenobarbital.
Study design
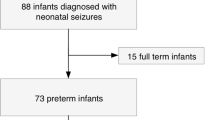
This retrospective cohort study included infants with seizures receiving phenobarbital or levetiracetam as the initial anti-seizure medication. Treatment failure was defined as the need for additional anti-seizure medication within 24–72 h and compared using mixed-effect logistic regression after adjustment for confounding factors, including center.
Results
In this cohort of 6842 infants, the incidence of treatment failure was 31% vs. 38% in infants receiving first-line phenobarbital versus levetiracetam (adjusted OR: 0.70; 95% CI 0.58–0.84). There was no significant difference in second-line treatment failure (adjusted OR: 1.31; 95% CI 0.92–1.86).
Conclusions
First-line treatment of neonatal seizures with phenobarbital is associated with a lower rate of treatment failure than levetiracetam. There was no significant difference in second-line treatment failure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
16 December 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41372-021-01285-2
References
El-Dib M, Soul JS. The use of phenobarbital and other anti-seizure drugs in newborns. Semin Fetal Neonatal Med. 2017;22:321–7.
Ahmad K, Desai S, Bennett M, Ahmad S, Ng Y, Clark R, et al. Changing antiepileptic drug use for seizures in US neonatal intensive care units from 2005 to 2014. J Perinatol. 2017;37:296–300.
Le VT, Abdi HH, Sánchez PJ, Yossef L, Reagan PB, Slaughter LA, et al. Neonatal Antiepileptic Medication Treatment Patterns: A Decade of Change. Am J Perinatol. 2021;38:469–76.
Dizon ML, Rao R, Hamrick SE, Zaniletti I, DiGeronimo R, Natarajan G, et al. Practice variation in anti-epileptic drug use for neonatal hypoxic-ischemic encephalopathy among regional NICUs. BMC Pediatrics. 2019;19:67.
Bartha AI, Shen J, Katz KH, Mischel RE, Yap KR, Ivacko JA, et al. Neonatal seizures: Multicenter variability in current treatment practices. Pediatr Neurol. 2007;37:85–90.
Glass HC, Kan J, Bonifacio SL, Ferriero DM. Neonatal seizures: Treatment practices among term and preterm infants. Pediatr Neurol. 2012;46:111–5.
Hellstrom-Westas L, Boylan G, Agren J. Systematic review of neonatal seizure management strategies provides guidance on anti-epileptic treatment. Acta Paediatr. 2015;104:123–9.
Painter MJ, Scher MS, Stein AD, Armatti S, Wang Z, Gardiner JC, et al. Phenobarbital compared with phenytoin for the treatment of neonatal seizures. N. Engl J Med. 1999;341:485–9.
Gilman JT, Gal P, Duchowny MS, Weaver RL, Ransom JL. Rapid sequential phenobarbital treatment of neonatal seizures. Pediatrics 1989;83:674–8.
Bittigau P, Sifringer M, Genz K, Reith E, Pospischil D, Govindarajalu S, et al. Antiepileptic drugs and apoptotic neurodegeneration in the developing brain. Proc Natl Acad Sci USA. 2002;99:15089–94.
Forcelli PA, Kim J, Kondratyev A, Gale K. Pattern of antiepileptic drug-induced cell death in limbic regions of the neonatal rat brain. Epilepsia 2011;52:e207–11.
Kaushal S, Tamer Z, Opoku F, Forcelli PA. Anticonvulsant drug-induced cell death in the developing white matter of the rodent brain. Epilepsia 2016;57:727–34.
McHugh DC, Lancaster S, Manganas LN. A systematic review of the efficacy of levetiracetam in neonatal seizures. Neuropediatrics 2018;49:12–7.
Rao LM, Hussain SA, Zaki T, Cho A, Chanlaw T, Garg M, et al. A comparison of levetiracetam and phenobarbital for the treatment of neonatal seizures associated with hypoxic-ischemic encephalopathy. Epilepsy Behav. 2018;88:212–7.
Abend NS, Gutierrez-Colina AM, Monk HM, Dlugos DJ, Clancy RR. Levetiracetam for treatment of neonatal seizures. J Child Neurol. 2011;26:465–70.
Aceves J, Khan O, Mungall D, Fonkem E, Wright CC, Wenner A, et al. Efficacy and tolerability of intravenous levetiracetam in children. Front Neurol. 2013;4:120.
Gowda VK, Romana A, Shivanna NH, Benakappa N, Benakappa A. Levetiracetam versus phenobarbitone in neonatal seizures—A randomized controlled trial. Indian Pediatrics. 2019;56:643–6.
Khan O, Cipriani C, Wright C, Crisp E, Kirmani B. Role of intravenous levetiracetam for acute seizure management in preterm neonates. Pediatr Neurol. 2013;49:340–3.
Sharpe C, Reiner GE, Davis SL, Nespeca M, Gold JJ, Rasmussen M, et al. Levetiracetam Versus Phenobarbital for Neonatal Seizures: A Randomized Controlled Trial. Pediatrics. 2020;145.
Penner H, Hariharan G. Comparative efficacy of levetiracetam to phenobarbital in the treatment of neonatal seizures. Acta Paediatr. 2021;110:2287–8.
Ahrens S, Ream MA, Slaughter LA. Status epilepticus in the neonate: Updates in treatment strategies. Curr Treat Options Neurol. 2019;21:8.
Khan O, Chang E, Cipriani C, Wright C, Crisp E, Kirmani B. Use of intravenous levetiracetam for management of acute seizures in neonates. Pediatr Neurol. 2011;44:265–9.
Furwentsches A, Bussmann C, Ramantani G, Ebinger F, Philippi H, Poschl J, et al. Levetiracetam in the treatment of neonatal seizures: A pilot study. Seizure 2010;19:185–9.
Grinspan ZM, Shellhaas RA, Coryell J, Sullivan JE, Wirrell EC, Mytinger JR, et al. Comparative effectiveness of levetiracetam vs phenobarbital for infantile epilepsy. JAMA Pediatrics. 2018;172:352–60.
Boylan G, Rennie J, Chorley G, Pressler R, Fox G, Farrer K, et al. Second-line anticonvulsant treatment of neonatal seizures: A video-EEG monitoring study. Neurology 2004;62:486–8.
Shany E, Benzaquen O, Friger M, Richardson J, Golan A. Influence of antiepileptic drugs on amplitude-integrated electroencephalography. Pediatr Neurol. 2008;39:387–91.
Maitre NL, Smolinsky C, Slaughter JC, Stark AR. Adverse neurodevelopmental outcomes after exposure to phenobarbital and levetiracetam for the treatment of neonatal seizures. J Perinatol. 2013;33:841–6.
Arican P, Dundar NO, Atasever NM, Inal MA, Gencpinar P, Cavusoglu D, et al. Comparison of the neurocognitive outcomes in term infants treated with levetiracetam and phenobarbital monotherapy for neonatal clinical seizures. Seizure 2020;80:71–4.
Author contributions
ES contributed to the study design and data interpretation, drafted the primary manuscript and subsequent revisions, and approved the final version of the manuscript. SH contributed to the study design and data interpretation, critically reviewed all drafts of the manuscript, and approved the final version of the manuscript. RP contributed to the study design and data interpretation, critically reviewed all drafts of the manuscript, and approved the final version of the manuscript. MB completed the data analysis, critically reviewed all drafts of the manuscript, and approved the final version of the manuscript. VT contributed to the study design, data acquisition, and data interpretation, critically reviewed all drafts of the manuscript, and approved the final version of the manuscript. KA contributed to the study design, data acquisition, and data interpretation, critically reviewed all drafts of the manuscript, and approved the final version of the manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The Supplementary information was corrected and a second table was added.
Supplementary information
Rights and permissions
About this article
Cite this article
Sewell, E.K., Hamrick, S.E.G., Patel, R.M. et al. Association between anti-seizure medication and outcomes in infants. J Perinatol 42, 359–364 (2022). https://doi.org/10.1038/s41372-021-01240-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01240-1