Abstract
Objective
To identify risk factors associated with high-frequency ventilation (HFV) following definitive closure of the patent ductus arteriosus (PDA).
Methods
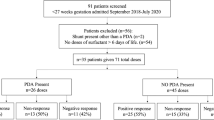
We performed a retrospective study of premature infants (<37 weeks) who were mechanically ventilated before and after surgical or transcatheter PDA closure. Primary outcome was HFV requirement within 24 h of procedure. Logistic regression was used to estimate clinical associations with post procedure HFV requirement.
Results
We identified 110 infants who were mechanically ventilated before PDA closure, of which 48 (44%) escalated to HFV within 24 h after closure. In the multivariable model, surgical ligation (OR 21.5, 95% CI 1.6–284), elevated Respiratory Severity Score (RSS) 1 h post-procedure (OR 1.78, 95% CI 1.07–2.99) and 12 h post-procedure (OR 2.12, 95% CI 1.37–3.26) were independent predictors of HFV.
Conclusion
Surgical ligation and elevated RSS values over the first 12 h after PDA closure are risk factors for HFV.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rios DR, Bhattacharya S, Levy PT, McNamara PJ. Circulatory insufficiency and hypotension related to the ductus arteriosus in neonates. Front Pediatr. 2018;6:62.
Serrano RM, Madison M, Lorant D, Hoyer M, Alexy R. Comparison of ‘post-patent ductus arteriosus ligation syndrome’ in premature infants after surgical ligation vs. percutaneous closure. J Perinatol. 2020;40:324–9.
Nealon E, Rivera BK, Cua CL, Ball MK, Stiver C, Boe BA, et al. Follow-up after Percutaneous Patent Ductus Arteriosus Occlusion in Lower Weight Infants. J Pediatr: Elsevier Inc; 2019. pp. 144–50.e143.
Willson DF, Thomas NJ, Markovitz BP, Bauman LA, DiCarlo JV, Pon S, et al. Effect of exogenous surfactant (calfactant) in pediatric acute lung injury: a randomized controlled trial. JAMA. 2005;293:470–6.
Stewart DL, Dela Cruz TV, Duncan SD, Cook LN. Response to high frequency jet ventilation may predict the need for extracorporeal membrane oxygenation. Eur Respir J. 1996;9:1257–60.
Golombek SG, Young JN. Efficacy of inhaled nitric oxide for hypoxic respiratory failure in term and late preterm infants by baseline severity of illness: a pooled analysis of three clinical trials. Clin Ther. 2010;32:939–48.
Shahid S, Dutta S, Symington A, Shivananda S, McMaster University N. Standardizing umbilical catheter usage in preterm infants. Pediatrics. 2014;133:e1742–1752.
de Brito CS, de Brito DV, Abdallah VO, Gontijo, Filho PP. Occurrence of bloodstream infection with different types of central vascular catheter in critically neonates. J Infect. 2010;60:128–32.
Deindl P, Waldhor T, Unterasinger L, Berger A, Keck M. Arterial catheterisation in neonates can result in severe ischaemic complications but does not impair long-term extremity function. Acta Paediatr. 2018;107:240–8.
Iyer NP, Mhanna MJ. Non-invasively derived respiratory severity score and oxygenation index in ventilated newborn infants. Pediatric Pulmonol. 2013;48:364–9.
Malkar MB, Gardner WP, Mandy GT, Stenger MR, Nelin LD, Shepherd EG, et al. Respiratory severity score on day of life 30 is predictive of mortality and the length of mechanical ventilation in premature infants with protracted ventilation. Pediatric Pulmonol. 2015;50:363–9.
Seo YM, Sung IK, Yum SK. Risk factors associated with prolonged mechanical ventilation after surgical patent ductus arteriosus ligation in preterm infants. J Matern Fetal Neonatal Med. 2020;8:1–8.
Ting JY, Resende M, More K, Nicholls D, Weisz DE, El-Khuffash A, et al. Predictors of respiratory instability in neonates undergoing patient ductus arteriosus ligation after the introduction of targeted milrinone treatment. J Thoracic Cardiovasc Surg. 2016;152:498–504.
Hsu KH, Wong P, Ram Kumar S, Evans J, Noori S. Predictors of respiratory improvement 1 week after ligation of patent ductus arteriosus in preterm infants. J Pediatr. 2019;205:49–54 e42.
Francis JV, Padmanabhan S, Jaques L, Courtot J, Sehgal A. Respiratory and cardiovascular morbidity in the first 48 h post surgical ligation of the patent ductus arteriosus. J Neonatal-Perinatal Med. 2011;4:21–6.
Philip R, Waller BR, Chilakala S, Graham B, Stecchi N, Apalodimas L, et al. Hemodynamic and clinical consequences of early versus delayed closure of patent ductus arteriosus in extremely low birth weight infants. J Perinatol. 2021;41:100–8.
Rodriguez Ogando A, Planelles Asensio I, de la Blanca ARS, Ballesteros Tejerizo F, Sanchez Luna M, Gil Jaurena JM, et al. Surgical ligation versus percutaneous closure of patent ductus arteriosus in very low-weight preterm infants: which are the real benefits of the percutaneous approach? Pediatric Cardiol. 2018;39:398–410.
Regan W, Benbrik N, Sharma SR, Auriau J, Bouvaist H, Bautista-Rodriguez C, et al. Improved ventilation in premature babies after transcatheter versus surgical closure of patent ductus arteriosus. Int J Cardiol. 2020;311:22–7.
Schwartz MC, Nykanen D, Winner LH, Perez J, McMahan M, Munro HM, et al. Transcatheter patent ductus arteriosus occlusion in small infants. Congenit Heart Dis. 2016;11:647–55.
Sathanandam S, Balduf K, Chilakala S, Washington K, Allen K, Knott-Craig C, et al. Role of Transcatheter patent ductus arteriosus closure in extremely low birth weight infants. Catheter Cardiovasc Interv. 2019;93:89–96.
Abu Hazeem AA, Gillespie MJ, Thun H, Munson D, Schwartz MC, Dori Y, et al. Percutaneous closure of patent ductus arteriosus in small infants with significant lung disease may offer faster recovery of respiratory function when compared to surgical ligation. Catheter Cardiovasc Interv. 2013;82:526–33.
Ulrich TJB, Hansen TP, Reid KJ, Bingler MA, Olsen SL. Post-ligation cardiac syndrome is associated with increased morbidity in preterm infants. J Perinatol. 2018;38:537–42.
Harting MT, Blakely ML, Cox CS Jr., Lantin-Hermoso R, Andrassy RJ, Lally KP. Acute hemodynamic decompensation following patent ductus arteriosus ligation in premature infants. J Invest Surg. 2008;21:133–8.
Clyman RI, Wickremasinghe A, Merritt TA, Solomon T, McNamara P, Jain A, et al. Hypotension following patent ductus arteriosus ligation: the role of adrenal hormones. J Pediatr. 2014;164:1449–55 e1441.
Jain A, Sahni M, El-Khuffash A, Khadawardi E, Sehgal A, McNamara PJ. Use of targeted neonatal echocardiography to prevent postoperative cardiorespiratory instability after patent ductus arteriosus ligation. J Pediatr. 2012;160:584–9 e581.
Wheeler CR, Stephens H, O’Donnell I, Zurakowski D, Smallwood CD. Mortality risk factors in preterm infants treated with high-frequency jet ventilation. Respiratory Care. 2020;65:1631–40.
Wheeler CR, Smallwood CD, O’Donnell I, Gagner D, Sola-Visner MC. Assessing initial response to high-frequency jet ventilation in premature infants with hypercapnic respiratory failure. Respiratory Care. 2017;62:867–72.
Sathanandam SK, Gutfinger D, O’Brien L, Forbes TJ, Gillespie MJ, Berman DP, et al. Amplatzer Piccolo Occluder clinical trial for percutaneous closure of the patent ductus arteriosus in patients ≥700 grams. Catheter Cardiovasc Interv. 2020;96:1–11.
Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression, Third edition/edn. Wiley: Hoboken, New Jersey, 2013.
Zhou X-h, McClish DK, Obuchowski NA. Statistical methods in diagnostic medicine, 2nd edn. Wiley: Hoboken, N.J., 2011.
Staffa SJ, Zurakowski D. Statistical power and sample size calculations: A primer for pediatric surgeons. J Pediatr Surg: Elsevier Inc.; 2020. pp. 1173–9.
Hamrick SEG, Sallmon H, Rose AT, Porras D, Shelton EL, reese J, et al. Patent Ductus Arteriosus of the Preterm Infant. Pediatrics; 2020. pp. 1–17.
Shah SI, Aboudi D, La Gamma EF, Brumberg HL. Respiratory Severity Score greater than or equal to 2 at birth is associated with an increased risk of mortality in infants with birth weights less than or equal to 1250 g. Pediatric Pulmonol. 2020;55:3304–11.
Indrani B, Anirudha D, Marc C, Hany A. Predicting outcomes of mechanically ventilated premature infants using respiratory severity score. Taylor & Francis; 2020. pp. 1–9.
Jung YH, Jang J, Kim H-S, Shin SH, Choi CW, Kim E-K, et al. Respiratory severity score as a predictive factor for severe bronchopulmonary dysplasia or death in extremely preterm infants. BMC Pediatrics; 2019;28:1–8.
Malkar MB, Gardner WP, Mandy GT, Stenger MR, Nelin LD, Shepherd EG, et al. Respiratory Severity Score on Day of Life 30 is Predictive of Mortality and the Length of Mechanical Ventilation in Premature Infants With Protracted Ventilation. Pediatric Pulmonol; 2015;140:363–9.
Teixeira LS, Shivananda SP, Stephens D, Van Arsdell G, McNamara PJ. Postoperative cardiorespiratory instability following ligation of the preterm ductus arteriosus is related to early need for intervention. J Perinatol. 2008;28:803–10.
McNamara PJ, Stewart L, Shivananda SP, Stephens D, Sehgal A. Patent ductus arteriosus ligation is associated with impaired left ventricular systolic performance in premature infants weighing less than 1000 g. J Thorac Cardiovasc Surg. 2010;140:150–7.
Noori S, Friedlich P, Seri I, Wong P. Changes in myocardial function and hemodynamics after ligation of the ductus arteriosus in preterm infants. J Pediatr. 2007;150:597–602.
Giesinger RE. Impaired right ventricular function is associated with adverse outcome following hypoxic ischemic encephalopathy. Am J Respir Crit Care Med. 2019. pp. 1–48.
Halliday M, Kavarana M, Ebeling M, Kiger J. Milrinone use for hemodynamic instability in patent ductus arteriosus ligation. J Matern Fetal Neonatal Med. 2017;30:529–33.
Moin F, Kennedy KA, Moya FR. Risk factors predicting vasopressor use after patent ductus arteriosus ligation. Amer J Perinatol. 2003;43:313–20.
Natarajan G, Chawla S, Aggarwal S. Short-term outcomes of patent ductus arteriosus ligation in preterm neonates: reason for concern? Amer J Perinatol. 2010;150:431–7.
Naik-Mathuria B, Chang S, Fitch ME, Westhoff J, Brandt ML, Ayres NA, et al. Patent ductus arteriosus ligation in neonates: preoperative predictors of poor postoperative outcomes. J Pediatr Surg. 2008;140:1100–5.
McNamara PJ, Stewart L, Shivananda SP, Stephens D, Sehgal A. Patent ductus arteriosus ligation is associated with impaired left ventricular systolic performance in premature infants weighing less than 1000 g. J Thorac Cardiovasc Surg. 2010;162:150–7.
Townsel CD, Emmer SF, Campbell WA, Hussain N. Gender differences in respiratory morbidity and mortality of preterm neonates. Front Pediatr. 2017;5:6.
EL-Khuffash AF, Jain A, McNamara PJ. Ligation of the patent ductus arteriosus in preterm infants: understanding the physiology. J Pediatr. 2013;40:1100–6.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–55.
Clyman RI, Hills NK. The effect of prolonged tracheal intubation on the association between patent ductus arteriosus and bronchopulmonary dysplasia (grades 2 and 3). J Perinatol. 2020;40:1358–65.
Clyman RI, Hills NK, Liebowitz M, Johng S. Relationship between duration of infant exposure to a moderate-to-large patent ductus arteriosus shunt and the risk of developing bronchopulmonary dysplasia or death before 36 weeks. Am J Perinatol. 2020;37:216–23.
Author information
Authors and Affiliations
Contributions
CRW and PTL devised the study protocol and analysis plan which was approved by all authors. DG, HS, and AK collected data. DZ provided expert assistance with statistical analysis and interpretation. JCI, KGF, RC and DP provided anesthesia, cardiology and procedural expertise. All of the listed authors made substantial contributions either to the conception of the study, data acquisition, analysis and interpretation of data. CRW and PTL wrote the first draft, but all listed authors critically revised it for intellectual content and approved the final version of the manuscript and have agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wheeler, C.R., Gagner, D., Stephens, H. et al. Phenotyping respiratory decompensation following definitive closure of the patent ductus arteriosus in preterm infants. J Perinatol 42, 649–654 (2022). https://doi.org/10.1038/s41372-021-01226-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01226-z