Abstract
Objective
About 40–50% of parents with children admitted to Neonatal Intensive Care Units (NICU) experience clinically significant levels of depression, anxiety, and trauma. Poor parental mental health can negatively influence parent–child interactions and child development. Therefore, early identification of parents at-risk for clinical distress is of paramount importance.
Methods
To address this need, the psychosocial team, including psychology and psychiatry, at a large, level 4 Neonatal Intensive Care Unit (NICU) developed a quality-improvement initiative to assess the feasibility of screening parents and to determine rates of depression and trauma in the unit.
Results
About 40% of mothers and 20% of fathers were screened between 2 weeks of their child’s hospitalization. About 40–45% of those parents endorsed clinically significant levels of depression and anxiety symptoms.
Conclusions
Recommendations for enhancing the feasibility and effectiveness of this process are discussed and considerations for future clinical and research endeavors are introduced.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
March of Dimes Perinatal Data Center. Special care nursery admissions. 2011. http://www.marchofdimes.com/peristats/pdfdocs/nicu_summary_final.pdf.
Harrison W, Goodman D. Epidemiologic trends in neonatal intensive care, 2007–2012. JAMA Pediatr. 2015;169:855–62.
Geller PA, Bonacquisti A, Patterson CA. Maternal experience of neonatal intensive care unit hospitalization: trauma exposure and psychosocial responses. In: Muzik and Rosenblum, editors. Motherhood in the Face of Trauma. Cham: Springer; 2018. p. 227–47.
Grunberg VA, Geller PA, Bonacquisti A, Patterson CA. NICU infant health severity and family outcomes: a systematic review of assessments and findings in psychosocial research. J Perinatol. 2019;39:156–72.
Woodward LJ, Bora S, Clark CA, Montgomery-Hönger A, Pritchard VE, Spencer C, et al. Very preterm birth: maternal experiences of the neonatal intensive care environment. J Perinatol. 2014;34:555–61.
Arnold L, Sawyer A, Rabe H, Abbott J, Gyte G, Duley L, et al. Parents’ first moments with their very preterm babies: a qualitative study. BMJ Open. 2013;3:e002487.
Hynan MT, Mounts KO, Vanderbilt DL. Screening parents of high-risk infants for emotional distress: rationale and recommendations. J Perinatol. 2013;33:748–53.
Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). J Clin Psychol Med Settings. 2010;17:230–7.
Mackley AB, Locke RG, Spear ML, Joseph R. Forgotten parent: NICU paternal emotional response. Adv Neonatal Care. 2010;10:200–3.
Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: a preliminary study. J Dev Behav Pediatr. 2009;30:50–6.
Hoffman C, Dunn D, Njoroge WFM. Impact of postpartum upon infant development. Curr Psychiatry Rep. 2017;19:100. https://doi.org/10.1007/s11920-017-0857-8.
Holditch‐Davis D, Schwartz T, Black B, Scher M. Correlates of mother–premature infant interactions. Res Nurs Health. 2007;30:333–46.
Zelkowitz P, Feeley N, Shrier I, Stremler R, Westreich R, Dunkley D, et al. The cues and care randomized controlled trial of a neonatal intensive care unit intervention: effects on maternal psychological distress and mother-infant interaction. J Dev Behav Pediatr. 2011;32:591–9.
Grunau RE, Whitfield MF, Petrie-Thomas J, Synnes AR, Cepeda IL, Keidar A, et al. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain. 2009;143:138–46.
Zhang R, Huang RW, Gao XR, Peng XM, Zhu LH, Rangasamy R, et al. Involvement of parents in the care of preterm infants: A pilot study evaluating a family-centered care intervention in a Chinese neonatal ICU. Pediatr Crit Care Med. 2018;19:741–7.
Segers E, Ockhuijsen H, Baarendse P, van Eerden I, van den Hoogen A. The impact of family centered care interventions in a neonatal or pediatric intensive care unit on parents’ satisfaction and length of stay: a systematic review. Intensive Crit Care Nurs. 2019;50:63–70.
Cherry AS, Blucker RT, Thornberry TS, Hetherington C, McCaffree MA, Gillaspy SR. Postpartum depression screening in the neonatal intensive care unit: Program development, implementation, and lessons learned. J Multidiscip Healthc. 2016;9:59–67.
Hynan MT, Steinberg Z, Baker L, Cicco R, Geller PA, Lassen S, et al. Recommendations for mental health professionals in the NICU. J Perinatol. 2015;35:S14–8.
Moreyra A, Dowtin LL, Ocampo M, Perez E, Borkovi TC, Wharton E, et al. Implementing a standardized screening protocol for parental depression, anxiety, and PTSD symptoms in the Neonatal Intensive Care Unit. Early Hum Dev. 2021;154:105279.
Mounts KO. Screening for maternal depression in the neonatal ICU. Clin Perinatol. 2009;36:137–52.
Cole JC, Olkkola M, Zarrin HE, Berger K, Moldenhauer JS. Universal postpartum mental health screening for parents of newborns with prenatally diagnosed birth defects. J Obstet Gynecol Neonatal Nurs. 2018;47:84–93.
Hall SL, Ryan DJ, Beatty J, Grubbs L. Recommendations for peer-to-peer support for NICU parents. J Perinatol. 2015;35:S9–13.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Lee A, Chokkanathan S. Factor structure of the 10‐item CES‐D scale among community dwelling older adults in Singapore. Int J Geriatr Psychiatry. 2008;23:592–7.
Weiss DS. The impact of event scale: revised. In: Wilson and Tang, editors. Cross-cultural assessment of psychological trauma and PTSD. Boston: Springer; 2007. p. 219–38.
Joseph S. Psychometric evaluation of Horowitz’s Impact of Event Scale: a review. J Trauma Stress. 2000;13:101–13.
Barry LM, Singer GH. Reducing maternal psychological distress after the NICU experience through journal writing. J Early Intervention. 2001;24:287–97.
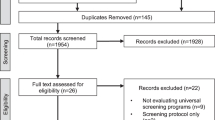
Murthy S, Haeusslein L, Bent S, Fitelson E, Franck LS, Mangurian C. Feasibility of universal screening for postpartum mood and anxiety disorders among caregivers of infants hospitalized in NICUs: a systematic review. J Perinatol. 2021;41:1–14.
Hall EM, Shahidullah JD, Lassen SR. Development of postpartum depression interventions for mothers of premature infants: a call to target low-SES NICU families. J Perinatol. 2020;40:1–9.
Shorey S, Chee CY, Ng ED, Chan YH, San Tam WW, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. 2018;104:235–48.
Scarff JR. Postpartum depression in men. Innov Clin Neurosci. 2019;16:5–6.
Centers for Disease Control and Prevention. National Center for Health Statistics Birth Data. https://www.cdc.gov/nchs/nvss/births.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fnchs%2Fbirths.htm.
Segre LS, O’Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression. Soc Psychiatry Psychiatr Epidemiol. 2007;42:316–21.
Bernard RS, Williams SE, Storfer‐Isser A, Rhine W, Horwitz SM, Koopman C, et al. Brief cognitive–behavioral intervention for maternal depression and trauma in the neonatal intensive care unit: a pilot study. J Trauma Stress. 2011;24:230–4.
Mendelson T, Cluxton-Keller F, Vullo GC, Tandon SD, Noazin S. NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics. 2017;139:e20161870.
Obregon E, Martin CR, Frantz ID III, Patel P, Smith VC. Neonatal Intensive Care Unit discharge preparedness among families with limited English proficiency. J Perinatol. 2019;39:135–42.
Palau MA, Meier MR, Brinton JT, Hwang SS, Roosevelt GE, Parker TA. The impact of parental primary language on communication in the neonatal intensive care unit. J Perinatol. 2019;39:307–13.
Hynan MT, Hall SL. Psychosocial program standards for NICU parents. J Perinatol. 2015;35:S1.
Acknowledgements
The authors wish to thank Christina DiSanza, MS, Arianna Albanese, MS, and Gaby Russo, MS for their contributions in collecting mental health information from parents and gathering sociodemographics from baby’s medical charts. We also want to extend our sincere gratitude to The Children’s Hospital of Philadelphia Social Work team, including Monica Straszewski, MSW, Ali Pomar, MSW, LSW, Lindsey Kunkel, MSW, LCSW, Ma Luisa Hasiuk, MSW, LCSW, Meredith Huber, MSW, LSW, and Jill Scott, MSW, LCSW, for their support with implementation and follow-up assessments with N/IICU parents.
Author information
Authors and Affiliations
Contributions
VG contributed to QI design, study coordination, data collection and led data analyses, data interpretation, and paper writing. PG contributed to QI design, study oversight, data interpretation, and paper writing. CH contributed to QI design, study oversight, data collection, data interpretation, and paper writing. WN contributed to QI design, study oversight, data interpretation, and paper writing. AA contributed to data collection, data analyses, data interpretation, and paper writing. CP contributed to QI design, study oversight, data collection, data interpretation, and paper writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This QI initiative was reviewed and determined exempt (did not meet the criteria for requiring human subjects research) by the hospital’s Institutional Review Board. Reasons given were as follows: the project is consistent with the institution’s definition of a quality-improvement program, the parents were not patients of the institution, risk was seen as minimal, and all data were de-identified.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grunberg, V.A., Geller, P.A., Hoffman, C. et al. Parental mental health screening in the NICU: a psychosocial team initiative. J Perinatol 42, 401–409 (2022). https://doi.org/10.1038/s41372-021-01217-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01217-0
This article is cited by
-
Collaborative Recognition of Wellbeing Needs: A Novel Approach to Universal Psychosocial Screening on the Neonatal Unit
Journal of Clinical Psychology in Medical Settings (2024)
-
The predictive roles of parental stress and intolerance of uncertainty on psychological well-being of parents with a newborn in neonatal intensive care unit: a hierarchical linear regression analysis
BMC Pediatrics (2023)
-
A biopsychosocial model of NICU family adjustment and child development
Journal of Perinatology (2023)
-
Advancing the Field of Fetal Neurology: A Call for Global Collaborations
Indian Pediatrics (2023)