Abstract
Objective
To examine erythroferrone (ERFE)-hepcidin iron regulation in premature infants under intensive care at risk of iron metabolic disorders.
Study design
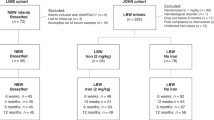
A retrospective cohort recruited 31 infants with a birth weight of <1500 g hospitalized in a tertiary center. Their hematological status was measured at birth and 2 and 4 weeks of life.
Results
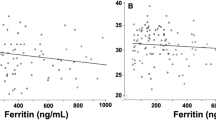
ERFE was positively correlated with the reticulocyte hemoglobin content at 2 (r2 = 0.2374) and 4 weeks (r2 = 0.6005). An assumed negative correlation between ERFE and hepcidin was not determined during the neonatal period. Hepcidin was positively correlated with the leukocyte count (r2 = 0.3089) and ferritin (r2 = 0.7476) at birth and C-reactive protein (r2 = 0.3591) at 2 weeks and negatively correlated with the reticulocyte count (r2 = 0.2887) at 4 weeks.
Conclusion
The vulnerability of the ERFE-hepcidin pathway within 4 weeks may contribute to iron imbalance in premature infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–3.
Ganz T. Hepcidin and iron regulation, 10 years later. Blood. 2011;117:4425–33.
Rishi G, Wallace DF, Subramaniam VN. Hepcidin: regulation of the master iron regulator. Biosci Rep. 2015;35:e00192.
Kautz L, Jung G, Du X, Gabayan V, Chapman J, Nasoff M, et al. Erythroferrone contributes to hepcidin suppression and iron overload in a mouse model of β-thalassemia. Blood. 2015;126:2031–7.
Arezes J, Foy N, McHugh K, Sawant A, Quinkert D, Terraube V, et al. Erythroferrone inhibits the induction of hepcidin by BMP6. Blood. 2018;132:1473–7.
Domellof M. Meeting the iron needs of low and very low birth weight infants. Ann Nutr Metab. 2017;71:16–23.
Park SH, Kim HM. The iron status of very low birth weight infants receiving multiple erythrocyte transfusions during hospitalization in the neonatal intensive care unit. Pediatr Gastroenterol Hepatol Nutr. 2015;18:100–7.
Ochiai M, Kurata H, Inoue H, Tanaka K, Matsushita Y, Fujiyoshi J, et al. An elevation of serum ferritin level might increase clinical risk for the persistence of patent ductus arteriosus, sepsis and bronchopulmonary dysplasia in erythropoietin-treated very-low-birth-weight infants. Neonatology. 2017;111:68–75.
Wang Y, Wu Y, Li T, Wang X, Zhu C. Iron metabolism and brain development in premature infants. Front Physiol. 2019;10:463.
Lonnerdal B. Excess iron intake as a factor in growth, infections, and development of infants and young children. Am J Clin Nutr. 2017;106:1681S–7S.
Watanabe K, Naruse K, Tanaka K, Metoki H, Suzuki Y. Outline of definition and classification of “Pregnancy induced Hypertension (PIH)”. Hypertension Res Pregnancy. 2013;1:3–4.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454.
El Gendy FM, EL-Hawy MA, Shehata AMF, Osheba HE. Erythroferrone and iron status parameters levels in pediatric patients with iron deficiency anemia. Eur J Haematol. 2018;100:356–60.
Ganz T, Jung G, Naeim A, Ginzburg Y, Pakbaz Z, Walter PB, et al. Immunoassay for human serum erythroferrone. Blood. 2017;130:1243–6.
Hanudel MR, Rappaport M, Chua K, Gabayan V, Qiao B, Jung G, et al. Levels of the erythropoietin-responsive hormone erythroferrone in mice and humans with chronic kidney disease. Haematologica. 2018;103:e141–e142.
Hara M, Nakamura Y, Suzuki H, Asao R, Nakamura M, Nishida K, et al. Hepcidin-25/erythroferrone ratio predicts improvement of anaemia in haemodialysis patients treated with ferric citrate hydrate. Nephrology. 2019;24:819–26.
Bahr TM, Ward DM, Jia X, Ohls RK, German KR, Christensen RD. Is the erythropoietin-erythroferrone-hepcidin axis intact in human neonates? Blood Cells Mol Dis. 2021;88:102536.
Karagülle M, Gündüz E, Sahin Mutlu F, Olga Akay M. Clinical significance of reticulocyte hemoglobin content in the diagnosis of iron deficiency anemia. Turk J Haematol. 2013;30:153–6.
Cai J, Wu M, Ren J, Du Y, Long Z, Li G, et al. Evaluation of the efficiency of the reticulocyte hemoglobin content on diagnosis for iron deficiency anemia in chinese adults. Nutrients. 2017;9:450.
Berglund S, Lonnerdal B, Westrup B, Domellof M. Effects of iron supplementation on serum hepcidin and serum erythropoietin in low-birth-weight infants. Am J Clin Nutr. 2011;94:1553–61.
Uijterschout L, Domellöf M, Berglund SK, Abbink M, Vos P, Rövekamp L, et al. Serum hepcidin in infants born after 32 to 37 wk of gestational age. Pediatr Res. 2016;79:608–13.
Kitajima J, Ohga S, Kinjo T, Ochiai M, Takahata Y, Honjo S, et al. Serum prohepcidin concentrations at birth and 1 month after birth in premature infants. Pediatr Blood Cancer. 2011;56:267–72.
Armitage AE, Agbla SC, Betts M, Sise EA, Jallow MW, Sambou E, et al. Rapid growth is a dominant predictor of hepcidin suppression and declining ferritin in Gambian infants. Haematologica. 2019;104:1542–53.
Meznarich JA, Draper L, Christensen RD, Yaish HM, Luem ND, Pysher TJ, et al. Fetal presentation of congenital dyserythropoietic anemia type 1 with novel compound heterozygous CDAN1 mutations. Blood cells Molecules Dis. 2018;71:63–66.
Darshan D, Wilkins SJ, Frazer DM, Anderson GJ. Reduced expression of ferroportin-1 mediates hyporesponsiveness of suckling rats to stimuli that reduce iron absorption. Gastroenterology. 2011;141:300–9.
Acknowledgements
The authors would like to thank our fellows (Dr. Korematsu T, Dr. Watabe T, and Dr. Egami N) for treating the patients and Ms. Unose R and Tanaka T for their technical assistance.
Author information
Authors and Affiliations
Contributions
All authors (NL, MO, TS, KY, JF, HI, and SO) had full access to all the data in the study, took responsibility for the data integrity and accuracy, and approved the final version to be published. MO, TS, and IH designed the study; NL, KY, and JF acquired, analyzed, and interpreted the data; MO, JF, and IH obtained funding; and IH and SO critically revised the relevant intellectual content.
Corresponding author
Ethics declarations
Competing interests
This study was supported in part by the KAKEN #15K09717 (MO), #16K19688 (JF), #17K16300 (HI), and #20K08231 (HI).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lenhartová, N., Ochiai, M., Sawano, T. et al. Serum erythroferrone levels during the first month of life in premature infants. J Perinatol 42, 97–102 (2022). https://doi.org/10.1038/s41372-021-01184-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01184-6
This article is cited by
-
Normal range and predictors of serum erythroferrone in infants
Pediatric Research (2023)