Abstract
Objective
To assess the association between time of birth and mortality among preterm infants.
Study design
Population-based study of infants born 22–36 weeks gestation (GA) in Canada from 2010 to 2015 (n = 173 789). Multivariable logistic regression models assessed associations between timing of birth and mortality.
Result
Among infants 22–27 weeks GA, evening birth was associated with higher mortality than daytime birth (adjusted odds ratio [AOR] 1.14, 95% CI 1.01–1.29). Among infants 28–32 weeks GA and 33–36 weeks GA, night birth was associated with lower mortality than daytime birth (AOR 0.75, 95% CI 0.59–0.95; AOR 0.78, 95% CI 0.62–0.99, respectively). Sensitivity analysis excluding infants with major congenital anomaly revealed that associations between hour of birth and mortality among infants born 28–32 and 33–36 weeks GA decreased or were not statistically significant.
Conclusion
Higher mortality among extremely preterm infants during off-peak hours may suggest variations in available resources based on time of day.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Beltempo M, Shah PS, Ye XY, Afifi J, Lee S, McMillan DD; Canadian Neonatal Network Investigators. SNAP-II for prediction of mortality and morbidity in extremely preterm infants. J Matern Fetal Neonatal Med. 2019;32:2694–2701. https://doi.org/10.1080/14767058.2018.1446079.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Rizzolo A, Shah PS, Boucorian I, Lemyre B, Bertelle V, Pelausa E, et al. Cumulative effect of evidence-based practices on outcomes of preterm infants born at <29 weeks gestational age. Am J Obstetrics Gynecol. 2020;222:181.e1–181.e10. https://doi.org/10.1016/j.ajog.2019.08.058.
Lyu Y, Shah PS, Ye XY, Warre R, Piedboeuf B, Deshpandey A, et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatrics. 2015;169:e150277.
Beltempo M, Lacroix G, Cabot M, Blais R, Piedboeuf B. Association of nursing overtime, nurse staffing and unit occupancy with medical incidents and outcomes of very preterm infants. J Perinatol. 2018;38:175–80.
Shahroor M, Lehtonen L, Lee SK, Hakansson S, Vento M, Darlow BA, et al. Unit-level variations in healthcare professionals’ availability for preterm neonates <29 weeks’ gestation: an international survey. Neonatology. 2019;116:347–55. https://doi.org/10.1159/000501801.
Bell EF, Hansen NI, Morriss FH Jr, Stoll BJ, Ambalavanan N, Gould JB, et al. Impact of timing of birth and resident duty-hour restrictions on outcomes for small preterm infants. Pediatrics. 2010;126:222–31.
Caughey AB, Urato AC, Lee KA, Thiet MP, Washington AE, Laros RK Jr. Time of delivery and neonatal morbidity and mortality. Am J Obstet Gynecol. 2008;199:496.e491–495.
Gijsen R, Hukkelhoven CW, Schipper CM, Ogbu UC, de Bruin-Kooistra M, Westert GP. Effects of hospital delivery during off-hours on perinatal outcome in several subgroups: a retrospective cohort study. BMC Pregnancy Childbirth. 2012;12:92.
Heller G, Misselwitz B, Schmidt S. Early neonatal mortality, asphyxia related deaths, and timing of low risk births in Hesse, Germany, 1990-8: observational study. BMJ (Clin Res ed). 2000;321:274–5.
Jensen EA, Lorch SA. Association between off-peak hour birth and neonatal morbidity and mortality among very low birth weight infants. J Pediatrics. 2017;186:41–48.e44.
Lee SK, Lee DS, Andrews WL, Baboolal R, Pendray M, Stewart S. Higher mortality rates among inborn infants admitted to neonatal intensive care units at night. J Pediatrics. 2003;143:592–7.
Paccaud F, Martin-Beran B, Gutzwiller F. Hour of birth as a prognostic factor for perinatal death. Lancet (Lond, Engl). 1988;1:340–3.
Beltempo M, Piedboeuf B, Platt RW, Barrington K, Bizgu V, Shah PS. Association of resident duty hour reform and neonatal outcomes of very preterm infants. Am J Perinatol. 2017;34:1396–404.
Knight HE, van der Meulen JH, Gurol-Urganci I, Smith GC, Kiran A, Thornton S, et al. Birth “out-of-hours”: an evaluation of obstetric practice and outcome according to the presence of senior obstetricians on the labour ward. PLoS Med. 2016;13:e1002000.
Canadian Neonatal Network Annual Report Committee. Canadian Neonatal Network 2017 Annual report. Toronto, Ontario; 2018.
Joseph KS, Fahey J. Validation of perinatal data in the Discharge Abstract Database of the Canadian Institute for Health Information. Chronic Dis Can. 2009;29:96–100.
Canadian Institute for Health Information. Data Quality Study of the 2015–2016 Discharge Abstract Database: A Focus on Hospital Harm. Ottawa, ON: CIHI; 2016.
Beltempo M, Clement K, Lacroix G, Bélanger S, Julien AS, Piedboeuf B. Association of resident duty hour restrictions, level of trainee, and number of available residents with mortality in the neonatal intensive care unit. Am J Perinatol. 2018;35:911–8.
Janssen PA, Saxell L, Page LA, Klein MC, Liston RM, Lee SK. Outcomes of planned home birth with registered midwife versus planned hospital birth with midwife or physician. Can Med Assoc J. 2009;181:377.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35.
Bassil KL, Collier S, Mirea L, Yang J, Seshia MM, Shah PS, et al. Association between congenital anomalies and area-level deprivation among infants in neonatal intensive care units. Am J Perinatol. 2013;30:225–32.
Allanson E, Tunçalp Ö, Gardosi J, Pattinson RC, Erwich JJ, Flenady VJ, et al. Classifying the causes of perinatal death. Bull World Health Organ. 2016;94:79–79a.
Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N. Engl J Med. 2015;372:1801–11.
Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–46.
Statistics Canada. Table 13-10-0415-01 Live births, by month. 2020.
Auger N, Park AL, Zoungrana H, McHugh NG, Luo ZC. Rates of stillbirth by gestational age and cause in Inuit and First Nations populations in Quebec. CMAJ. 2013;185:E256–262.
Cnattingius S, Johansson S, Razaz N. Apgar score and risk of neonatal death among preterm infants. N. Engl J Med. 2020;383:49–57.
Ruffieux C, Marazzi A, Paccaud F. The circadian rhythm of the perinatal mortality rate in Switzerland. Am J Epidemiol. 1992;135:936–52.
Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, et al. Risks of complications by attending physicians after performing nighttime procedures. Jama. 2009;302:1565–72.
Rollinson DC, Rathlev NK, Moss M, Killiany R, Sassower KC, Auerbach S, et al. The effects of consecutive night shifts on neuropsychological performance of interns in the emergency department: a pilot study. Ann Emerg Med. 2003;41:400–6.
Campbell AM, Nilsson K, Pilhammar Andersson E. Night duty as an opportunity for learning. J Adv Nurs. 2008;62:346–53.
Aalen OO, Valberg M, Grotmol T, Tretli S. Understanding variation in disease risk: the elusive concept of frailty. Int J Epidemiol. 2015;44:1408–21.
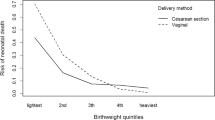
Grabovac M, Karim JN, Isayama T, Liyanage SK, McDonald SD. What is the safest mode of birth for extremely preterm breech singleton infants who are actively resuscitated? A systematic review and meta-analyses. Bjog. 2018;125:652–63.
Jarde A, Feng YY, Viaje KA, Shah PS, McDonald SD. Vaginal birth vs caesarean section for extremely preterm vertex infants: a systematic review and meta-analyses. Arch Gynecol Obstet. 2020;301:447–58.
Delnord M, Blondel B, Drewniak N, Klungsøyr K, Bolumar F, Mohangoo A, et al. Varying gestational age patterns in cesarean delivery: an international comparison. BMC pregnancy childbirth. 2014;14:321.
Wang D, Yasseen AS 3rd, Marchand-Martin L, Sprague AE, Graves E, Goffinet F, et al. A population-based comparison of preterm neonatal deaths (22-34 gestational weeks) in France and Ontario: a cohort study. CMAJ Open. 2019;7:E159–e166.
Shah PS, Lui K, Sjors G, Mirea L, Reichman B, Adams M, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatrics. 2016;177:144. e146
Lee SK, Beltempo M, McMillan DD, Seshia M, Singhal N, Dow K, et al. Outcomes and care practices for preterm infants born at less than 33 weeks’ gestation: a quality-improvement study. CMAJ. 2020;192:E81–e91.
Allin S. Does equity in healthcare use vary across Canadian provinces? Health Policy. 2008;3:83–99.
Tran DT, Welsh RC, Ohinmaa A, Thanh NX, Bagai A, Kaul P. Quality of acute myocardial infarction care in Canada: a 10-year review of 30-day in-hospital mortality and 30-day hospital readmission. Can J Cardiol. 2017;33:1319–26.
Acknowledgements
The authors thank all site investigators and data abstractors of the Canadian Neonatal Network (CNN) and the Canadian Preterm Birth Network (CPTBN). A list of Network member investigators and their affiliations is provided below. We thank Heather McDonald Kinkaid, PhD, for editorial support in preparing this manuscript. Dr. Kinkaid is a scientific writer employed with the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada; and receives a salary for her work. We thank other MiCare staff for organizational support.
Canadian Neonatal Network (CNN) and the Canadian Preterm Birth Network
Haim Abenhaim8, Jehier Afifi9, Ruben Alvaro10, James Andrews11, Anthony Armson9, Francois Audibert12, Khalid Aziz13, Marilyn Ballantyne14, Jon Barrett15, Marc Beltempo16, Anick Berard17, Valerie Bertelle18¸ Lucie Blais17, Alan Bocking19, Jaya Bodani20, Jason Burrows21, Kimberly Butt4, Roderick Canning22, George Carson20, Nils Chaillet23, Sue Chandra13, Paige Church24, Zenon Cieslak25, Kevin Coughlin26, Joan Crane27, Dianne Creighton28, Orlando Da Silva29¸ Thierry Daboval30, Leanne Dahlgren31, Sibasis Daspal32, Cecilia de Cabo33, Akhil Deshpandey27, Kimberly Dow34, Christine Drolet35, Michael Dunn24, Salhab el Helou36, Darine El-Chaar30, Walid El-Naggar9, Carlos Fajardo28, Jonathan Foster37, Robert Gagnon16, Rob Gratton29, Victor Han38, Adele Harrison39, Shabih Hasan40, Michael Helewa10, Matthew Hicks41, KS Joseph42, Andrzej Kajetanowicz43, Zarin Kalapesi20, May Khairy44, Thierry Lacaze-Masmonteil45, Kyong-Soon Lee46, Brigitte Lemyre47, Abhay Lodha48, Deepak Louis49, Thuy Mai Luu50, Linh Ly46, Annette Majnemer44, Hala Makary51, Isabelle Marc23, Edith Masse18, Sarah D McDonald52, Doug McMillan10, Nir Melamed24, Amy Metcalfe53, Diane Moddemann33, Luis Monterrosa11, Michelle Morais36, Amit Mukerji36, William Mundle54, Lynn Murphy22, Kellie Murphy19, Anne-Monique Nuyt12, Chuks Nwaesei54, Karel O’Brien19, Martin Offringa46, Cecil Ojah11, Annie Ouellet18, Jean-Charles Pasquier55, Petros Pechlivanoglou46, Ermelinda Pelausa8, Bruno Piedboeuf23, Elodie Portales-Casamar56, Shahirose Premji40, Pramod Puligandla44, Eleanor Pullenayegum46, Amber Reichert57, Kate Robson37, Carol Schneider58, Mary Seshia58, Prakesh S Shah19, Vibhuti Shah19, Rebecca Sherlock21, Sandesh Shivananda42, Nalini Singhal28, Erik Skarsgard59, Amanda Skoll60, Graeme Smith34, Anne Synnes42, Katherine Thériault35, Joseph Ting60, Suzanne Tough40, Jennifer Toye13, Jagdeep Ubhi25, Michael Vincer9, Wendy Whittle19, Hilary Whyte46, Doug Wilson48, Stephen Wood48, Philip Ye19, Wendy Yee48, Jill Zwicker42
Funding
This study was supported by a grant from the Canadian Institutes of Health Research (CIHR) funding the Canadian Preterm Birth Network (PBN 150642). Organizational support for the Canadian Neonatal Network and the Canadian Preterm Birth Network was provided by the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by a CIHR Team Grant (CTP 87518), the Ontario Ministry of Health and Long-Term Care, and the participating hospitals. Prakesh Shah holds a CIHR Applied Research Chair in Reproductive and Child Health Services and Policy Research (APR-126340). Marc Beltempo holds an Early Career Investigator Grant from the CIHR Institute of Human Development, Child and Youth Health (IHDCYH). The funding agencies had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
AR and MB were responsible for designing and writing the protocol, interpreting results, and redacting this manuscript. XYY was responsible for statistical analysis and generating the tables. PSS, VB, HM, XYY, HAA, and BP were responsible for reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Canadian Neonatal Network (CNN) and Canadian Preterm Birth Network (CPTBN) are listed below Acknowledgements.
Supplementary information
Rights and permissions
About this article
Cite this article
Rizzolo, A., Shah, P.S., Bertelle, V. et al. Association of timing of birth with mortality among preterm infants born in Canada. J Perinatol 41, 2597–2606 (2021). https://doi.org/10.1038/s41372-021-01092-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01092-9
This article is cited by
-
Neonatal intensive care unit occupancy rate and probability of discharge of very preterm infants
Journal of Perinatology (2023)
-
Time at birth and short-term outcomes among extremely preterm infants in Spain: a multicenter cohort study
European Journal of Pediatrics (2022)
-
Outcomes of infants with hypoxic-ischemic encephalopathy during COVID-19 pandemic lockdown in Canada: a cohort study
Child's Nervous System (2022)