Abstract
Objective:
To serially assess fetal cardiac dimensions in congenital diaphragmatic hernia (CDH) and their relation to disease severity.
Study design:
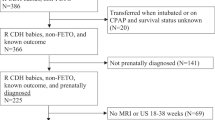
Retrospective analysis of CDH cases and matched controls. Mitral (MVd) and tricuspid (TVd) valve diameters, left (LV) and right (RV) ventricular length and area, Z-scores, were serially assessed at 24–26, 30–32, and 35–37 weeks gestational age (GA).
Results:
In CDH cases MVd, MVd Z-score, and LV area were significantly reduced at 24–26 and 35–37 weeks GA. TVd, TVd Z-score, and RV area were significantly reduced at 24–26 weeks. RV area Z-score increased with advancing GA. MVd and MVd Z-score were significantly lower at 24–26 weeks GA in CDH who had a combined outcome of death and/or ECMO.
Conclusions:
LV hypoplasia in CDH is characterized by reduced MVd from 24 weeks GA. MVd, and the ratio of mitral and tricuspid valve diameters at later gestations, may be potential predictors of disease severity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Harting MT, Lally KP. The Congenital Diaphragmatic Hernia Study Group registry update. Semin Fetal Neonatal Med. 2014;19:370–5.
Harting MT. Congenital diaphragmatic hernia-associated pulmonary hypertension. Semin Pediatr Surg. 2017;26:147–53.
Kinsella JP, Ivy DD, Abman SH. Pulmonary vasodilator therapy in congenital diaphragmatic hernia: acute, late, and chronic pulmonary hypertension. Semin Perinatol. 2005;29:123–8.
Kipfmueller F, Heindel K, Schroeder L, Berg C, Dewald O, Reutter H, et al. Early postnatal echocardiographic assessment of pulmonary blood flow in newborns with congenital diaphragmatic hernia. J Perinat Med. 2018;46:735–43.
Patel N, Massolo AC, Paria A, Stenhouse EJ, Hunter L, Finlay E, et al. Early postnatal ventricular dysfunction is associated with disease severity in patients with congenital diaphragmatic hernia. J Pediatr. 2018;203:400–7.
Patel N, Lally PA, Kipfmueller F, Massolo AC, Luco M, Van Meurs KP, et al. Ventricular dysfunction is a critical determinant of mortality in congenital diaphragmatic hernia. Am J Respir Crit Care Med. 2019;200:1522–30.
Siebert JR, Haas JE, Beckwith JB. Left ventricular hypoplasia in congenital diaphragmatic hernia. J Pediatr Surg. 1984;19:567–71.
Kinsella J, Steinhorn R, Mullen M, Hopper R, Keller R, Ivy D, et al. The left ventricle in congenital diaphragmatic hernia: implications for the management of pulmonary hypertension. J Pediatr. 2018;197:17–22.
Putnam LR, Harting MT, Tsao K, Morini F, Yoder BA, Luco M, et al. Congenital diaphragmatic hernia defect size and infant morbidity at discharge. Pediatrics. 2016;138:e20162043.
Alves L, Byrne A, Keller RL, Brook MM, Silverman H, Moon-grady AJ. Left heart structures in human neonates with congenital diaphragmatic hernia and the effect of fetal endoscopic tracheal occlusion. Fetal Diagn Ther. 2014;35:36–43.
Lee W, Riggs T, Amula V, Tsimis M, Cutler N, Bronsteen R, et al. Fetal echocardiography: Z-score reference ranges for a large patient population. Ultrasound Obstet Gynecol. 2010;35:28–34.
Mardy C, Blumenfeld YJ, Arunamata AA, Girsen AI, Sylvester KG, Halabi S, et al. In fetuses with congenital lung masses, decreased ventricular and atrioventricular valve dimensions are associated with lesion size and clinical outcome. Prenat Diagn. 2020;40:206–15.
Vogel M, McElhinney DB, Marcus E, Morash D, Jennings RW, Tworetzky W. Significance and outcome of left heart hypoplasia in fetal congenital diaphragmatic hernia. Ultrasound Obstet Gynecol. 2010;35:310–7.
Schneider C, McCrindle BW, Carvalho JS, Hornberger LK, McCarthy KP, Daubeney PEF. Development of Z-scores for fetal cardiac dimensions from echocardiography. Ultrasound Obstet Gynecol. 2005;26:599–605.
Jani J, Nicolaides KH, Keller RL, Benachi A, Peralta CFA, Favre R, et al. Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007;30:67–71.
Romiti A, Viggiano M, Conforti A, Valfré L, Ravà L, Ciofi Degli Atti M, et al. Ultrasonographic assessment of mediastinal shift angle (MSA) in isolated left congenital diaphragmatic hernia for the prediction of postnatal survival. J Matern Neonatal Med. 2018;0:1–6.
Byrne FA, Keller RL, Meadows J, Miniati D, Brook MM, Silverman NH, et al. Severe left diaphragmatic hernia limits size of fetal left heart more than does right diaphragmatic hernia. Ultrasound Obstet Gynecol. 2015;46:688–94.
Kailin JA, Dhillon GS, Maskatia SA, Cass DL, Shamshirsaz AA, Mehollin-ray AR, et al. Fetal left-sided cardiac structural dimensions in left-sided congenital diaphragmatic hernia–association with severity and impact on postnatal outcomes. Prenat Diagn. 2017;37:502–9.
Stressig R, Fimmers R, Eising K, Gembruch U, Kohl T. Preferential streaming of the ductus venosus and inferior caval vein towards the right heart is associated with left heart underdevelopment in human fetuses with left-sided diaphragmatic hernia. Heart. 2010;96:1564–8.
Duy D, Patel N, Harting MT, Lally KP, Lally PA, Buchmiller TL. Early left ventricular dysfunction and severe pulmonary hypertension predict adverse outcomes in ‘low-risk’ congenital diaphragmatic hernia. Pediatr Crit Care Med. 2020;21:637–46.
Crawford DC, Wright VM, Drake DP, Allan LD. Fetal diaphragmatic hernia: the value of fetal echocardiography in the prediction of postnatal outcome. BJOG Int J Obstet Gynaecol. 1989;96:705–10.
Yamoto M, Tanaka Y, Fukumoto K, Miyake H, Nakajima H, Koyama M, et al. Cardiac fetal ultrasonographic parameters for predicting outcomes of isolated left-sided congenital diaphragmatic hernia. J Pediatr Surg. 2015;50:2019–24.
Mandell EW, Kinsella JP. Left ventricular dysfunction and persistent perfusion abnormalities in infants with congenital diaphragmatic hernia. J Pediatr. 2019;219:7–8.
Massolo AC, Paria A, Hunter L, Finlay E, Davis CF, Patel N. Ventricular dysfunction, interdependence, and mechanical dispersion in newborn infants with congenital diaphragmatic hernia. Neonatology. 2019;116:68–75.
Oluyomi-obi T, Kuret V, Puligandla P, Lodha A, Lee-robertson H, Lee K, et al. Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg. 2017;52:881–8.
Tan J, Silverman NH, Hoffman JIE, Villegas M, Schmidt KG. Cardiac dimensions determined by cross-sectional echocardiography in the normal human fetus from 18 weeks to term. Am J Cardiol. 1992;70:1459–67.
Acknowledgements
We are grateful to the Dr. Irma Capolupo for her assistance with the study, to Dr. Luciano Pasquini and Dr. Alessandra Toscano for their expert advice in preparation of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors met ICMJE authorship criteria.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics statement
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Massolo, A.C., Romiti, A., Viggiano, M. et al. Fetal cardiac dimensions in congenital diaphragmatic hernia: relationship with gestational age and postnatal outcomes. J Perinatol 41, 1651–1659 (2021). https://doi.org/10.1038/s41372-021-00986-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00986-y
This article is cited by
-
Early nitric oxide is not associated with improved outcomes in congenital diaphragmatic hernia
Pediatric Research (2023)
-
Right to left ventricular volume ratio is associated with mortality in congenital diaphragmatic hernia
Pediatric Research (2023)
-
Epidemiology of congenital diaphragmatic hernia among 24 million Chinese births: a hospital-based surveillance study
World Journal of Pediatrics (2023)
-
Congenital diaphragmatic hernia
Nature Reviews Disease Primers (2022)