Abstract
Objective
To compare medications dispensed during the first 2 years in children born preterm and full-term.
Study design
Retrospective analysis of claims data from a commercial national managed care plan 2008–2019. 329,855 beneficiaries were enrolled from birth through 2 years, of which 25,408 (7.7%) were preterm (<37 weeks). Filled prescription claims and paid amount over 2 years were identified.
Results
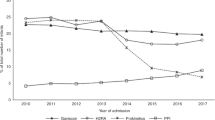
In preterm children, the number of filled prescriptions was 1.4 times and cost was 3.8 times that of full-term children. Number and cost of medications were inversely related to gestational age. Differences peak at 4–9 months and resolve by 19 months after discharge. Palivizumab, ranitidine, albuterol, lansoprazole, budesonide, and prednisolone had the greatest differences in utilization.
Conclusion
Prescription medication utilization among preterm children under 2 years is driven by palivizumab, anti-reflux, and respiratory medications, despite little evidence regarding efficacy for many medications and concern for harm with certain classes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Authors' data use agreement for the claims dataset does not permit public posting of this patient information.
Code availability
Code used to generate the results is available by request to the corresponding author; however, per terms of the health plan supplying the data, and because of the risk of reidentification, the underlying patient data are not able to be shared.
References
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: Final data for 2017. National Vital Statistics Reports; vol 67 no 8. Hyattsville, MD: National Center for Health Statistics; 2018.
Smith VC, Zupancic JAF, McCormick MC, Croen LA, Greene J, Escobar GJ, et al. Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr. 2004;144:799–803.
Wade KC, Lorch SA, Bakewell-Sachs S, Medoff-Cooper B, Silber JH, Escobar GJ. Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol. 2008;28:696–701.
Beam AL, Fried I, Palmer N, Agniel D, Brat G, Fox K, et al. Estimates of healthcare spending for preterm and low-birthweight infants in a commercially insured population: 2008–2016. J Perinatol. 2020. https://doi.org/10.1038/s41372-020-0635-z.
Bamat NA, Kirpalani H, Feudtner C, Jensen EA, Laughon MM, Zhang H, et al. Medication use in infants with severe bronchopulmonary dysplasia admitted to United States children’s hospitals. J Perinatol. 2019;39:1291–9.
D’Agostino JA, Passarella M, Martin AE, Lorch SA. Use of gastroesophageal reflux medications in premature infants after NICU discharge. Pediatrics. 2016;138. https://doi.org/10.1542/peds.2016-1977.
Orenstein SR, Hassall E, Furmaga-Jablonska W, Atkinson S, Raanan M. Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety of proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. J Pediatr. 2009;154:514–520.e4.
Ho T, Dukhovny D, Zupancic JAF, Goldmann DA, Horbar JD, Pursley DM. Choosing wisely in newborn medicine: five opportunities to increase value. Pediatrics. 2015;136:e482–9.
Canani RB, Cirillo P, Roggero P, Romano C, Malamisura B, Terrin G, et al. Therapy with gastric acidity inhibitors increases the risk of acute gastroenteritis and community-acquired pneumonia in children. Pediatrics. 2006;117:e817–20.
Mitre E, Susi A, Kropp LE, Schwartz DJ, Gorman GH, Nylund CM. Association between use of acid-suppressive medications and antibiotics during infancy and allergic diseases in early childhood. JAMA Pediatr. 2018;172:e180315.
Wagner KL, Wagner SC, Susi A, Gorman G, Hisle-Gorman E. Prematurity and early childhood fracture risk. Pediatrics. 2018;141:757.
FDA. FDA requests removal of all ranitidine products (Zantac) from the Market. FDA; 2020. https://www.fda.gov/news-events/press-announcements/fda-requests-removal-all-ranitidine-products-zantac-market. Accessed 22 Jun 2020.
Amneal Pharmaceuticals, LLC. Issues voluntary nationwide recall of nizatidine oral solution, 15 mg/mL, due to potential levels of n-nitrosodimethylamine (NDMA) impurity amounts above the levels established by FDA. US Food Drug Adm; 2020. https://www.fda.gov/safety/recalls-market-withdrawals-safety-alerts/amneal-pharmaceuticals-llc-issues-voluntary-nationwide-recall-nizatidine-oral-solution-15-mgml-due. Accessed 22 Jun 2020.
Landry JS, Croitoru D, Jin Y, Schwartzman K, Benedetti A, Menzies D. Health care utilization by preterm infants with respiratory complications in Quebec. Can Respir J. 2012;19:255–60.
Damgaard AL, Hansen BM, Mathiasen R, Buchvald F, Lange T, Greisen G. Prematurity and prescription asthma medication from childhood to young adulthood: a Danish national cohort study. PLoS ONE. 2015;10:e0117253.
Damgaard AL, de B, Gregersen R, Lange T, Buchvald F, Hansen BM, et al. The increased purchase of asthma medication for individuals born preterm seems to wane with age: a register-based longitudinal national cohort study. PLoS ONE. 2018;13:e0199884.
Ryan RM, Keller RL, Poindexter BB, D’Angio CT, Shaw PA, Bellamy SL, et al. Respiratory medications in infants <29 weeks during the first year postdischarge: the Prematurity and Respiratory Outcomes Program (PROP) Consortium. J Pediatr. 2019;208:148–155.e3.
Duijts L, Meel ER van, Moschino L, Baraldi E, Barnhoorn M, Bramer WM, et al. European Respiratory Society guideline on long term management of children with bronchopulmonary dysplasia. Eur Respir J. 2019. https://doi.org/10.1183/13993003.00788-2019.
Lakhani CM, Tierney BT, Manrai AK, Yang J, Visscher PM, Patel CJ. Repurposing large health insurance claims data to estimate genetic and environmental contributions in 560 phenotypes. Nat Genet. 2019;51:327–34.
Fried I, Beam AL, Kohane IS, Palmer NP. Utilization, cost, and outcome of branded vs compounded 17-alpha hydroxyprogesterone caproate in prevention of preterm birth. JAMA Intern Med. 2017;177:1689–90.
Geva A, Gronsbell JL, Cai T, Cai T, Murphy SN, Lyons JC, et al. A computable phenotype improves cohort ascertainment in a pediatric pulmonary hypertension registry. J Pediatr. 2017;188:224–231.e5.
Natarajan G, Shankaran S. Short- and long-term outcomes of moderate and late preterm infants. Am J Perinatol. 2016;33:305–17.
Fawke J, Lum S, Kirkby J, Hennessy E, Marlow N, Rowell V, et al. Lung function and respiratory symptoms at 11 years in children born extremely preterm: the EPICure study. Am J Respir Crit Care Med. 2010;182:237–45.
Thunqvist P, Tufvesson E, Bjermer L, Winberg A, Fellman V, Domellöf M, et al. Lung function after extremely preterm birth—a population-based cohort study (EXPRESS). Pediatr Pulmonol. 2018;53:64–72.
Ambalavanan N, Carlo WA, McDonald SA, Yao Q, Das A, Higgins RD, et al. Identification of extremely premature infants at high risk of rehospitalization. Pediatrics. 2011;128:e1216–1225.
Keller RL, Feng R, DeMauro SB, Ferkol T, Hardie W, Rogers EE, et al. Bronchopulmonary dysplasia and perinatal characteristics predict 1-year respiratory outcomes in newborns born at extremely low gestational age: a prospective cohort study. J Pediatr. 2017;187:89–97.e3.
Mourani PM, Kinsella JP, Clermont G, Kong L, Perkins AM, Weissfeld L, et al. Intensive care unit readmission during childhood after preterm birth with respiratory failure. J Pediatr. 2014;164:749–755.e3.
Hsieh EM, Hornik CP, Clark RH, Laughon MM, Benjamin DK, Smith PB. Medication use in the neonatal intensive care unit. Am J Perinatol. 2014;31:811–22.
Schmiedl S, Fischer R, Ibáñez L, Fortuny J, Klungel OH, Reynolds R, et al. Utilisation and off-label prescriptions of respiratory drugs in children. PLoS ONE. 2014;9. https://doi.org/10.1371/journal.pone.0105110.
Eichenwald EC, Committee on Fetus and Newborn. Diagnosis and management of gastroesophageal reflux in preterm infants. Pediatrics. 2018;142. https://doi.org/10.1542/peds.2018-1061.
Collaco JM, Kole AJ, Riekert KA, Eakin MN, Okelo SO, McGrath-Morrow SA. Respiratory medication adherence in chronic lung disease of prematurity. Pediatr Pulmonol. 2012;47:283–91.
Funding
This research was supported by the following funding sources: NHLBI U01HL121518 (KDM) and T15LM007092 (PI: Nils Gehlenborg).
Author information
Authors and Affiliations
Contributions
JCL designed and conducted the analysis and drafted the initial manuscript. ALB designed initial code to identify the cohort, assisted with statistical analysis, and reviewed the manuscript. KPF assisted with design of the analysis and reviewed the manuscript. KDM provided supervision for the design and analysis and provided multiple manuscript revisions.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Levin, J.C., Beam, A.L., Fox, K.P. et al. Medication utilization in children born preterm in the first two years of life. J Perinatol 41, 1732–1738 (2021). https://doi.org/10.1038/s41372-021-00930-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00930-0
This article is cited by
-
Early childhood antibiotic utilization for infants discharged from the neonatal intensive care unit
Journal of Perinatology (2022)