Abstract
Objective
Determine odds ratios for neonatal abstinence syndrome (NAS) and neonatal intensive care unit (NICU) admissions for babies born to women associated with severe mental illness (SMI) and gestational opioid use.
Study design
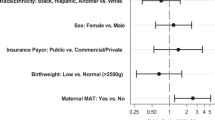
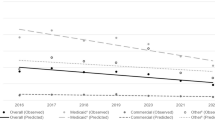
A retrospective pharmacoepidemiologic study using Medicaid data included 17,130 mothers with and 170,430 mothers without SMI, and their babies. Odds ratios for NAS and NICU admissions among babies born to mothers associated with SMI diagnoses and associated with varying degrees of gestational opioid use were determined using logistic regression.
Results
The adjusted odds ratio for a baby in the methadone or buprenorphine group having NAS was 168.93 [95% confidence interval (CI) 148.78–191.71, P < 0.001] and was 9.64 (95% CI 8.74–10.65, P < 0.001) for NICU admissions compared to babies with no opioid exposure.
Conclusions
Chronicity of prescription maternal opioid use was the strongest factor associated with NAS and NICU admissions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Code availability
The codes generated during the study are available from the corresponding author on request.
References
Centers for Disease Control and Prevention. Data overview—overview of the drug overdose epidemic: behind the numbers. 2018. https://www.cdc.gov/drugoverdose/data/index.html. Accessed 20 Nov 2019.
Hedegaard H, Minino AM, and Warner M Drug overdose deaths in the United States, 1999–2017. National Center for Health Statstics Data Brief No. 329. 2018. https://www.cdc.gov/nchs/products/databriefs/db329.htm. Accessed 20 Nov 2019.
Caitline ME, Longinaker N, Terplan M. Recent trends in treatment admissions for prescription opioid abuse during pregnancy. J Subst Abus Treat. 2015;48:32–42.
Ross EJ, Graham DL, Money KM, Stanwood GD. Developmental consequences of fetal exposure to drugs: what we know and what we still must learn. Neuropsychopharmacology. 2015;40:61–87.
Broussard CS, Rasmussen SA, Reefhuis J, Friedman JM, Jann MW, Riehle-Colarusso T, et al. Maternal treatment with opioid analgesics and risk for birth defects. Am J Obstet Gynecol. 2011;204:314.e1–11.
Disher T, Gullickson C, Singh B, Cameron C, Boulos L, Beaubien L, et al. Pharmacological treatments for neonatal abstinence syndrome: a systematic review and network meta-analysis. JAMA Pediatr. 2019;173:234–43. https://doi.org/10.1001/jamapediatrics.2018.5044
Reddy UM, Davis JM, Ren Z, Greene MF. Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, American Congress of Obstetricians and Gynecologists, American Academy of Pediatrics, Society for Maternal-Fetal Medicine, Centers for Disease Control and Prevention, and March of Dimes Foundation. Obstet Gynecol 2017;130:1028. https://doi.org/10.1097/AOG.0000000000002054
Jones HE, Kaltenbach K, Heil SH, Stine SM, Coyle MG, Arria AM, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N Eng J Med. 2010;363:2320–31. https://doi.org/10.1056/NEJMoa1005359
Jones HE, Johnson RE, Jasinski DR, O’Grady KE, Chisholm CA, Choo RE, et al. Buprenorphine versus methadone in treatment of pregnant opioid-dependent patients: effects on the neonatal abstinence syndrome. Drug Alcohol Depend. 2005;79:1–10.
Azuine RE, Ji Y, Chang HY, Kim Y, Ji H, DiBari J, et al. Prenatal risk factors and perinatal and postnatal outcomes associated with maternal opioid exposure in an urban, low-income, multiethnic US population. JAMA Netw Open. 2019;2:e196405. https://doi.org/10.1001/jamanetworkopen.2019.6405
Witt CE, Rudd KE, Rivara FP, Hawes SE, Weiss NE. Neonatal abstinence syndrome and childhood morbidity and mortality in Washington state: a retrospective cohort study. J Perinatol. 2017;37:1124–9.
Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, et al. Neonatal outcomes in women with untreated antenatal depression compared to women without depression: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73:826–37. https://doi.org/10.1001/jamapsychiatry.2016.0934
Wisner KL, Sit DK, Hanusa BH, Moses-Kolko EL, Bogen DL, Hunker DF, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009;165:557–66. https://doi.org/10.1176/appi.ajp.2008.08081170.
Mei-Dan E, Ray JG, Vigod SN. Perinatal outcomes among women with bipolar disorder: a population-based cohort study. Am J Obstet Gynecol. 2015;212:367.e1–8.
Nilson E, Lichtenstein P, Cnattingius S, et al. Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophrenia Res. 2002;58:221–9.
Lee HC, Lin HC. Maternal bipolar disorder increased low birthweight and preterm births: a nationwide population-based study. J Affect Disord. 2010;121:100–5.
Bennedsen BE, Mortensen PB, Olesen AV, Henriksen TB. Congenital malformations, stillbirths, and infant deaths among children of women with schizophrenia. Arch Gen Psychiatry. 2001;58:674–9.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, MaCallum M, et al. Perinatal mental health 3: effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384:1800–19.
Centers for Medicare and Medicaid Services. 2018 General Equivalence Mappings (GEMS). 2017. https://www.cms.gov/Medicare/Coding/ICD10/2018-ICD-10-CM-and-GEMs.html. Accessed 12 Aug 2019.
Florida Department of Health, Office of Rural Health. Rural county list based on a density of less than 100 persons per square mile. 2019. http://www.floridahealth.gov/programs-and-services/community-health/rural-health/_documents/rual-counties-2000-2010.pdf. Accessed 22 Jul 2019.
Centers for Disease Control and Prevention. Opioid use disorder documented at delivery hospitalization—United States, 1999–2014. Morbidity Mortal Wkly Rep. 2018;67:845–9.
Florence C, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54:901–6.
Winkelman T, Chang VW, Biswanger IA. Health, polysubstance use, and criminal justice involvement in adults with varying levels of opioid use. JAMA Netw Open. 2018;1:80558. https://doi.org/10.1001/jamanetworkopen.2018.0558
Centers for Disease Control and Prevention. Understanding the epidemic. 2018. https://www.cdc.gov/drugoverdose/epidemic/index.html. Accessed 22 July 2019.
Whiteman VE, Salemi JL, Mogos MF, Cain MA, Aliyu MH, and Salihu HM. Maternal opioid drug use during pregnancy and its impact on perinatal morbidity, mortality, and the costs of medical care in the United States. J Pregnancy. 2014:906723. https://doi.org/10.1155/2014/906723.
Lorenz K, Gannon M, Ramage M, Coulson CC, Wilson C, and Galvin SL. Psychotropic medications do not appear to increase NAS risk in women on MAT. Am J Obstet Gynecol. 2019;220,suppl:S224–5.
The American College of Obstetricians and Gynecologists. Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130:e81–94. Committee Opinion No 711.
Patrick SW, Schumacher RE, Horbar JD, Buus-Frank ME, Edwards EM, Morrow KA, et al. Improving care for neonatal abstinence syndrome. Pediatrics. 2016;137:e20153835.
Hartgrove MJ, Meschke LL, King TL, Saunders C. Treating infants with neonatal abstinence syndrome: an examination of three protocols. J Perinatol. 2019;29:1377–83.
Jones HE, Fischer G, Heil SH, Kaltenbach K, Martin PR, Coyle MG, et al. Maternal Opioid Treatment: Human Experimental Research (MOTHER)—approach, issues, and lessons learned. Addiction. 2012;107(Supp. 1):28–35. https://doi.org/10.1111/j.1360-0443.2012.04036.x
Wachman EM, Hayes MJ, Brown MS, Paul J, Harvey-Wilkes K, Terrin N, et al. Association of OPRM1 and COMT single-nucleotide polymorphisms with hospital length of stay and treatment of neonatal abstinence syndrome. JAMA. 2013;309:1821.7. https://doi.org/10.1001/jama.2013.3411
Maalouf FI, Cooper WO, Stratton SM, Dudley JA, Ko J, Banerji A, et al. Positive predictive value of administrative data for neonatal abstinence syndrome. Pediatrics. 2019;143:e20174183.
Acknowledgements
The authors wish to thank the Florida Agency for Healthcare Administration for their support.
Funding
This study was funded through a grant from the Florida Agency for Healthcare Administration (AHCA).
Author information
Authors and Affiliations
Contributions
JM designed the study and conducted the analyses. VS was involved in writing and formatting the manuscript. RK and TB provided guidance, feedback for the study design and analyses, and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ma, J., Sahasranaman, V., Kirby, R.S. et al. Adverse neonatal outcomes associated with maternal severe mental health diagnoses and opioid use. J Perinatol 40, 1497–1505 (2020). https://doi.org/10.1038/s41372-020-0759-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0759-1