Abstract
Objective
The purpose of this study was to describe differences and identify education gaps in the perception of palliative care (PC) between neonatal care providers in a Level IV Neonatal intensive care unit.
Study design
This is a descriptive survey mixed methods study. Email surveys were sent to social workers, pharmacists, dieticians, nurses, respiratory therapists, fellows and faculty in November of 2018. Total number of respondents was 181 with a response rate of 56%.
Results
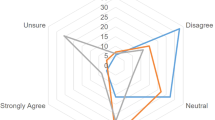
Statistically significant differences between faculty and non-faculty were found in regards to benefits of early PC consults, need for automatic consults for certain diagnosis and the frequency of PC consults.
Conclusion
The perception of PC differs greatly between faculty and non-faculty. Educational initiatives surrounding PC and communication along with instituting automatic consults for certain diagnosis could help bridge this difference in perception and educational gap.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Cortezzo DE, Sanders MR, Brownell E, Moss K. Neonatologists’ perspectives of palliative and end-of-life care in neonatal intensive care units. J Perinatol. 2013;33:731–5.
Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital- Stat Rep. 2009;57:1–134.
Carter BS, Bhatia J. Comfort/palliative care guidelines for neonatal practice: development and implementation in an academic medical center. J Perinatol. 2001;21:279–83.
Singh J, Lantos J, Meadow W. End-of-life after birth: death and dying in a neonatal intensive care unit. Pediatrics. 2004;114:1620–6.
Marc-Aurele KL, English NK. Primary palliative care in neonatal intensive care. Semin Perinatol. 2017;41:133–9.
Henner N, Boss RD. Neonatologist training in communication and palliative care. Semin Perinatol. 2017.
Section On H, Palliative M, Committee On Hospital C. Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. 2013;132:966–72.
American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics. 2000;106:351–7.
Keele L, Keenan HT, Sheetz J, Bratton SL. Differences in characteristics of dying children who receive and do not receive palliative care. Pediatrics. 2013;132:72–8.
Pierucci RL, Kirby RS, Leuthner SR. End-of-life care for neonates and infants: the experience and effects of a palliative care consultation service. Pediatrics. 2001;108:653–60.
Samsel C, Lechner BE. End-of-life care in a regional level IV neonatal intensive care unit after implementation of a palliative care initiative. J Perinatol. 2015;35:223–8.
Carter BS. Pediatric Palliative Care in Infants and Neonates. Children (Basel). 2018;5:21.
Kain V, Gardner G, Yates P. Neonatal palliative care attitude scale: development of an instrument to measure the barriers to and facilitators of palliative care in neonatal nursing. Pediatrics. 2009;123:e207–13.
Wool C. Clinician perspectives of barriers in perinatal palliative care. MCN Am J Matern Child Nurs. 2015;40:44–50.
Boss RD, Urban A, Barnett MD, Arnold RM. Neonatal Critical Care Communication (NC3): training NICU physicians and nurse practitioners. J Perinatol. 2013;33:642–6.
Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S, et al. Pediatric palliative care programs in children’s hospitals: a cross-sectional national survey. Pediatrics. 2013;132:1063–70.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276–82.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals neonatal database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Michelson KN, Steinhorn DM. Pediatric end-of-life issues and palliative care. Clin Pediatr Emerg Med. 2007;8:212–9.
Enguidanos S, Housen P, Penido M, Mejia B, Miller JA. Family members’ perceptions of inpatient palliative care consult services: a qualitative study. Palliat Med. 2014;28:42–8.
Vadeboncoeur C, McHardy M. Benefits of early referral to pediatric palliative care for a child with a rare disease. Pediatrics. 2018;141:6.
Lafond DA, Kelly KP, Hinds PS, Sill A, Michael M. Establishing feasibility of early palliative care consultation in pediatric hematopoietic stem cell transplantation. J Pediatr Oncol Nurs. 2015;32:265–77.
Nguyen LT, Cooperberg DB, Spear ML. Introduction of triggers for palliative care consultation improves utilization and satisfaction within a level four NICU. J Perinatol. 2018;38:574–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Niehaus, J.Z., Palmer, M.M., Slaven, J. et al. Neonatal palliative care: perception differences between providers. J Perinatol 40, 1802–1808 (2020). https://doi.org/10.1038/s41372-020-0714-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0714-1


