Abstract
Objective
This study examined acute findings and long-term outcome trajectories between birth and adolescence in children with prenatal opiate exposure.
Study Design
Ninety children (45 opiate-exposed, 45 non-exposed) completed assessments between 1 month and 15 years of age. Outcome variables (medical, anthropomorphic, developmental, and behavioral) were analyzed at individual time points and using longitudinal statistical modeling.
Results
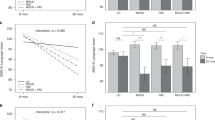
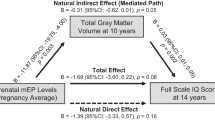
Opiate-exposed infants displayed transient neurologic findings, but no substantial signs or symptoms long term. There were no group differences in growth, cognitive functioning, or behavior at individual time periods; however, the trajectories of outcomes using longitudinal analyses adjusting for variables known to impact outcome demonstrated increased deficits among opiate-exposed children over time with regards to weight, head circumference, cognitive functioning, and behavior.
Conclusions
Findings support concerns that maternal opiate use during pregnancy may negatively impact a child’s developmental trajectory, which in turn may impose concerns to society (e.g., increased need for social, medical, and/or educational services).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Centers for Disease Control and Prevention. CDC grand rounds: prescription drug overdoses—a U.S. epidemic. MMWR Rep. 2012;61:10–3.
Hamilton KL, Harris AC, Gewirtz JC, Sparber SB, Schrott LM. HPA axis dysregulation following prenatal opiate exposure and postnatal withdrawal. Neurotoxicol Teratol. 2005;27:95–103.
McCabe SE, Cranford JA, West BT. Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: Results from two national surveys. Addict Behav. 2008;33(10):1297–305.
Hayes MJ, Brown MS. Epidemic of prescription opiate abuse and neonatal abstinence. JAMA. 2012;307:1974–1975.
Shankaran S, Lester BM, Das A, Bauer CR, Bada HS, LaGasse L, et al. Impact of maternal substance use during pregnancy on child outcome. Semin Fetal Neonatal Med. 2007;12(2):143–50.
The National Survey on Drug Use and Health. America’s behavioral health changes and challenges. Rockville: Substance Abuse and Mental Health Services Administration; 2017.
Bada HS, Bauer CR, Shankaran S, Lester B, Wright LL, Das A, et al. Central and autonomic system signs with in utero drug exposure. Arch Dis Child Fetal Neonatal Ed. 2002;87:F106–F112.
Richardson KA, Yohay ALJ, Gauda EB, McLemore GL. Neonatal animal models of opiate withdrawal. ILAR J. 2006;47:39–48.
Vathy I. Prenatal opiate exposure: long-term CNS consequences in the stress system of the offspring. Psychoneuroendocrinology. 2002;27:273–83.
Finnegan LP, Connaughton JF Jr, Kron RE, Emich JP. Neonatal abstinence syndrome: assessment and management. Addict Dis. 1975;2(1–2):141–58.
Wachman EM, Schiff DM, Silverstein M. Neonatal abstinence syndrome: advances and treatment. JAMA. 2018;39:1362–1374.
Villapiano NLG, Winkelman TNA, Kozhimannil KB, Davis MM, Patrick SW. Rural and urban differences in neonatal abstinence syndrome and maternal opioid use, 2004 to 2013. JAMA Pediatr. 2017;171:194–196.
LaGasse LL, Messinger D, Lester BM, Seifer R, Tronick EZ, Bauer CR, et al. Prenatal drug exposure and maternal and infant feeding behavior. Arch Dis Child Fetal Neonatal Ed. 2003;88:F391–9.
Hunt RW, Tzioumi D, Collins E, Jeffery HE. Adverse neurodevelopmental outcome of infants exposed to opiate in-utero. Early Hum Dev. 2008;84:29–35.
Heller NA, Logan BA, Morrison DG, Paul JA, Brown MS, Hayes MJ. Neonatal abstinence syndrome: neurobehavior at 6 weeks of age in infants with or without pharmacological treatment for withdrawal. Dev Psychobiol. 2017;59:574–82.
Hans SL. Developmental consequences of prenatal exposure to methadone. Ann NY Acad Sci. 1989;562:195–207.
Nygaard E, Moe V, Slinning K, Walhovd KB. Longitudinal cognitive development of children born to mothers with opioid and polysubstance use. Pediatr Res. 2015;78:330–5.
Towers CV, Hyatt BW, Visconti KC, Chernicky L, Chattin K, Fortner KB. Neonatal head circumference in newborns with neonatal abstinence syndrome. Pediatrics. 2019;143:e20180541.
Hudak ML, Makker K. Fetal opioid exposure and smaller birth head circumference: cause for concern? Pediatrics. 2019;143:e20183376.
Messinger DM, Bauer CR, Das A, Seifer R, Lester BM, LaGasse LL, et al. The Maternal Lifestyle Study: cognitive, motor, and behavioral outcomes of cocaine-exposed and opiate-exposed infants through three years of age. Pediatrics. 2004;113:1677–85.
Pulsifer MB, Radonovich K, Belcher HME, Butz AM. Intelligence and school readiness in preschool children with prenatal drug exposure. Child Neuropsychol. 2004;10:89–101.
Kaltenbach K, O’Grady KE, Heil SH, Salisbury AL, Coyle MG, Fischer G, et al. Prenatal exposure to methadone or buprenorphine: Early childhood developmental outcomes. Drug Alcohol Depend. 2018;185:40–49. https://doi.org/10.1016/j.drugalcdep.2017.11.030.
Davis DD, Templer DI. Neurobehavioral functioning in children exposed to narcotics in utero. Addict Behav. 1988;13(3):275–83.
Hans S. Prenatal drug exposure: behavioral functioning in late childhood and adolescence. In: Wetherington C, Smeriglio V, Finnegan L, editors. Behavioral studies of drug-exposed offspring: methodological issues in human and animal research. Rockville: US Department of Health and Human Services; 1996. p. 261–276.
Hickey JE, Suess PE, Newlin DB, Spurgeon L. Vagal tone regulation during sustained attention in boys exposed to opiates in utero. Addict Behav. 1995;2:43–59.
Suess PE, Newlin DB, Porges SW. Motivation, sustained attention, and autonomic regulation in school-age boys exposed in utero to opiates and alcohol. Exp Clin Psychopharmacol. 1997;5:375–87.
Guo X, Spencer JW, Suess PE, Hickey JE, Better WE, Herning RI. Cognitive brain potential alterations in boys exposed to opiates: in utero and lifestyle comparisons. Addict Behav. 1994;19:429–41.
Mayes, LC, Fahy, T. Prenatal drug exposure and cognitive development. In: Sternberg RJ, Grigorenko EL, editors. Environmental effects on cognitive abilities. Mahwah: Erlbaum; 2001. p. 189–220.
Oei JL, Melhuish E, Uebel H, Azzam N, Breen C, Burns L, et al. Neonatal abstinence syndrome and high school performance. Pediatrics. 2017;139:e20162651.
Bada HS, Langer J, Twomey J, Bursi C, LaGasse L, Bauer CR, et al. Importance of stability of early living arrangements on behavior outcomes of children with and without prenatal drug exposure. J Dev Behav Pediatr. 2008;29:173–82.
Bauer CR, Langer JC, Shankaran S, Bada HS, Lester B, Wright LL, et al. Acute neonatal effects of cocaine exposure during pregnancy. Arch Pediatr Adolesc Med. 2005;159:824–834.
Choo RE, Huestis MA, Schroeder JR, Shin AS, Jones HE. Neonatal abstinence syndrome in methadone-exposed infants is altered by level of prenatal tobacco exposure. Drug Alcohol Depend. 2004;75:253–60.
Griffith DR, Azuma SD, Chasnoff IJ. Three-year outcome of children exposed prenatally to drugs. J Am Acad Child Adolesc Psychiatry. 1994;33:20–7.
Hogan DM. Annotation: The psychological development and welfare of children of opiate and cocaine users: Review and research needs. J Child Psychol Psychiat. 1998;39:609–20.
Kolar AF, Brown BS, Haertzen CA, Michaelson BS. Children of substance abusers: the life experiences of children of opiate addicts in methadone maintenance. Am J Drug Alcohol Abus. 1994;20:159–71.
McGlade A, Ware R, Crawford M. Child protection outcomes for infants of substance-using mothers: a Matched-Cohort Study. Pediatrics. 2009;124:285–93.
Nair P, Rothblum S, Hebel R. Neonatal outcome in infants with evidence of fetal exposure to opiates, cocaine, and cannabinoids. Clin Pediatr. 1994;33:280–5.
Schempf AH, Strobino DM. Drug use and limited prenatal care: an examination of responsible barriers. Am J Obstet Gynecol. 2009;200:412.e1–10.
Van Baar AL, Soeptami S, Gunning WB, Akkerhuis GW. Development after prenatal exposure to cocaine, heroin, and methadone. Acta Paediatr. 1994;404 Suppl:40–6.
Sternberg RJ, Grigorenko EL, editors. Environmental effects on cognitive abilities. Erlbaum, Mahwah; 2001. p. 189– 220.
ElSohly MA, Stanford DF, Murphy TP, Lester BM, Wright LL, Smeriglio VL, et al. Immunoassay and GC-MS procedures for the analysis of drugs of abuse in meconium. J Anal Toxicol. 1999;23:436–445.
Lester BM, ElSohly M, Wright LL, Smeriglio VL, Verter J, Bauer CR, et al. The Maternal Lifestyle Study: drug use by meconium toxicology and maternal self-report. Pediatrics. 2001;107:309–317.
Bayley N. Bayley Scales of infant development. 2nd ed. San Antonio: The Psychological Corporation; 1993.
Wechsler D. Wechsler Preschool and Primary Scale of Intelligence-Revised. San Antonio, TX: Psychological Corporation; 1989.
Wechsler D. Wechsler Intelligence Scale for Children. 3rd ed. San Antonio: The Psychological Corporation; 1991.
Wechsler D. Wechsler Abbreviated Scale of Intelligence. New York: The Psychological Corporation: Harcourt Brace & Company; 1999.
Woodcock RW, McGrew KS, Mather N. Woodcock-Johnson III Tests of Achievement. Itasca: Riverside Publishing; 2001.
Lester BM, Tronick EZ. History and description of the Neonatal Intensive Care Unit Network Neurobehavioral Scale. Pediatrics. 2004;113(3):634–40.
Achenbach TM. Manual for Child Behavior Checklist/4-18 and 1991 Profile. Burlington: Univ. Vermont, Dept. of Psychiatry; 1991.
Achenbach TM. Manual for Child Behavior Checklist/2-3 and 1992 Profile. Burlington, VT: Univ. Vermont, Dept. of Psychiatry; 1992.
Sparrow SS, Balla DA, Cicchetti DV. The Vineland Adaptive Behavior Scales: Classroom Edition. Circle Pines: American Guidance Service; 1985.
SAS Version 9.3. SAS Institute Inc., Cary. 2011.
Nygaard E, Slinning K, Moe V, Walhovd KB. Behavior and attention problems in eight-year-old children with prenatal opiate and poly-substance exposure: a Longitudinal Study. PLoS ONE. 2016;11:1–21.
Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA. 2012;307:1934–1940.
Acknowledgements
Support for the Maternal Lifestyle Study was provided by the National Institutes of Health through the National Institute on Drug Abuse and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with supplemental funding from the National Institute of Mental Health, the Administration on Children, Youth, and Families and the Center for Substance Abuse and Treatment, US Department of Health and Human Services. We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. The following federal grants contributed to this study: Brown University Warren Alpert Medical School Women & Infants Hospital of Rhode Island (U10 DA24119, U10 HD27904, N01 HD23159); RTI International (U10 HD36790); University of Miami Holtz Children’s Hospital (U10 DA24118, U10 HD21397); University of Tennessee (U10 DA24128, U10 HD21415, U10 HD42638); and Wayne State University Hutzel Women’s Hospital and Children’s Hospital of Michigan (U10 DA24117, U10 HD21385).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bauer, C.R., Langer, J., Lambert-Brown, B. et al. Association of prenatal opiate exposure with youth outcomes assessed from infancy through adolescence. J Perinatol 40, 1056–1065 (2020). https://doi.org/10.1038/s41372-020-0692-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0692-3