Abstract
Objective
To assess the sound reducing characteristics of modern incubators in the neonatal intensive care unit (NICU) and to better characterize auditory and language exposures for NICU infants.
Study design
Sound frequency spectral analysis was conducted on language and noise audio acquired simultaneously inside and outside incubators located in the NICU.
Results
Sound transmission into the incubators was nonuniform. Very low-frequency sounds (<100 Hz) were unattenuated or even slightly amplified inside the incubators. Maximal reduction was observed for low-to-mid frequencies (300–600 Hz) and high frequencies (>2000 Hz), which convey important language information.
Conclusions
Sound reductions observed across NICU incubator walls are more severe than those reported for sound transmission into the intrauterine environment, particularly for midrange frequencies that are important for language. Although incubator walls may serve as a protection against noxious noise levels, these findings reveal a potentially detrimental effect on language exposure for infants inside a NICU incubator.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009;124:717–28.
Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. J Am Med Assoc. 2002;288:728–37.
Barre N, Morgan A, Doyle LW, Anderson PJ. Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J Pediatr. 2011;158:766–774 e761.
Dupin R, Laurent JP, Stauder JE, Saliba E. Auditory attention processing in 5-year-old children born preterm: evidence from event-related potentials. Dev Med Child Neurol. 2000;42:476–80.
Vohr B. Speech and language outcomes of very preterm infants. Semin Fetal Neonatal Med. 2014;19:78–83.
Pineda R, Guth R, Herring A, Reynolds L, Oberle S, Smith J. Enhancing sensory experiences for very preterm infants in the NICU: an integrative review. J Perinatol. 2017;37:323–32.
Graven SN. Sound and the developing infant in the NICU: conclusions and recommendations for care. J Perinatol. 2000;20:S88–93.
Moore JK, Linthicum FH Jr. The human auditory system: a timeline of development. Int J Audiol. 2007;46:460–78.
Hepper PG, Shahidullah BS. Development of fetal hearing. Arch Dis Child. 1994;71:F81–87.
Byers JF, Waugh WR, Lowman LB. Sound level exposure of high-risk infants in different environmental conditions. Neonatal Netw. 2006;25:25–32.
Kellam B, Bhatia J. Sound spectral analysis in the intensive care nursery: measuring high-frequency sound. J Pediatr Nurs. 2008;23:317–23.
Kent WD, Tan AK, Clarke MC, Bardell T. Excessive noise levels in the neonatal ICU: potential effects on auditory system development. J Otolaryngol. 2002;31:355–60.
Krueger C, Wall S, Parker L, Nealis R. Elevated sound levels within a busy NICU. Neonatal Netw. 2005;24:33–7.
Philbin MK, Gray L. Changing levels of quiet in an intensive care nursery. J Perinatol. 2002;22:455–60.
Levy GD, Woolston DJ, Browne JV. Mean noise amounts in level II vs level III neonatal intensive care units. Neonatal Netw. 2003;22:33–8.
Williams AL, van Drongelen W, Lasky RE. Noise in contemporary neonatal intensive care. J Acoust Soc Am. 2007;121:2681–90.
Lasky RE, Williams AL. Noise and light exposures for extremely low birth weight newborns during their stay in the neonatal intensive care unit. Pediatrics. 2009;123:540–6.
Slevin M, Farrington N, Duffy G, Daly L, Murphy JF. Altering the NICU and measuring infants’ responses. Acta Paediatr. 2000;89:577–81.
Zahr LK, Balian S. Responses of premature infants to routine nursing interventions and noise in the NICU. Nurs Res. 1995;44:179–85.
Johnson AN. Neonatal response to control of noise inside the incubator. Pediatr Nurs. 2001;27:600–5.
Gadeke R, Doring B, Keller F, Vogel A. The noise level in a childrens hospital and the wake-up threshold in infants. Acta Paediatr Scand. 1969;58:164–70.
Trapanotto M, Benini F, Farina M, Gobber D, Magnavita V, Zacchello F. Behavioural and physiological reactivity to noise in the newborn. J Paediatr Child Health. 2004;40:275–81.
Wachman EM, Lahav A. The effects of noise on preterm infants in the NICU. Arch Dis Child Fetal Neonatal Ed. 2011;96:F305–309.
Jurkovicova J, Aghova L. Evaluation of the effects of noise exposure on various body functions in low-birthweight newborns. Act Nerv Super. 1989;31:228–9.
Noise: a hazard for the fetus and the newborn. American Academy of Pediatrics CoEH. Pediatrics. 1997;100:724–7.
White RD, Smith JA, Shepley MM, Committee to Establish Recommended Standards for Newborn ICUD. Recommended standards for newborn ICU design, eighth edition. J Perinatol. 2013;33 Suppl 1:S2–16.
Wang D, Aubertin C, Barrowman N, Moreau K, Dunn S, Harrold J. Examining the effects of a targeted noise reduction program in a neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2014;99:F203–208.
Chawla S, Barach P, Dwaihy M, Kamat D, Shankaran S, Panaitescu B, et al. A targeted noise reduction observational study for reducing noise in a neonatal intensive unit. J Perinatol. 2017;37:1060–4.
Casavant SG, Bernier K, Andrews S, Bourgoin A. Noise in the neonatal intensive care unit: what does the evidence tell us? Adv Neonatal Care. 2017;17:265–73.
Jobe AH. A risk of sensory deprivation in the neonatal intensive care unit. J Pediatr. 2014;164:1265–7.
Pineda RG, Neil J, Dierker D, Smyser CD, Wallendorf M, Kidokoro H, et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J Pediatr. 2014;164:52–60 e52.
Bures Z, Popelar J, Syka J. The effect of noise exposure during the developmental period on the function of the auditory system. Hear Res. 2017;352:1–11.
Caskey M, Stephens B, Tucker R, Vohr B. Importance of parent talk on the development of preterm infant vocalizations. Pediatrics. 2011;128:910–6.
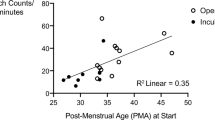
Pineda R, Durant P, Mathur A, Inder T, Wallendorf M, Schlaggar BL. Auditory exposure in the neonatal intensive care unit: room type and other predictors. J Pediatr. 2017;183:56–66 e53.
Caskey M, Stephens B, Tucker R, Vohr B. Adult talk in the NICU with preterm infants and developmental outcomes. Pediatrics. 2014;133:e578–84.
Gerhardt KJ, Abrams RM. Fetal exposures to sound and vibroacoustic stimulation. J Perinatol. 2000;20:S21–30.
Peters AJ, Gerhardt KJ, Abrams RM, Longmate JA. Three-dimensional intraabdominal sound pressures in sheep produced by airborne stimuli. Am J Obstet Gynecol. 1993;169:1304–15.
Richards DS, Frentzen B, Gerhardt KJ, McCann ME, Abrams RM. Sound levels in the human uterus. Obstet Gynecol. 1992;80:186–90.
Robertson SJ, Burnashev N, Edwards FA. Ca2+ permeability and kinetics of glutamate receptors in rat medial habenula neurones: implications for purinergic transmission in this nucleus. J Physiol. 1999;518:539–49.
Wubben SM, Brueggeman PM, Stevens DC, Helseth CC, Blaschke K. The sound of operation and the acoustic attenuation of the Ohmeda Medical Giraffe OmniBed. Noise Health. 2011;13:37–44.
Monson BB, Lotto AJ, Story BH. Analysis of high-frequency energy in long-term average spectra of singing, speech, and voiceless fricatives. J Acoust Soc Am. 2012;132:1754–64.
DeCasper AJ, Fifer WP. Of human bonding: newborns prefer their mothers’ voices. Science. 1980;208:1174–6.
Decasper AJ, Spence MJ. Prenatal maternal speech influences newborns perception of speech sounds. Infant Behav Dev. 1986;9:133–50.
Moon C, Cooper RP, Fifer WP. 2-day-olds prefer their native language. Infant Behav Dev. 1993;16:495–500.
Moon C, Lagercrantz H, Kuhl PK. Language experienced in utero affects vowel perception after birth: a two-country study. Acta Paediatr. 2013;102:156–60.
Querleu D, Renard X, Versyp F, Paris-Delrue L, Crepin G. Fetal hearing. Eur J Obstet, Gynecol, Reprod Biol. 1988;28:191–212.
French NR, Steinberg JC. Factors governing the intelligibility of speech sounds. J Acoust Soc Am. 1947;19:90–119.
Hillenbrand J, Getty LA, Clark MJ, Wheeler K. Acoustic characteristics of American english vowels. J Acoust Soc Am. 1995;97:3099–111.
Remez RE, Rubin PE, Pisoni DB, Carrell TD. Speech perception without traditional speech cues. Science. 1981;212:947–9.
Mann VA. Influence of preceding liquid on stop-consonant perception. Percept Psychophys. 1980;28:407–12.
Miyawaki K, Jenkins J, Strange W, Liberman A, Verbrugge R, Fujimura O. An effect of linguistic experience: The discrimination of [r] and [l] by native speakers of Japanese and English. Percept Psychophys. 1975;18:331–40.
Sher AE, Owens E. Consonant confusions associated with hearing loss above 2000 Hz. J Speech Hear Res. 1974;17:669–81.
Doheny L, Morey JA, Ringer SA, Lahav A. Reduced frequency of apnea and bradycardia episodes caused by exposure to biological maternal sounds. Pediatr Int. 2012;54:e1–3.
Doheny L, Hurwitz S, Insoft R, Ringer S, Lahav A. Exposure to biological maternal sounds improves cardiorespiratory regulation in extremely preterm infants. J Matern Fetal Neonatal Med. 2012;25:1591–4.
Zimmerman E, Keunen K, Norton M, Lahav A. Weight gain velocity in very low-birth-weight infants: effects of exposure to biological maternal sounds. Am J Perinatol. 2013;30:863–70.
Chorna OD, Slaughter JC, Wang L, Stark AR, Maitre NL. A pacifier-activated music player with mother’s voice improves oral feeding in preterm infants. Pediatrics. 2014;133:462–8.
Loewy J, Stewart K, Dassler AM, Telsey A, Homel P. The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics. 2013;131:902–18.
Acknowledgements
This study was supported by a grant from the Center for Health, Aging and Disabilities in the College of Applied Health Sciences, University of Illinois at Urbana-Champaign. The authors thank the Carle NICU staff for assistance with set up.
Funding
This study was supported by a grant from the Center for Health, Aging and Disabilities in the College of Applied Health Sciences, University of Illinois at Urbana-Champaign.
Author information
Authors and Affiliations
Contributions
BBM conceptualized and designed the study, collected the data, carried out the analysis, drafted the initial manuscript, and revised the manuscript. JR collected the data, drafted the initial manuscript, and revised the manuscript. MC collected the data and revised the manuscript. VS designed the study, coordinated data collection, and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose. The authors have no financial relationships relevant to this article to disclose. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Monson, B.B., Rock, J., Cull, M. et al. Neonatal intensive care unit incubators reduce language and noise levels more than the womb. J Perinatol 40, 600–606 (2020). https://doi.org/10.1038/s41372-020-0592-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0592-6