Abstract
Objective
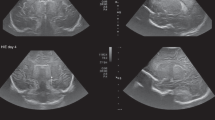
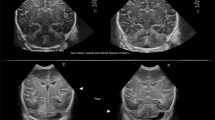
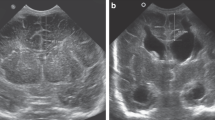
Intraventricular hemorrhage (IVH) is a complication of prematurity. Grades III and IV IVH lead to significant morbidity, but mounting evidence shows low-grade IVH (grades I–II) may be associated with adverse sequelae. Head ultrasounds (HUS) are used to screen infants for IVH but may miss low-grade IVH. Our study compared the results of HUS around 7 days of age to susceptibility-weighted imaging (SWI) obtained at term-corrected age in infants born at <30 wGA.
Study design
Infants <30 weeks gestational age (GA) with an HUS and MRI at admission to UF Health were identified by a retrospective chart review. Images were re-read by a pediatric neuroradiologist.
Results
Ninety-four infants with a mean GA of 25.8 weeks were identified. Of those with normal HUS, 50% had low-grade IVH on the term-corrected MRI.
Conclusions
HUS are effective for screening for high-grade IVH. SWI is more sensitive in identifying low-grade IVH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Roberts J, Javed M, Hocker J, Wang H, Tarantino M. Risk factors associated with intraventricular hemorrhage in extremely premature neonates. Blood Coagul Fibrinolysis. 2018;29:25–9.
Szpecht D, Szymankiewicz M, Nowak I, Gadzinowski J. Intraventricular hemorrhage in neonates born before 32 weeks of gestation-retrospective analysis of risk factors. Childs Nerv Syst. 2016;32:1399–404.
Ment LR, Oh W, Ehrenkranz RA, Philip AG, Duncan CC, Makuch RW. Antenatal steroids, delivery mode, and intraventricular hemorrhage in preterm infants. Am J Obstet Gynecol. 1995;172:795–800.
Humberg A, Härtel C, Paul P, Hanke K, Bossung V, Hartz A, et al. Delivery mode and intraventricular hemorrhage risk in very-low-birth-weight infants: Observational data of the German Neonatal Network. Eur J Obstet Gynecol Reprod Biol. 2017;212:144–9.
Mohamed MA, Aly H. Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 2010;95:F403–407.
Futagi Y, Toribe Y, Ogawa K, Suzuki Y. Neurodevelopmental outcome in children with intraventricular hemorrhage. Pediatric Neurol. 2006;34:219–24.
Patra K, Wilson-Costello D, Taylor HG, Mercuri-Minich N, Hack M. Grades I-II intraventricular hemorrhage in extremely low birth weight infants: effects on neurodevelopment. J Pediatr. 2006;149:169–73.
Klebermass-Schrehof K, Czaba C, Olischar M, Fuiko R, Waldhoer T, Rona Z, et al. Impact of low-grade intraventricular hemorrhage on long-term neurodevelopmental outcome in preterm infants. Childs Nerv Syst. 2012;28:2085–92.
Vohr BR, Allan W, Katz KH, Schneider K, Tucker R, Ment LR. Adolescents born prematurely with isolated grade 2 haemorrhage in the early 1990s face increased risks of learning challenges. Acta Paediatr. 2014;103:1066–71.
Vasileiadis GT, Gelman N, Han VK, Williams LA, Mann R, Bureau Y, et al. Uncomplicated intraventricular hemorrhage is followed by reduced cortical volume at near-term age. Pediatrics. 2004;114:e367–372.
Maalouf EF, Duggan PJ, Counsell SJ, Rutherford MA, Cowan F, Azzopardi D, et al. Comparison of findings on cranial ultrasound and magnetic resonance imaging in preterm infants. Pediatrics. 2001;107:719–27.
Tong KA, Ashwal S, Obenaus A, Nickerson JP, Kido D, Haacke EM. Susceptibility-weighted MR imaging: a review of clinical applications in children. AJNR Am J Neuroradiol. 2008;29:9–17.
Schelhorn J, Gramsch C, Deuschl C, Quick HH, Nensa F, Moenninghoff C, et al. Intracranial hemorrhage detection over time using susceptibility-weighted magnetic resonance imaging. Acta Radio. 2015;56:1501–7.
Neubauer V, Djurdjevic T, Griesmaier E, Biermayr M, Gizewski ER, Kiechl-Kohlendorfer U. Routine magnetic resonance imaging at term-equivalent age detects brain injury in 25% of a contemporary cohort of very preterm infants. PLoS ONE. 2017;12:e0169442.
Gomori JM, Grossman RI. Mechanisms responsible for the MR appearance and evolution of intracranial hemorrhage. Radiographics. 1988;8:427–40.
Rutherford M. Hemorrhagic lesions of the newborn brain. MRI of the Neonatal Brain, 4 ed. London, United Kingdom: Saunders Ltd; 2001.
Meoded A, Poretti A, Northington FJ, Tekes A, Intrapiromkul J, Huisman TA. Susceptibility weighted imaging of the neonatal brain. Clin Radio. 2012;67:793–801.
Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med. 2006;355:685–94.
de Vries LS, Benders MJ, Groenendaal F. Imaging the premature brain: ultrasound or MRI? Neuroradiology. 2013;55:13–22.
Ho T, Dukhovny D, Zupancic JA, Goldmann DA, Horbar JD, Pursley DM. Choosing wisely in newborn medicine: five opportunities to increase value. Pediatrics. 2015;136:e482–489.
Pearce R, Baardsnes J. Term MRI for small preterm babies: do parents really want to know and why has nobody asked them? Acta Paediatr. 2012;101:1013–5.
Levene MI, Fawer CL, Lamont RF. Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Arch Dis Child. 1982;57:410–7.
Vollmer B, Roth S, Baudin J, Stewart AL, Neville BG, Wyatt JS. Predictors of long-term outcome in very preterm infants: gestational age versus neonatal cranial ultrasound. Pediatrics. 2003;112:1108–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nataraj, P., Svojsik, M., Sura, L. et al. Comparing head ultrasounds and susceptibility-weighted imaging for the detection of low-grade hemorrhages in preterm infants. J Perinatol 41, 736–742 (2021). https://doi.org/10.1038/s41372-020-00890-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00890-x
This article is cited by
-
Incidence of brain injuries in a large cohort of very preterm and extremely preterm infants at term-equivalent age: results of a single tertiary neonatal care center over 10 years
European Radiology (2024)
-
The diagnostic value of susceptibility-weighted imaging for identifying acute intraarticular hemorrhages
Skeletal Radiology (2022)