Abstract
Objective
To compare outcomes of twin-twin transfusion syndrome (TTTS) patients who underwent early elective delivery vs. expectant management.
Study design
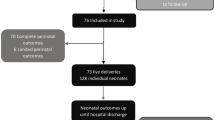
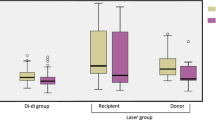
Retrospective study of monochorionic diamniotic twins who underwent laser surgery for TTTS and had dual survivors at 32 weeks. Patients who underwent elective delivery between 32 0/7 to 35 6/7 weeks (“early elective group”) were compared with all patients who delivered ≥36 0/7 weeks (“expectant management group”). The primary outcome was a composite of fetal and neonatal morbidity.
Results
The final study population was comprised of 15 early elective and 119 expectant management patients. Those in the early elective group were seven times more likely to experience the primary outcome (OR 7.38 [2.01–27.13], p = 0.0026).
Conclusion
Among patients who underwent laser surgery for TTTS who had dual survivors at 32 weeks, elective delivery prior to 36 weeks did not appear to be protective.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Danon D, Sekar R, Hack KE, Fisk NM. Increased stillbirth in uncomplicated monochorionic twin pregnancies: a systematic review and meta-analysis. Obstet Gynecol. 2013;121:1318–26.
Simoes T, Amaral N, Lerman R, Ribeiro F, Dias E, Blickstein I. Prospective risk of intrauterine death of monochorionic-diamniotic twins. Am J Obstet Gynecol. 2006;195:134–9.
Sullivan AE, Hopkins PN, Weng HY, Henry E, Lo JO, Varner MW, et al. Delivery of monochorionic twins in the absence of complications: analysis of neonatal outcomes and costs. Am J Obstet Gynecol. 2012;206:257 e251–257.
Stephens AS, Lain SJ, Roberts CL, Bowen JR, Nassar N. Survival, hospitalization, and acute-care costs of very and moderate preterm infants in the first 6 years of life: a population-based study. J Pediatr. 2016;169:61–68 e63.
Boyle EM, Poulsen G, Field DJ, Kurinczuk JJ, Wolke D, Alfirevic Z, et al. Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. Brit Med J. 2012;344:e896.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196:147 e141–148.
Burgess JL, Unal ER, Nietert PJ, Newman RB. Risk of late-preterm stillbirth and neonatal morbidity for monochorionic and dichorionic twins. Am J Obstet Gynecol. 2014;210:578 e571–579.
Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics. 2006;118:1207–14.
Cheong-See F, Schuit E, Arroyo-Manzano D, Khalil A, Barrett J, Joseph KS, et al. Prospective risk of stillbirth and neonatal complications in twin pregnancies: systematic review and meta-analysis. Brit Med J. 2016;354:i4353.
Lee YM, Wylie BJ, Simpson LL, D’Alton ME. Twin chorionicity and the risk of stillbirth. Obstet Gynecol. 2008;111(2 Pt 1):301–8.
ACOG Committee Opinion No. 764. Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2019;133:e151–e155.
Committee on Practice B-O, Society for Maternal-Fetal M. Practice Bulletin No. 169: multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2016;128:e131–146.
Barigye O, Pasquini L, Galea P, Chambers H, Chappell L, Fisk NM. High risk of unexpected late fetal death in monochorionic twins despite intensive ultrasound surveillance: a cohort study. PLoS Med. 2005;2:e172.
Practice bulletin no. 169. Summary: multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2016;128:926–8.
Newman RB, Unal ER. Multiple gestations: timing of indicated late preterm and early-term births in uncomplicated dichorionic, monochorionic, and monoamniotic twins. Semin Perinatol. 2011;35:277–85.
Unal ER. Fetal surveillance and timing of delivery for multiples. Clin Obstet Gynecol. 2015;58:676–89.
Cleary-Goldman J, D’Alton ME. Uncomplicated monochorionic diamniotic twins and the timing of delivery. PLoS Med. 2005;2:e180.
Emery SP, Bahtiyar MO, Moise KJ. The north american fetal therapy network consensus statement: management of complicated monochorionic gestations. Obstet Gynecol. 2015;126:575–84.
Society for Maternal-Fetal M, Simpson LL. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 2013;208:3–18.
Bahtiyar MO, Emery SP, Dashe JS, Wilkins-Haug LE, Johnson A, Paek BW, et al. The North American fetal therapy network consensus statement: prenatal surveillance of uncomplicated monochorionic gestations. Obstet Gynecol. 2015;125:118–23.
Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999;19(8 Pt 1):550–5.
Chmait RH, Kontopoulos EV, Korst LM, Llanes A, Petisco I, Quintero RA. Stage-based outcomes of 682 consecutive cases of twin-twin transfusion syndrome treated with laser surgery: the USFetus experience. Am J Obstet Gynecol. 2011;204:393 e391–396.
Quintero RA, Ishii K, Chmait RH, Bornick PW, Allen MH, Kontopoulos EV. Sequential selective laser photocoagulation of communicating vessels in twin-twin transfusion syndrome. J Matern Fetal Neonatal Med. 2007;20:763–8.
Ruano R, Rodo C, Peiro JL, Shamshirsaz AA, Haeri S, Nomura ML, et al. Fetoscopic laser ablation of placental anastomoses in twin-twin transfusion syndrome using ‘Solomon technique’. Ultrasound Obstet Gynecol. 2013;42:434–9.
Gordon BJ, Chon AH, Korst LM, Llanes A, Miller DA, Chmait RH. Incidental septostomy after laser surgery for twin-twin transfusion syndrome: perinatal outcomes and antenatal management. Fetal Diagn Ther. 2018;44:285–90.
Caughey AB, Sundaram V, Kaimal AJ, Cheng YW, Gienger A, Little SE, et al. Maternal and neonatal outcomes of elective induction of labor. Evid Rep Technol Assess (Full Rep). 2009;176:1–257.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84.
Breathnach FM, McAuliffe FM, Geary M, Daly S, Higgins JR, Dornan J, et al. Optimum timing for planned delivery of uncomplicated monochorionic and dichorionic twin pregnancies. Obstet Gynecol. 2012;119:50–9.
Hernandez GD, Korst LM, Goodwin TM, Miller DA, Caughey AB, Ouzounian JG. Late pregnancy complications can affect risk estimates of elective induction of labor. J Matern Fetal Neonatal Med. 2011;24:787–94.
Korst LM, Fridman M, Lu MC, Mitchell C, Lawton E, Griffin F, et al. Monitoring childbirth morbidity using hospital discharge data: further development and application of a composite measure. Am J Obstet Gynecol. 2014;211:268 e261–268 e216.
Stirnemann JJ, Quibel T, Essaoui M, Salomon LJ, Bussieres L, Ville Y. Timing of delivery following selective laser photocoagulation for twin-to-twin transfusion syndrome. Am J Obstet Gynecol. 2012;207:127 e121–126.
Jopling J, Henry E, Wiedmeier SE, Christensen RD. Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics. 2009;123:e333–337.
American College of O, Gynecologists. ACOGcommittee opinion no. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121:911–5.
Refuerzo JS. Impact of multiple births on late and moderate prematurity. Semin Fetal Neonatal Med. 2012;17:143–5.
Kosinska-Kaczynska K, Szymusik I, Bomba-Opon D, Madej A, Oleszczuk J, Patro-Malysza J, et al. Late prematurity in twins: a polish multicenter study. Twin Res Hum Genet. 2014;17:369–75.
Harijan P, Boyle EM. Health outcomes in infancy and childhood of moderate and late preterm infants. Semin Fetal Neonatal Med. 2012;17:159–62.
Zaretsky MV, Tong S, Lagueux M, Lim F-Y, Khalek N, Emery SP, et al. North American Fetal Therapy Network: timing of and indications for delivery following laser ablation for twin-twin transfusion syndrome. Am J Obstet Gynecol MFM. 2019;1:74–81.
Luke B, Brown MB, Alexandre PK, Kinoshi T, O’Sullivan MJ, Martin D, et al. The cost of twin pregnancy: maternal and neonatal factors. Am J Obstet Gynecol. 2005;192:909–15.
Nist MD, Rodgers EA, Ruth BM, Bertoni CB, Bartman T, Keller LA, et al. Skin rounds: a quality improvement approach to enhance skin care in the neonatal intensive care unit. Adv Neonatal Care. 2016;16 Suppl 5S:S33–S41.
Bennett NJ, Tabarani CM, Bartholoma NM, Wang D, Huang D, Riddell SW, et al. Unrecognized viral respiratory tract infections in premature infants during their birth hospitalization: a prospective surveillance study in two neonatal intensive care units. J Pediatr. 2012;161:814–8.
Civardi E, Tzialla C, Baldanti F, Strocchio L, Manzoni P, Stronati M. Viral outbreaks in neonatal intensive care units: what we do not know. Am J Infect Control. 2013;41:854–6.
Soares BN, Pissarra S, Rouxinol-Dias AL, Costa S, Guimaraes H. Complications of central lines in neonates admitted to a level III Neonatal Intensive Care Unit. J Matern Fetal Neonatal Med. 2018;31:2770–6.
Sekar KC. Iatrogenic complications in the neonatal intensive care unit. J Perinatol. 2010;30:Suppl: S51–56.
Al Maghaireh DF, Abdullah KL, Chan CM, Piaw CY, Al Kawafha MM. Systematic review of qualitative studies exploring parental experiences in the Neonatal Intensive Care Unit. J Clin Nurs. 2016;25:2745–56.
Alkozei A, McMahon E, Lahav A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J Matern Fetal Neonatal Med. 2014;27:1738–43.
Zhang H, Zhang J, Zhao S. Airway damage of prematurity: the impact of prolonged intubation, ventilation, and chronic lung disease. Semin Fetal Neonatal Med. 2016;21:246–53.
Keszler M. Mechanical ventilation strategies. Semin Fetal Neonatal Med. 2017;22:267–74.
Wesley JR. Efficacy and safety of total parenteral nutrition in pediatric patients. Mayo Clin Proc. 1992;67:671–5.
Assaf SA, Korst LM, Chmait RH. Normalization of amniotic fluid levels after fetoscopic laser surgery for twin-twin transfusion syndrome. J Ultrasound Med. 2010;29:1431–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Portions of this manuscript were presented in Abstract # 220 Poster Session I at the Society for Maternal-Fetal Medicine 38th Annual Pregnancy Meeting, Dallas, Texas from January 29—February 3, 2018.
Rights and permissions
About this article
Cite this article
Chon, A.H., Chang, M.R., Chmait, H.R. et al. Delivery timing after laser surgery for twin-twin transfusion syndrome. J Perinatol 40, 248–255 (2020). https://doi.org/10.1038/s41372-019-0532-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0532-5