Abstract
Objective
The objective of this study was to use current national data to evaluate the characteristics and survival trends of preterm infants born with CDH from 2004 to 2014.
Study design
Data was queried from the National Inpatient Sample (NIS) and KID database from 2004 to 2014. Infants were included if diagnosed with CDH by ICD-9 coding and gestational age <37 weeks. Descriptive statistics, chi-square, and trend analysis were completed.
Results
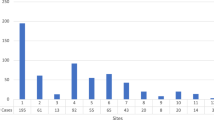
We identified 2356 infants born prematurely with CDH. The overall survival rate was 49%. The survival range is 21.2–62.3% for gestational age <26 weeks to 35–36 weeks, respectively. Total mortality was 1183; of them, 1052 (89%) were not repaired and 363 (30.7%) did not receive mechanical ventilation. Surgical repair occurred in 55.1% of infants.
Conclusions
Preterm infants have lower survival compared with term infants. Survival rates decrease with lower gestational age and have improved over time.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Langham MR Jr., Kays DW, Ledbetter DJ, Frentzen B, Sanford LL, Richards DS. Congenital diaphragmatic hernia. Epidemiology and outcome. Clin Perinatol. 1996;23:671–88.
Balayla J, Abenhaim HA. Incidence, predictors and outcomes of congenital diaphragmatic hernia: a population-based study of 32 million births in the United States. J Matern Fetal Neonatal Med. 2014;27:1438–44.
Zani-Ruttenstock E, Zani A, Eaton S, Fecteau A. First population-based report of infants with congenital diaphragmatic hernia: 30-day outcomes from the American College of Surgeons National Quality Improvement Program. Eur J Pediatr Surg. 2019;29:62–7.
Grover TR, Murthy K, Brozanski B, Gien J, Rintoul N, Keene S, et al. Short-term outcomes and medical and surgical interventions in infants with congenital diaphragmatic hernia. Am J Perinatol. 2015;32:1038–44.
O’Mahony E, Stewart M, Sampson A, East C, Palma-Dias R. Perinatal outcome of congenital diaphragmatic hernia in an Australian tertiary hospital. Aust N Z J Obstet Gynaecol. 2012;52:189–94.
Tsao K, Allison ND, Harting MT, Lally PA, Lally KP. Congenital diaphragmatic hernia in the preterm infant. Surgery. 2010;148:404–10.
Danzer E, Gerdes M, D’Agostino JA, Bernbaum J, Hoffman C, Herkert LM, et al. Younger gestational age is associated with increased risk of adverse neurodevelopmental outcome during infancy in congenital diaphragmatic hernia. J Pediatr Surg. 2016;51:1084–90.
Lally KP, Lally PA, Langham MR, Hirschl R, Moya FR, Tibboel D, et al. Surfactant does not improve survival rate in preterm infants with congenital diaphragmatic hernia. J Pediatr Surg. 2004;39:829–33.
Vieira R, Pearse R, Rankin J. Mortality factors in infants with congenital diaphragmatic hernia: a systematic review. Birth Defects Res. 2018;110:1241–9.
Yamoto M, Tanaka Y, Fukumoto K, Miyake H, Nakajima H, Koyama M, et al. Cardiac fetal ultrasonographic parameters for predicting outcomes of isolated left-sided congenital diaphragmatic hernia. J Pediatr Surg. 2015;50:2019–24.
Yang SH, Nobuhara KK, Keller RL, Ball RH, Goldstein RB, Feldstein VA, et al. Reliability of the lung-to-head ratio as a predictor of outcome in fetuses with isolated left congenital diaphragmatic hernia at gestation outside 24-26 weeks. Am J Obstet Gynecol. 2007;197:30 e31–37.
Hidaka N, Ishii K, Furutake Y, Yamamoto R, Sasahara J, Mitsuda N. Magnetic resonance fetal right lung volumetry and its efficacy in predicting postnatal short-term outcomes of congenital left-sided diaphragmatic hernia. J Obstet Gynaecol Res. 2014;40:429–38.
Stranak Z, Krofta L, Haak LA, Vojtech J, Haslik L, Rygl M, et al. Antenatal assessment of liver position, rather than lung-to-head ratio (LHR) or observed/expected LHR, is predictive of outcome in fetuses with isolated left-sided congenital diaphragmatic hernia. J Matern Fetal Neonatal Med. 2017;30:74–8.
Sananes N, Britto I, Akinkuotu AC, Olutoye OO, Cass DL, Sangi-Haghpeykar H, et al. Improving the prediction of neonatal outcomes in isolated left-sided congenital diaphragmatic hernia by direct and indirect sonographic assessment of liver herniation. J Ultrasound Med. 2016;35:1437–43.
Agency for Healthcare Research and Quality. HCUP kids’ inpatient database (KID). Healthcare Cost and Untilization Project (HCUP). Agency for Healthcare Research and Quality; 2004–12. https://www.hcup-us.ahrq.gov/kidoverview.jsp.
Agency for Heathcare Research and Quality. HCUP National Inpatient Sample (NIS). Healthcare Utilization Project (HCUP). Agency for Healthcare Research and Quality; 2004–12. https://www.hcup-us.ahrq.gov/nisoverview.jsp.
Aly H, Bianco-Batlles D, Mohamed MA, Hammad TA. Mortality in infants with congenital diaphragmatic hernia: a study of the United States National Database. J Perinatol. 2010;30:553–7.
Chien LY, Whyte R, Aziz K, Thiessen P, Matthew D, Lee SK. Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol. 2001;98:247–52.
Author information
Authors and Affiliations
Contributions
AP: conceptualized the study, and drafted and reviewed the manuscript. HO: carried out the initial analyses, and reviewed and revised the manuscript. IS: reviewed and revised the manuscript. EE: reviewed and revised the manuscript. NY: contributed expertize content and critically reviewed the manuscript. HA: conceptualized and designed the study and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peluso, A.M., Othman, H.F., Elsamny, E.M. et al. Survival trends and outcomes among preterm infants with congenital diaphragmatic hernia. J Perinatol 40, 263–268 (2020). https://doi.org/10.1038/s41372-019-0523-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0523-6
This article is cited by
-
Outcomes of congenital diaphragmatic hernia among preterm infants: inverse probability of treatment weighting analysis
Journal of Perinatology (2023)
-
The Utility of Serial Echocardiography Parameters in Management of Newborns with Congenital Diaphragmatic Hernia (CDH) and Predictors of Mortality
Pediatric Cardiology (2023)