Abstract
Objective
To determine the relationship between nutritive sucking and microstructural integrity of sensorimotor tracts in newborns with brain injury.
Study design
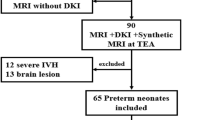
Diffusion imaging was performed in ten newborns with brain injury. Nutritive sucking was assessed using Nfant®. The motor, sensory, and corpus callosum tracts were reconstructed via tractography. Fractional anisotropy, radial, axial, and mean diffusivity were estimated for these tracts. Multiple regression models were developed to test the association between sucking features and diffusion parameters.
Results
Low-sucking smoothness correlated with low-fractional anisotropy of motor tracts (p = 0.0096). High-sucking irregularity correlated with high-mean diffusivity of motor (p = 0.030) and corpus callosum tracts (p = 0.032). For sensory tracts, high-sucking irregularity (p = 0.018) and low-smoothness variability (p = 0.002) correlated with high-mean diffusivity.
Interpretation
We show a correlation between neuroimaging-demonstrated microstructural brain abnormalities and variations in sucking patterns of newborns. The consistency of this relationship should be shown on larger cohorts.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Code availability
The MATLAB code for the nutritive sucking analyses is available upon request.
References
American Academy of Pediatrics. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Browne JV, Ross ES. Eating as a neurodevelopmental process for high-risk newborns. Clin Perinatol. 2011;38:731–43.
Muscatelli F, Bouret SG. Wired for eating: how is an active feeding circuitry established in the postnatal brain? Curr Opin Neurobiol. 2018;52:165–71.
LaMantia AS, Moody SA, Maynard TM, Karpinski BA, Zohn IE, Mendelowitz D, et al. Hard to swallow: developmental biological insights into pediatric dysphagia. Dev Biol. 2016;409:329–42.
Poore MA, Barlow SM. Suck predicts neuromotor integrity and developmental outcomes. Perspect Speech Sci Orofac Disord. 2009;19:44–51.
Barkat-Masih M, Saha C, Hamby DK, Ofner S, Golomb MR. Feeding problems in children with neonatal arterial ischemic stroke. J Child Neurol. 2010;25:867–72.
Quattrocchi CC, Longo D, Delfino LN, Cilio MR, Piersigilli F, Capua MD, et al. Dorsal brain stem syndrome: MR imaging location of brain stem tegmental lesions in neonates with oral motor dysfunction. Am J Neuroradiol. 2010;31:1438–42.
Mizuno K, Ueda A. Neonatal feeding performance as a predictor of neurodevelopmental outcome at 18 months. Dev Med Child Neurol. 2005;47:299–304.
Reilly S, Skuse D, Poblete X. Prevalence of feeding problems and oral motor dysfunction in children with cerebral palsy: a community survey. J Pediatr. 1996;129:877–82.
Slattery J, Morgan A, Douglas J. Early sucking and swallowing problems as predictors of neurodevelopmental outcome in children with neonatal brain injury: a systematic review. Dev Med Child Neurol. 2012;54:796–806.
Bickell M, Barton C, Dow K, Fucile S. A systematic review of clinical and psychometric properties of infant oral motor feeding assessments. Devl Neurorehabil. 2018;21:351–61.
Tsai SW, Chen CH, Lin MC. Prediction for developmental delay on Neonatal Oral Motor Assessment Scale in preterm infants without brain lesion. Pedia Int. 2010;52:65–8. [PubMed: 19400913]
Wolthuis-Stigter MI, Luinge MR, da Costa SP, Krijnen WP, van der Schans CP, Bos AF. The association between sucking behavior in preterm infants and neurodevelopmental outcomes at 2 years of age. J Pedia. 2015;166:26–30.
Zhang X, Zhou M, Yin H, Dai Y, Li Y. The predictive value of early oral motor assessments for neurodevelopmental outcomes of moderately and late preterm infants. Medicine. 2017;96:e9207.
Medoff-Cooper B, Shults J, Kaplan J. Sucking behavior of preterm neonates as a predictor of developmental outcomes. J Dev Behav Pedia. 2009;30:16–22. [PubMed: 19194323]
Tamilia E, Taffoni F, Formica D, Ricci L, Schena E, Keller F, et al. Technological solutions and main indices for the assessment of newborns’ nutritive sucking: a review. Sensors. 2014;14:634–58.
Tamilia E, Formica D, Scaini A, Taffoni F. An automated system for the analysis of newborns’ oral-motor behavior. IEEE Trans Neural Syst Rehabil Eng. 2016;24:1294–303.
Capilouto GJ, Cunningham TJ, Mullineaux DR, Tamilia E, Papadelis C, Giannone PJ. Quantifying neonatal sucking performance: promise of new methods. Semin Speech Lang. 2017;38:147–58.
Tamilia E, Formica D, Visco AM, Scaini A, Taffoni F. An automated system for quantitative analysis of newborns’ oral-motor behavior and coordination during bottle feeding. In: 2015 37th Conf Proc IEEE Eng Med Biol Soc (EMBC), 25 Aug 2015. IEEE Milano, Italy; 2015 p. 7386–9.
Inder TE, Anderson NJ, Spencer C, Wells S, Volpe JJ. White matter injury in the premature infant: a comparison between serial cranial sonographic and MR findings at term. Am J Neuroradiol. 2003;24:805–9.
Wimberger DM, Roberts TP, Barkovich AJ, Prayer LM, Moseley ME, Kucharczyk J. Identification of” premyelination” by diffusion-weighted MRI. J Comput Assist Tomogr. 1995;19:28–33.
Berman JI, Mukherjee P, Partridge SC, Miller SP, Ferriero DM, Barkovich AJ, et al. Quantitative diffusion tensor MRI fiber tractography of sensorimotor white matter development in premature infants. Neuroimage. 2005;27:862–71.
Capilouto GJ, Cunningham TJ, Giannone PJ, Grider D. A comparison of the nutritive sucking performance of full term and preterm neonates at hospital discharge: a prospective study. Early Hum Dev. 2019;134:26–30.
Soares J, Marques P, Alves V, Sousa N. A hitchhiker’s guide to diffusion tensor imaging. Front Neurosci. 2013;7:31.
Amaizu N, Shulman RJ, Schanler RJ, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008;97:61–7.
Woolrich MW, Jbabdi S, Patenaude B, Chappell M, Makni S, Behrens T, et al. Bayesian analysis of neuroimaging data in FSL. NeuroImage. 2009;45:S173–86.
Behrens TE, Berg HJ, Jbabdi S, Rushworth MF, Woolrich MW. Probablistic diffusion tractography with multiple fibre orientations: what can we gain? NeuroImage. 2007;34:144–55.
Papadelis C, Butler EE, Rubenstein M, Sun L, Zollei L, Nimec D, et al. Reorganization of the somatosensory cortex in hemiplegic cerebral palsy associated with impaired sensory tracts. NeuroImage: Clin. 2018;17:198–212.
Oishi K, Mori S, Donohue PK, Ernst T, Anderson L, Buchthal S, et al. Multi-contrast human neonatal brain atlas: application to normal neonate development analysis. Neuroimage. 2011;56:8–20.
Guye M, Parker GJ, Symms M, Boulby P, Wheeler-Kingshott CA, Salek-Haddadi A, et al. Combined functional MRI and tractography to demonstrate the connectivity of the human primary motor cortex in vivo. Neuroimage. 2003;19:1349–60.
Fiori S, Guzzetta A. Plasticity following early-life brain injury: insights from quantitative MRI. Semin Perinatol. 2015;39:141–6.
Balasubramanian S, Melendez-Calderon A, Roby-Brami A, Burdet E. On the analysis of movement smoothness. J Neuroeng Rehabil. 2015;12:112.
Burdet E, Milner TE. Quantization of human motions and learning of accurate movements. Biol Cybern. 1998;78:307–18.
Burdet E, Franklin DW, Milner TE. Human robotics: neuromechanics and motor control. MIT press, Cambridge, MA, USA; 2013.
Tamilia E, Delafield J, Fiore S, Taffoni F. An automatized system for the assessment of nutritive sucking behavior in infants: a preliminary analysis on term neonates. In: 2014 36th Conf Proc IEEE Eng Med Biol Soc (EMBC), 26 Aug 2014. IEEE, Chicago, Illinois, USA; 2014. p. 5752–55.
Pierpaoli C, Basser PJ. Toward a quantitative assessment of diffusion anisotropy. Magn Reson Med. 1996;36:893–906.
Seki K, Fetz EE. Gating of sensory input at spinal and cortical levels during preparation and execution of voluntary movement. J Neurosci. 2012;32:890–902.
Hadders-algra M. Early human motor development: from variation to the ability to vary and adapt. Neurosci Biobehav Rev. 2018;90:411–27.
Eishima K. The analysis of sucking behaviour in newborn infants. Early Hum Dev. 1991;27:163–73.
Fabri M, Polonara G. Functional topography of human corpus callosum: an FMRI mapping study. Neural Plast. 2013;2013:251308.
Fabri M, Polonara G, Quattrini A, Salvolini U, Del Pesce M, Manzoni T. Role of the corpus callosum in the somatosensory activation of the ipsilateral cerebral cortex: an fMRI study of callosotomized patients. Eur J Neurosci. 1999;11:3983–94.
Hynd GW, Semrud-Clikeman M, Lorys AR, Novey ES, Eliopulos D, Lyytinen H. Corpus callosum morphology in attention deficit-hyperactivity disorder: morphometric analysis of MRI. J Learn Disabil. 1991;24:141–6.
Bancroft TW, Ian CP. Inference based on conditional specification. Int Stat Rev. 1977;45:117–28.
Acknowledgements
We thank the participants and their families for taking part in this research. We would like to thank Helen Christou and Stella Kourembanas for their support and guidance throughout the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tamilia, E., Parker, M.S., Rocchi, M. et al. Nutritive sucking abnormalities and brain microstructural abnormalities in infants with established brain injury: a pilot study. J Perinatol 39, 1498–1508 (2019). https://doi.org/10.1038/s41372-019-0479-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0479-6
This article is cited by
-
Advances in Swallowing Neurophysiology Across Pediatric Development: Current Evidence and Insights
Current Physical Medicine and Rehabilitation Reports (2021)