Abstract
Objectives
The primary objective was to describe the early “natural history” of pulmonary hypertension (PH) in the premature population. The secondary objective was to describe factors associated with poor outcomes in the premature population with PH at 36 weeks post-menstrual age (PMA).
Study design
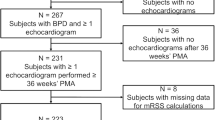
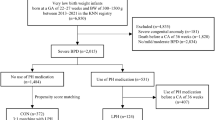
Retrospective chart review of patients followed at our institution from 2000 to 2017 with echocardiographic (ECHO) evidence of PH at 36 weeks PMA, and born ≤ 32 weeks estimated gestational age (GA). Cox regression was used for survival analysis.
Results
Sixty-one patients with PH (26.5 ± 1.5 weeks at birth) were included. All PH patients had bronchopulmonary dysplasia (BPD), with 89% considered severe; 38% were small for gestational age. Necrotizing enterocolitis requiring surgery was common (25%). Use of post-natal steroids (HR 11.02, p = 0.01) and increased severity of PH (HR 1.05, p < 0.001) were associated with mortality. Pulmonary vein stenosis (PVS) was documented in 26% of the PH cohort, but not associated with increased mortality. ECHO estimation of pulmonary artery pressure (PAP) was available in 84%. PAP was higher in those who died (sPAP/sBP ratio 1.09 ± 27 vs 0.83 ± 20 %, p = 0.0002). At follow-up (mean 250 ± 186 weeks PMA), 72% of the PH cohort was alive. Most survivors (66%) had resolution of their PH on their most recent ECHO; 31% remained on PH therapy.
Conclusion
PH resolved in most survivors in this study population. Mortality in those with BPD-PH was associated with male sex, post-natal steroid use, and increased severity of PH, but not with PVS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bhat R, Salas AA, Foster C, Carlo WA, Ambalavanan N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics. 2012;129:e682–e689.
Khemani E, McElhinney DB, Rhein L, Andrade O, Lacro RV, Thomas KC, et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics. 2007;120:1260–9.
Abman SH, Hansmann G, Archer SL, Ivy DD, Adatia I, Chung WK, et al. Pediatric pulmonary hypertension guidelines from the American Heart Association and American Thoracic Society. Circulation. 2015;132:21.
Weismann, C. G., Asnes, J. D., Bazzy-Asaad, A., et al. Pulmonary hypertension in preterm infants: results of a prospective screening program. Journal of Perinatology, 2017;37:p. 572.
Berkelhamer SK, Mestan KK, Steinhorn RH. Pulmonary hypertension in bronchopulmonary dysplasia. Semin Perinatol. 2013;37:124–31.
Altit G, Dancea A, Renaud C, Perreault T, Lands LC, Sant’Anna G. Pathophysiology, screening and diagnosis of pulmonary hypertension in infants with bronchopulmonary dysplasia-a review of the literature. Paediatr Respir Rev. 2016;23:16–26.
Farquhar M, Fitzgerald DA. Pulmonary hypertension in chronic neonatal lung disease. Paediatr Respir Rev. 2010;11:149–53.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
King M, Braun H, Goldblatt A, Liberthson R, Weyman A. Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation. 1983;68:68–75.
Kalfa D, Belli E, Bacha E, Lambert V, di Carlo D, Kostolny M, et al. Primary pulmonary vein stenosis: outcomes, risk factors, and severity score in a multicentric study. Ann Thorac Surg. 2017;104:182–9.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1.
Davignon A. ECG standards for children. Pediatr Cardiol. 1980;1:133–52.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196:147. e141–148.
Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. Intensive care for extreme prematurity—moving beyond gestational age. New Engl J Med. 2008;358:1672–81.
Matsuda A, Orihara K, Fukuda S, Fujinaga H, Matsumoto K, Saito H. Corticosteroid enhances TNF-alpha-mediated leukocyte adhesion to pulmonary microvascular endothelial cells. Allergy. 2008;63:1610–6.
Price LC, Shao D, Meng C, Perros F, Garfield BE, Zhu J, et al. Dexamethasone induces apoptosis in pulmonary arterial smooth muscle cells. Respir Res. 2015;16:114.
Wagner EM, Sanchez J, McClintock JY, Jenkins J, Moldobaeva A. Inflammation and ischemia-induced lung angiogenesis. Am J Physiol Lung Cell Mol Physiol. 2008;294:L351–357.
Neuhaus W, Schlundt M, Fehrholz M, Ehrke A, Kunzmann S, Liebner S, et al. Multiple antenatal dexamethasone treatment alters brain vessel differentiation in newborn mouse pups. PLoS ONE. 2015;10:e0136221.
Kasselman LJ, Kintner J, Sideris A, Pasnikowski E, Krellman JW, Shah S, et al. Dexamethasone treatment and ICAM-1 deficiency impair VEGF-induced angiogenesis in adult brain. J Vasc Res. 2007;44:283–91.
Niu Y, Herrera EA, Evans RD, Giussani DA. Antioxidant treatment improves neonatal survival and prevents impaired cardiac function at adulthood following neonatal glucocorticoid therapy. J Physiol. 2013;591:5083–93.
Herrera EA, Verkerk MM, Derks JB, Giussani DA. Antioxidant treatment alters peripheral vascular dysfunction induced by postnatal glucocorticoid therapy in rats. PLoS ONE. 2010;5:e9250.
de Vries WB, van der Leij FR, Bakker JM, Kamphuis PJ, van Oosterhout MF, Schipper ME, et al. Alterations in adult rat heart after neonatal dexamethasone therapy. Pediatr Res. 2002;52:900–6.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Heching HK, Turner M, Farkouh-Karoleski C, Krishnan U. Pulmonary vein stenosis and necrotising enterocolitis: is there a possible link with necrotising enterocolitis? Arch Dis Child Fetal Neonatal Ed. 2014:99:F282–5.
Mourani PM, Sontag MK, Younoszai A, Ivy DD, Abman SH. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics. 2008;121:317–25.
Stenmark KR, Abman SH. Lung vascular development: implications for the pathogenesis of bronchopulmonary dysplasia. Annu Rev Physiol. 2005;67:623–61.
Mourani PM, Abman SH. Pulmonary hypertension and vascular abnormalities in bronchopulmonary dysplasia. ClinPerinatol. 2015;42; 839–855.
Latson LA, Prieto LR. Congenital and acquired pulmonary vein stenosis. Circulation. 2007;115:103–8.
Amin R, Kwon S, Moayedi Y, Sweezey N. Pulmonary vein stenosis: case report and literature review. Can Respir J. 2009;16:e77.
Edwards J. Congenital stenosis of pulmonary veins. Pathologic and developmental considerations. Lab Investig. 1959;9:46–66.
Laux D, Rocchisani MA, Boudjemline Y, Gouton M, Bonnet D, Ovaert C. Pulmonary hypertension in the preterm infant with chronic lung disease can be caused by pulmonary vein stenosis: a must-know entity. Pediatr Cardiol. 2016;37:313–21.
Swier NL, Richards B, Cua CL, Lynch SK, Yin H, Nelin LD, et al. Pulmonary vein stenosis in neonates with severe bronchopulmonary dysplasia. Am J Perinatol 2016;33:671–7.
Mahgoub L, Kaddoura T, Kameny AR, Lopez Ortego P, Vanderlaan RD, Kakadekar A, et al. Pulmonary vein stenosis of ex‐premature infants with pulmonary hypertension and bronchopulmonary dysplasia, epidemiology, and survival from a multicenter cohort. Pediatr Pulmonol. 2017;52:1063–70.
Swier NL, Richards B, Cua CL, Lynch SK, Yin H, Nelin LD, et al. Pulmonary vein stenosis in neonates with severe bronchopulmonary dysplasia. Am J Perinatol. 2016;33:671–7.
Acknowledgements
We acknowledge Dr. Gautier Gabriel Marcq, MD, MSc, for his review of the statistical analysis.
Author information
Authors and Affiliations
Contributions
Gabriel Altit designed the protocol, worked on the data collection and analysis, and prepared the manuscript. Shazia Bhombal and Theresa Tacy helped in the design of the study and on the preparation of the manuscript. Rachel Hopper helped in the interpretation of data and on preparation of manuscript. Jeffrey Feinstein overviewed the whole process from design of the study to preparation of final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to the content of this study. Gabriel Altit is the author that wrote the first draft. This study was approved by the institutional review board of Stanford University (protocol - IRB-39388). The study was supported by the Vera Moulton Wall Center for Pulmonary Vascular Disease at Stanford.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Altit, G., Bhombal, S., Hopper, R.K. et al. Death or resolution: the “natural history” of pulmonary hypertension in bronchopulmonary dysplasia. J Perinatol 39, 415–425 (2019). https://doi.org/10.1038/s41372-018-0303-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0303-8
This article is cited by
-
Association of the respiratory severity score with bronchopulmonary dysplasia-associated pulmonary hypertension in infants born extremely preterm
Journal of Perinatology (2024)
-
Assessing the role of tracheostomy placement in bronchopulmonary dysplasia with pulmonary hypertension
Journal of Perinatology (2024)
-
Extremely premature infants born at 23–25 weeks gestation are at substantial risk for pulmonary hypertension
Journal of Perinatology (2022)
-
Bench to bedside — new insights into the pathogenesis of necrotizing enterocolitis
Nature Reviews Gastroenterology & Hepatology (2022)
-
Screening Echocardiography Identifies Risk Factors for Pulmonary Hypertension at Discharge in Premature Infants with Bronchopulmonary Dysplasia
Pediatric Cardiology (2022)