Abstract
Objective:
To evaluate the association between hypercarbia in the first 24 h of life and clinical outcomes in infants with congenital diaphragmatic hernia (CDH).
Study design:
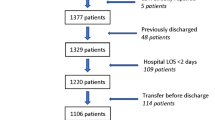
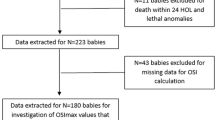
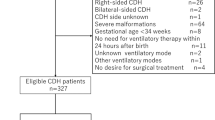
Retrospective review of patients entered into the CDHSG registry between 2007–2014. Half of the identified patients were analyzed to identify the PaCO2 value most predictive of mortality. Prediction models for outcomes of death, ECMO, and respiratory support at 30 days of life (DOL) were developed using PaCO2. Remaining half of data was used for validation of study findings.
Results:
1878 and 1875 patients were analyzed in the testing and validation groups. Lowest PaCO2≥60 mmHg in the first DOL is highly predictive of death prior to discharge. Prediction models including this variable demonstrate good discrimination for outcomes of death, ECMO, and respiratory support (AUC 0.8808, 0.8279, 0.8065).
Conclusion:
Lowest PaCO2 in the first DOL is an independent risk factor of mortality and morbidity in CDH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Schultz CM, DiGeronimo RJ, Yoder BA. Congenital diaphragmatic hernia: a simplified postnatal predictor of outcome. J Pediatr Surg. 2007;42:510–6.
Haricharan RN, Barnhart DC, Cheng H, Delzell E. Identifying neonates at a very high risk for mortality among children with congenital diaphragmatic hernia managed with extracorporeal membrane oxygenation. J Pediatr Surg. 2009;44:97–93.
Coleman AJ, Brozanski B, Mahmood B, Wearden PD, Potoka D, Kuch BA. First 24-h SNAP-II score and highest PaCO2 predict the need for ECMO in congenital diaphragmatic hernia. J Pediatr Surg. 2013;48:2214–8.
Park HW, Lee BS, Lim G, Choi Y, Kim EA, Kim K. A simplified formula using early blood gas analysis can predict survival outcomes and the requirements for extracorporeal membrane oxygenation in congenital diaphragmatic hernia. J Korean Med Sci. 2013;28:924–8.
Brindle ME, Cook EF, Tibboel D, Lally PA, Lally KP, Congenital Diaphragmatic Hernia Study Group. A Clinical prediction rule for the severity of congenital diaphragmatic hernias in newborns. Pediatrics. 2014;134:e413–9.
Terui K, Nagata K, Kanamori Y, Takahashi S, Hayakawa M, Okuyama H, et al. Risk stratification for congenital diaphragmatic hernia by factors within 24h after birth. J Perinatol. 2017;37:805–8.
Bohn DJ, James I, Filler RM, Ein SH, Wesson DE, Shandling B, et al. The relationship between PaCO2 and ventilation parameters in predicting survival in congenital diaphragmatic hernia. J Pediatr Surg. 1984;19:666–71.
Germain JF, Farnoux C, Pinquier D, Cortez A, Hartmann JF, Sibony O, et al. Can blood gas values predict pulmonary hypoplasia in antenatally diagnosed congenital diaphragmatic hernia? J Pediatr Surg. 1996;31:1634–9.
Salas AA, Bhat R, Dabrowska K, Leadford A, Anderson S, Harmon CM, et al. The value of PaCO2 in relation to outcome in congenital diaphragmatic hernia. Am J Perinatol. 2014;31:939–46.
Khmour AY, Konduri GG, Sato TT, Uhing MR, Basir MA. Role of admission gas exchange measurement in predicting congenital diaphragmatic hernia survival in the era of gentle ventilation. J Pediatr Surg. 2014;49:1197–201.
Abbas PI, Cass DI, Olutoye OO, Zamora IJ, Akinkuotu AC, Sheik F, et al. Persistent hypercarbia after resuscitation is associated with increased mortality in congenital diaphragmatic hernia patients. J Pediatr Surg. 2015;50:739–43.
Kays DW, Islam S, Perkins JM, Larson SD, Taylor JA, Talbert JL. Outcomes in the physiologically most severe congenital diaphragmatic hernia (CDH) patients: Whom should we treat? J Pediatr Surg. 2015;50:893–7.
Grizelj R, Bojanic K, Pritisanac E, Luetic T, Vukovic J, Weingarten TN, et al. Survival prediction of high-risk outborn neonates with congenital diaphragmatic hernia from capillary blood gases. BMC Pediatr 2016; 16.
Bagolan P, Morini F. Long-term follow up in infants with congenital diaphragmatic hernia. Semin Pediatr Surg. 2007;16:134–44.
Cauley RP, Potanos K, Fullington N, Bairdain S, Sheils CA, Finkelstein JA, et al. Pulmonary support on day of life 30 is a strong predictor of increased 1 and 5-year morbidity in survivors of congenital diaphragmatic hernia. J Pediatr Surg. 2015;50:849–55.
Bruns AS, Lau PE, Dhillon GS, Hagan J, Kailin JA, Mallory GB, et al. Predictive value of oxygenation index for outcome in left-sided congenital diaphragmatic hernia. J Pediatr Surg. 2018;53:1675–80.
Author information
Authors and Affiliations
Consortia
Contributions
Minal Patel conceptualized the study, performed some statistical analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Cynthia Bell developed a detailed statistical plan, performed expert statistical analysis, provided guidance with data interpretation, and revised the manuscript. Kevin Lally provided oversight on study design and critically reviewed the manuscript. Pamela Lally coordinated and supervised data collection in the Congenital Diaphragmatic Hernia Study Group database, provided data output for the study, and critically reviewed the manuscript. Lakshmi Katakam conceptualized the study, provided oversight on study design, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Patel, M.J., Bell, C.S., Lally, K.P. et al. Lowest PaCO2 on the first day of life predicts mortality and morbidity among infants with congenital diaphragmatic hernia. J Perinatol 39, 229–236 (2019). https://doi.org/10.1038/s41372-018-0269-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0269-6
This article is cited by
-
Congenital diaphragmatic hernia
Nature Reviews Disease Primers (2022)