Abstract
Objective:
Decrease time to enteral feeding initiation and advancement.
Study Design:
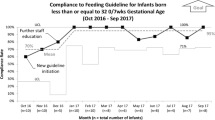
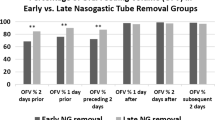
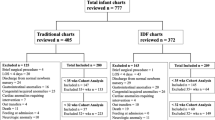
In our all-referral neonatal intensive care unit, we developed an evidence-based guideline addressing feeding initiation and advancement. During 6 months before and 7 months after guideline implementation, we measured time to initiate feeding, time to 100 ml/kg/day of feeding, gastric residual measurement frequency, and incidence of necrotizing enterocolitis (balancing measure).
Result:
Two hundred twenty-three infants were studied. Time from admission to feeding initiation was shorter after guideline implementation (mean 0.5 days [95% CI: 0.4–0.7] vs. 1.1 days [95% CI: 0.7–1.5], p = 0.01). Time from admission to 100 ml/kg/day feeding was also shorter (3.6 days [95% CI: 2.8–4.4] vs. 6.2 days [95% CI: 4.4–8.1], p = 0.01). After guideline implementation, routine gastric residual measurements were discontinued.
Conclusion:
After implementation of an enteral feeding guideline, which included discontinuation of routine gastric residual assessment, we observed a faster initiation of enteral feeding and shorter time to reach 100 ml/kg/day.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Belfort MB, Ehrenkranz RA. Neurodevelopmental outcomes and nutritional strategies in very low birth weight infants. Semin Fetal Neonatal Med. 2017;22:42–8.
Senterre T. Practice of enteral nutrition in very low birth weight and extremely low birth weight infants. In: World review of nutrition and dietetics; B. Koletzko, B. Poindexter, and R Uauy. Karger: Basel, Switzerland, 2014. p. 201–14.
Maas C, Poets CF, Franz AR. Avoiding postnatal undernutrition of VLBW infants during neonatal intensive care: evidence and personal view in the absence of evidence. Arch Dis Child Fetal Neonatal Ed. 2015;100:F76–81.
Embleton ND, Morgan C, King C. Balancing the risks and benefits of parenteral nutrition for preterm infants: can we define the optimal composition? Arch Dis Child Fetal Neonatal Ed. 2014;100:72–6.
Bevan A, Johnson M, Pond J, Lansdowne Z, Leaf A, Hayes P, et al. Reformulation of standardised neonatal parenteral nutrition to improve nutrient delivery. Arch Dis Child. 2013;98:e1–e1.
Rangel SJ, Calkins CM, Cowles RA, Barnhart DC, Huang EY, Abdullah F, et al. Parenteral nutrition-associated cholestasis: an American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J Pediatr Surg. 2012;47:225–40.
Piazza AJ, Brozanski B, Provost L, Grover TR, Chuo J, Smith JR, et al. SLUG Bug: quality improvement with orchestrated testing leads to NICU CLABSI reduction. Pediatrics. 2016;137:e20143642.
Konnikova Y, Zaman MM, Makda M, D’Onofrio D, Freedman SD, Martin CR. Late enteral feedings are associated with intestinal inflammation and adverse neonatal outcomes. PLoS ONE. 2015;10:e0132924.
Dutta S, Singh B, Chessell L, Wilson J, Janes M, McDonald K, et al. Guidelines for feeding very low birth weight infants. Nutrients. 2015;7:423–42.
Stefanescu BM, Gillam-Krakauer M, Stefanescu AR, Markham M, Kosinski JL. Very low birth weight infant care: adherence to a new nutrition protocol improves growth outcomes and reduces infectious risk. Early Hum Dev. 2016;94:25–30.
Patole SK, de Klerk N. Impact of standardised feeding regimens on incidence of neonatal necrotising enterocolitis: a systematic review and meta-analysis of observational studies. Arch Dis Child Fetal Neonatal Ed. 2005;90:F147–51.
Jasani B, Patole S. Standardized feeding regimen for reducing necrotizing enterocolitis in preterm infants: an updated systematic review. J Perinatol. 2017;37:827–833.
van Goudoever JB, Turck D. Term and preterm infants. In: World review of nutrition and dietetics; B. Koletzko B, R. Shamir, and D. Turck. Karger: Basel, Switzerland, 2016. p. 50–65.
Goswami I, Rochow N, Fusch G, Liu K, Marrin M, Heckmann M, et al. Length normalized indices for fat mass and fat-free mass in preterm and term infants during the first six months of life. Nutrients. 2016;8:417.
Institute for Healthcare Improvement. The breakthrough series: IHI’s Collaborative Model for achieving breakthrough improvement (IHI Innovation Series white paper). Boston: Institute for Healthcare Improvement; 2003.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Kliegman RM, Walsh MC. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr. 1987;17:213–88.
Buttrey SE. An excel add-in for statistical process control charts. J Stat Softw. 2009;30:1–12.
Morgan J, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Systematic Rev. 2015:CD001241.
Patel AL, Trivedi S, Bhandari NP, Ruf A, Scala CM, Witowitch G, et al. Reducing necrotizing enterocolitis in very low birth weight infants using quality-improvement methods. J Perinatol. 2014;34:850–7.
Patole SK, Kadalraja R, Tuladhar R, Almonte R, Muller R, Whitehall JS. Benefits of a standardised feeding regimen during a clinical trial in preterm neonates. Int J Clin Pract. 2000;54:429–31.
Torrazza RM, Parker LA, Li Y, Talaga E, Shuster J, Neu J. The value of routine evaluation of gastric residuals in very low birth weight infants. J Perinatol. 2015;35:57–60.
Giesinger RE, McNamara PJ. Hemodynamic instability in the critically ill neonate: An approach to cardiovascular support based on disease pathophysiology. Semin Perinatol. 2016;40:1–15.
Malhotra AK, Deorari AK, Paul VK, Bagga A, Singh M. Gastric residuals in preterm babies. J Trop Pediatr. 1992;38:262–4.
Kuzma-O’Reilly B, Duenas ML, Greecher C, Kimberlin L, Mujsce D, Miller D, et al. Evaluation, development, and implementation of potentially better practices in neonatal intensive care nutrition. Pediatrics. 2003;111(4 Pt 2):e461–70.
Bertino E, Giuliani F, Prandi G, Coscia A, Martano C, Fabris C. Necrotizing enterocolitis: risk factor analysis and role of gastric residuals in very low birth weight infants. J Pediatr Gastroenterol Nutr. 2009;48:437–42.
Mihatsch WA, von Schoenaich P, Fahnenstich H, Dehne N, Ebbecke H, Plath C, et al. The significance of gastric residuals in the early enteral feeding advancement of extremely low birth weight infants. Pediatrics. 2002;109:457–9.
Li Y-F, Lin H-C, Torrazza RM, Parker L, Talaga E, Neu J. Gastric residual evaluation in preterm neonates: a useful monitoring technique or a hindrance? Pediatr Neonatol. 2014;55:335–40.
Shulman RJ, Ou C-N, Smith EO. Evaluation of potential factors predicting attainment of full gavage feedings in preterm infants. Neonatology. 2011;99:38–44.
Battersby C, Longford N, Mandalia S, Costeloe K, Modi N, UK Neonatal Collaborative Necrotising Enterocolitis (UKNC-NEC) study group. Incidence and enteral feed antecedents of severe neonatal necrotising enterocolitis across neonatal networks in England, 2012–13: a whole-population surveillance study. Lancet Gastroenterol Hepatol. 2017;2:43–51.
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. Standards for QUality Improvement Reporting Excellence 2.0: revised publication guidelines from a detailed consensus process. J Surg Res. 2016;200:676–82.
Acknowledgements
We thank all the patients, families, and care providers who participated in the study. We thank Munish Gupta MD, MMSc for providing guidance regarding project design. We used the SQUIRE 2.0 guideline to write this manuscript (31).
Funding:
Funding provided by the Program for Patient Quality and Safety at Boston Children’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Morton, S.U., Belfort, M.B., Kahlon, P.S. et al. Reducing time to initiation and advancement of enteral feeding in an all-referral neonatal intensive care unit. J Perinatol 38, 936–943 (2018). https://doi.org/10.1038/s41372-018-0110-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0110-2
This article is cited by
-
Very low birth weight infants receive full enteral nutrition within 2 postnatal weeks
Journal of Perinatology (2020)