Abstract
Objectives
To improve Neonatal Abstinence Syndrome (NAS) inpatient outcomes through a comprehensive quality improvement (QI) program.
Design
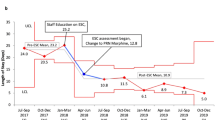
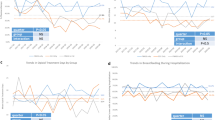
Inclusion criteria were opioid-exposed infants ≥36 weeks. QI methodology including stakeholder interviews and plan-do-study-act (PDSA) cycles were utilized. We compared pre- and post-intervention NAS outcomes after a QI initiative that included: A non-pharmacologic care bundle, function-based assessments consisting of symptom prioritization and then the “Eat, Sleep, Console” (ESC) Tool; and a switch to methadone for pharmacologic treatment.
Results
Pharmacologic treatment decreased from 87.1 to 40.0%; adjunctive agent use from 33.6 to 2.4%; hospitalization length from a mean 17.4 to 11.3 days, and opioid treatment days from 16.2 to 12.7 (p < 0.001 for all). Total hospital charges decreased from $31,825 to $20,668 per infant. Parental presence increased from 55.6 to 75.8% (p < 0.0001). No adverse events were noted.
Conclusions
A comprehensive QI program focused on non-pharmacologic care, function-based assessments, and methadone resulted in significant sustained improvements in NAS outcomes. These findings have important implications for establishing potentially better practices for opioid-exposed newborns.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated healthcare expenditures—United States, 2000−2009. JAMA. 2012;307:1934–40.
Patrick SW, Davis MM, Lehman CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35:667.
Milliren CE, Gupta M, Graham DA, Melvin P, Jorina M, Ozonoff A. Hospital variation in neonatal abstinence syndrome incidence, treatment modalities, resource use, and costs across pediatric hospitals in the United States, 2013 to 2016. Hosp Pediatr. 2018;8:15–20.
Massachusetts Department of Public Health. 2017. Data brief: an assessment of opioid-related overdoses in Massachusetts 2011−2015 [Homepage on the Internet]. http://www.mass.gov/eohhs/docs/dph/stop-addiction/data-brief-chapter-55-aug-2017.pdf (Accessed August 2017).
Hudak ML, Tan RC. From the American Academy of Pediatrics: Neonatal drug withdrawal. Pediatrics. 2012;129:e540–560.
Kraft WK, Adeniyi-Jones SC, Chervoneva I, Greenspan JS, Abatemarco D, Kaltenbach K, et al. Buprenorphine for the treatment of the neonatal abstinence syndrome. N Engl J Med. 2017;376:2341–8.
Brown MS, Hayes MJ, Thornton LM. Methadone versus morphine for treatment of neonatal abstinence syndrome: a prospective randomized clinical trial. J Perinatol. 2015;35:278–83.
Tolia VN, Patrick SW, Bennett MM, Murthy K, Sousa J, Smith PB, et al. Increasing incidence of the neonatal abstinence syndrome in U.S. neonatal ICUs. N Engl J Med. 2015;372:2118–26.
Sarkar S, Donn SM. Management of neonatal abstinence syndrome in neonatal intensive care units: a national survey. J Perinatol. 2006;26:15–17.
Mehta A, Forbes KD, Kuppala VS. Neonatal abstinence syndrome management from prenatal counseling to post-discharge follow-up care: results of a national survey. Hosp Pediatr. 2013;3:317–23.
Bogen DL, Whalen BL, Kair LR, Vining M, King BA. Wide variation found in care of opioid-exposed newborns. Acad Pediatr. 2017;17:374–80.
Finnegan LP, Connaughton JF Jr, Kron RE, Emich JP. Neonatal abstinence syndrome: assessment and management. Addict Dis. 1975;2:141–58.
Jones HE, Seashore C, Johnson E, Horton E, O’Grady KE, Andringa K, et al. Psychometric assessment of the Neonatal Abstinence Scoring System and the MOTHER NAS Scale. Am J Addict. 2016;25:370–3.
Grossman M, Berkwitt A, Osborn R, Xu Y, Esserman DA, Shapiro ED. et al. An initiative to improve the quality of care of infants with neonatal abstinence syndrome. Pediatrics. 2017;139:e20163360
Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr. 2018;8:1–6.
Holmes AV, Atwood EC, Whalen B, Beliveau J, Jarvis JD, Matulis J. et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics. 2016;137:e20152929
Bagley SM, Wachman EM, Holland E, Brogly SB. Review of the assessment and management of neonatal abstinence syndrome. Addict Sci Clin Pract. 2014;9:19.
Howard MB, Schiff MD, Penwill N, Si W, Rai A, Wolfgang T, et al. Impact of parental presence at infants’ bedside on neonatal abstinence syndrome. Hosp Pediatr. 2017;7:63–69.
MacMillan KD, Rendon CP, Verma K, Riblet N, Washer DB, Holmes AV. Rooming-in for neonatal abstinence syndrome: a systematic review and meta-analysis. JAMA Pediatrics. Feb. 5. https://doi.org/10.1001/jamapediatrics.2017.5195 [Epub ahead of print].
Neo Advances [homepage on the Internet]. Karen D’Apilito. Available from: https://www.neoadvances.com/index.html.
Clinical Trials.Gov: improving outcomes in neonatal abstinence syndrome [homepage on the Internet]. First posted October 2013, updated December 2017. Available from: https://clinicaltrials.gov/ct2/show/NCT01958476.
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290–8.
Wachman EM, Newby PK, Vreeland J, Byun J, Bonzagni A, Bauchner H, et al. The relationship between maternal opioid agonists and psychiatric medications on length of hospitalization for neonatal abstinence syndrome. J Addict Med. 2011;5:293–9.
Jones HE, Heil SH, Tuten M, Chisolm MS, Foster JM, O’Grady KE, et al. Cigarette smoking in opioiddependent pregnant women: neonatal and maternal outcomes. Drug Alcohol Depend. 2013;131:271–7.
Patrick SW, Dudley J, Martin PR, Harrell FE, Warren MD, Hartmann KE, et al. Prescription opioid epidemic and infant outcomes. Pediatrics. 2015;135:842–50.
Hall ES, Meinzen-Derr J, Wexelblatt SL. Cohort analysis of a pharmacokinetic-modeled methadone weaning optimization for neonatal abstinence syndrome. J Pediatr. 2015;167:1221–5.e1.
Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. BMJ Qual Saf. 2003;12:458–64.
Saia K, Bagley SM, Wachman EM, Patel PP, Nadas MD, Brogly SB. Prenatal treatment for opioid dependency: observations from a large inner-city clinic. Addict Sci Clin Pract. 2017;12:5.
Acknowledgements
This study was funded by the Massachusetts Health Policy Commission and the Boston Medical Center Department of Pediatrics. We would like to acknowledge Kathryn MacMillan, Victoria Flanagan, William Edwards, Sheila-Jane Lewis, Rachel Hoch, Rishitha Bollam, Nicole Desai, Kate Mitchell, Nicole Penwill, Rachel Morgan, Cathleen Dehn, Kristine Smith, Jordana Price, Michelle Sia, Tirah Samura, the entire Project RESPECT team, all pediatric nurses from the BMC inpatient units, Mary Beth Howard, Macy Reed, CALM volunteers, Zoe Thomas, Leonie Hoyo, Maria D’Amico, Nina Gummadi, and Cassie Duran.
Funding
Massachusetts Health Policy Commission Neonatal Abstinence Syndrome Innovation Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wachman, E.M., Grossman, M., Schiff, D.M. et al. Quality improvement initiative to improve inpatient outcomes for Neonatal Abstinence Syndrome. J Perinatol 38, 1114–1122 (2018). https://doi.org/10.1038/s41372-018-0109-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0109-8
This article is cited by
-
Evaluating a web-based training curriculum for disseminating best practices for the care of newborns with neonatal opioid withdrawal syndrome in a rural hospital, the NOWS-NM Program
BMC Pediatrics (2024)
-
The Alberta Neonatal Abstinence Syndrome Mother-Baby Care ImprovEmeNT (NASCENT) program: protocol for a stepped wedge cluster randomized trial of a hospital-level Neonatal Abstinence Syndrome rooming-in intervention
BMC Health Services Research (2023)
-
Addressing drivers of healthcare utilization for neonatal opioid withdrawal syndrome
Journal of Perinatology (2023)
-
RETRACTED ARTICLE: The Neonatal Withdrawal Assessment Tool (NWAT): pilot inter-rater reliability and content validity
Journal of Perinatology (2023)
-
Drivers of decision-making regarding infant sleep practices among mothers with opioid use disorder
Journal of Perinatology (2023)