Abstract
Background
Acute bilirubin encephalopathy (ABE) is an important cause of neonatal morbidity in Nigeria, accounting for 5–14% of neonatal deaths. Most newborns with severe ABE have irreversible damage before receiving treatment emphasizing the need for timely pre-admission monitoring and referral. There is limited evidence that educational interventions targeting mothers and health care providers will reduce delayed care.
Objective
To provide baseline data on the incidence of ABE and associated pre-admission risk factors in five centers of Nigeria in order to evaluate the effect of subsequent educational interventions on outcome.
Study design
The incidence of ABE among newborns treated for hyperbilirubinemia was documented prospectively. Bivariate analysis and multivariate logistic regression were used to evaluate risk factors for acute bilirubin encephalopathy and reasons for regional differences in its occurrence.
Results
Of 1040 infants, 159 treated for hyperbilirubinemia (15.3%) had mild to severe bilirubin encephalopathy (including 35 deaths), but the incidence ranged from 7 to 22% between centers. Logistic regression identified four common predictors: total serum bilirubin (odds ratio 1.007 per mg/dl rise), out-of-hospital births (OR 2.6), non-alloimmune hemolytic anemia (OR 2.8), and delayed care seeking (OR 4.3).
Conclusion
The high occurrence of bilirubin encephalopathy in Nigeria is due in large part to a delay in seeking care. A planned intervention strategy will target conditions leading to severe hyperbilirubinemia and delay.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Adebami OJ. Factors associated with the incidence of acute bilirubin encephalopathy in Nigerian population. J Pediatr Neurol. 2011;9(20):347–53.
Ogunlesi TA, Dedeke IO, Adekanmbi AF, Fetuga MB, Ogunfowora OB. The incidence and outcome of bilirubin encephalopathy in Nigeria: a bi-centre study. Niger J Med. 2007;16(4):354–9.
Owa JA, Taiwo O, Adebiyi JAO, Dogunro SA. Neonatal Jaundice at Wesley Guild Hospital. Ilesa and Ife State Hospital, Ile-Ife. Niger J Paediatr. 1989;16:23–30.
Owa JA, Osinaike AI. Neonatal morbidity and mortality in Nigeria. Indian J Pediatr. 1998;65(3):441–9.
Okechukwu A, Achonwa A. Morbidity and mortality patterns of admissions into the special care baby unit of University of Abuja Teaching Hospital. Niger J Clin Pract. 2009;4(12):389–94.
Udo JJ, Anah MU, Ochigbo SO, Etuk IS, Ekanem AD. Neonatal morbidity and mortality in Calabar, Nigeria: a hospital-based study. Niger J Clin Pract. 2008;11(3):285–9.
Ugwu R, Eneh A, Oruamabo R. Mortality in the special care baby unit of the University of Port Harcourt Teaching Hospital (UPTH). Why and when do newborns die? Nig J Paediatr. 2006;3(33):133–4.
Iskander I, Gamaleldin R, El Houchi S, El Shenawy A, Seoud I, El Gharbawi N, et al. Serum bilirubin and bilirubin/albumin ratio as predictors of bilirubin encephalopathy. Pediatrics . 2014;134(5):e1330–e1339.
Saluja S, Agarwal A, Kler N, Amin S. Auditory neuropathy spectrum disorder in late preterm and term infants with severe jaundice. Int J Pediatr Otorhinolaryngol. 2010;74(11):1292–7.
Olusanya BO, Akande AA, Emokpae A, Olowe SA. Infants with severe neonatal jaundice in Lagos, Nigeria: incidence, correlates and hearing screening outcomes. Trop Med Int Health. 2009;14:301–10.
Belonwu RO, Gwarzo GD, Adeleke SI. Cerebral palsy in Kano, Nigeria-a review. Niger J Med. 2009;18:186–9.
Ayanniyi O, Abdulsalam KS. Profile of children with cerebral palsy attending out-patient physiotherapy clinics in Southwest Nigeria. AJPARS. 2015;7:32–39.
Okperi BO. Neonatal jaundice and birth asphyxia as major causes of cerebral palsy in Nigeria: are doctors’ wrong beliefs and practices part of the problem? Int J Med Biomed Res. 2013;2:226–30.
Olusanya BO, Ogunlesi TA, Slusher TM. Why is kernicterus still a major cause of death and disability in low and middle-income countries? Arch Dis Child. 2014;99(12):1117–21.
Owa JA, Ogunlesi TA. Why we are still doing so many exchange blood transfusion for neonatal jaundice in Nigeria. World J Pediatr. 2009;5(1):51–55.
Ogunlesi TA, Ogunfowora OB. Predictors of acute bilirubin encephalopathy among Nigerian term babies with moderate-to-severe hyperbilirubinaemia. J Trop Pediatr. 2011;57(2):80–86.
Ogunlesi TA, Abdul AR. Maternal knowledge and care-seeking behaviors for newborn jaundice in Sagamu, Southwest Nigeria. Niger J Clin Pract. 2015;18(1):33–40.
Ogunlesi T, Ogunlesi F. Family socio-demographic factors and maternal obstetric factors influencing appropriate health-care seeking behaviours for newborn jaundice in Sagamu, Nigeria. Matern Child Health J. 2012;16(3):677–84.
Goodman OOK, Odugbemi BA, Femi-Adebayo TT, Odusanya OO. Neonatal jaundice: knowledge, attitude and practices of mothers in Mosan-Okunola community, Lagos, Nigeria. Niger Postgrad Med J. 2015;22(3):158–63.
Egube BA, Ofili AN, Isara AR, Onakewhor JU. Neonatal jaundice and its management: knowledge, attitude, and practice among expectant mothers attending antenatal clinic at University of Benin Teaching Hospital, Benin City, Nigeria. Niger J Clin Pract. 2013;16(2):188–94.
Eneh AU, Ugwu RO. Perception of neonatal jaundice among women attending children out patient and immunization clinics of the UPTH Port Harcourt. Niger J Clin Pract. 2009;12(2):187–91.
Ezeaka CV, Ugwu RO, Mukhtar-Yola M, Ekure EN, Olusanya BO. Pattern and predictors of maternal care-seeking practices for severe neonatal jaundice in Nigeria: a multi-centre survey. BMC Health Serv Res. 2014;14(1):192–192.
Johnson L, Bhutani VK, Karp K, Sivieri EM, Shapiro SM. Clinical report from the pilot USA Kernicterus Registry (1992 to 2004). J Perinatol. 2009;29:S25–45. Suppl 1
El Houchi SZ, Iskander I, Gamaleldin R, El Shenawy A, Seoud I, Abou-Youssef H, et al. Prediction of 3- to 5-month outcomes from signs of acute bilirubin toxicity in newborn infants. J Pediatr. 2017;183:51–55. e1
Radmacher PG, Groves FD, Owa JA, Ofovwe GE, Amuabunos EA, Olusanya BO, et al. A modified Bilirubin-induced neurologic dysfunction (BIND-M) algorithm is useful in evaluating severity of jaundice in a resource-limited setting. BMC Pediatr. 2015;15:28.
Shapiro SM. Definition of the clinical spectrum of kernicterus and bilirubin-induced neurologic dysfunction (BIND). J Perinatol. 2005;25(1):54–59.
Watchko JF, Oski FA. Bilirubin 20 mg/dL = vigintiphobia. Pediatrics. 1983;71(4):660–3.
Kuzniewicz MW, Wickremasinghe AC, Wu YW, McCulloch CE, Walsh EM, Wi S, et al. Incidence, etiology, and outcomes of hazardous hyperbilirubinemia in newborns. Pediatrics. 2014;134(3):504–9.
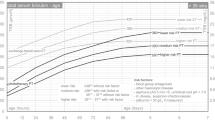
Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near term newborns. Pediatrics. 1999;103(1):6–14.
Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33:1.
Hoerl AE, Kennard RW. Ridge regresssion: biased estimation for nonorthogonal problems. Technometrics. 1970;12:55–67.
Tibshirani R. Regression shrinkage and selection via the lasso. J Royal Stat. Soc. Series B Methodol. 1996;58(1):267–88.
Wennberg RP, Ahlfors CE, Bhutani VK, Johnson LH, Shapiro SM. Toward understanding kernicterus: a challenge to improve the management of jaundiced newborns. Pediatrics. 2006;117(2):474–85.
Olusanya BO, Iskander IF, Slusher TM, Wennberg RP. A decision-making tool for exchange transfusions in infants with severe hyperbilirubinemia in resource-limited settings. J Perinatol. 2016;36(5):338–41.
Slusher TM, Vreman HJ, McLaren DW, Lewison LJ, Brown AK, Stevenson DK. Glucose-6-phosphate dehydrogenase deficiency and carboxyhemoglobin concentrations associated with bilirubin-related morbidity and death in Nigerian infants. J Pediatr. 1995;126(1):102–8.
Williams O, Gbadero D, Edowhorhu G, Brearley A, Slusher T, Lund TC. Glucose-6-phosphate dehydrogenase deficiency in Nigerian children. PLoS One. 2013;8(7):e68800.
Olusanya BO, Emokpae AA, Zamora TG, Slusher TM. Addressing the burden of neonatal hyperbilirubinaemia in countries with significant glucose-6-phosphate dehydrogenase deficiency. Acta Paediatr. 2014;103(11):1102–9.
Owa JA. Relationship between exposure to icterogenic agents, glucose-6-phosphate dehydrogenase deficiency and neonatal jaundice in Nigeria. Acta Paediatr Scand. 1989;78(6):848–52.
Sodeinde O, Chan MC, Maxwell SM, Familusi JB, Hendrickse RG. Neonatal jaundice, aflatoxins and naphthols: report of a study in Ibadan, Nigeria. Ann Trop Paediatr. 1995;15(2):107–13.
Israel-Aina YT, Omoigberale AI. Risk factors for neonatal jaundice in babies presenting at the University of Benin Teaching Hospital Benin City. Niger J Paediatr. 2012;39:159–63.
WHO Working Group. Glucose-6-phosphate dehydrogenase deficiency. Bull World Health Organ. 1989;67:601–11.
Kaplan M, Hammerman C, Bhutani VK. Parental education and the WHO neonatal G-6-PD screening program: a quarter century later. J Perinatol. 2015;35:779–84.
Ogunfowora OB, Daniel OJ. Neonatal jaundice and its management: knowledge, attitude and practice of community health workers in Nigeria. BMC Public Health. 2006;6:19.
Moawad EM, Abdallah EA, Ali YZ. Perceptions, practices, and traditional beliefs related to neonatal jaundice among Egyptian mothers: A cross-sectional descriptive study. Med (Baltim). 2016;95(36):e4804.
National Population Commission (NPC) [Nigeria] and ICF International. Nigeria Demographic and Health Survey 2013. NPC and ICF International. NPC and ICF International Abuja, Nigeria, and Rockville, Maryland, USA: 2014.
Federal Ministry of Health. Saving newborn lives in Nigeria: Newborn health in the context of the Integrated Maternal, Newborn and Child Helath Strategy. 2nd ed. Abuja: Federal Ministry of Health, Save the Children; 2011.
Olusanya BO, Osibanjo FB, Mabogunje CA, Slusher TM, Olowe SA. The burden and management of neonatal jaundice in Nigeria: A scoping review of the literature. Niger J Clin Pract. 2016;19(1):1–17.
World Health Organisation. Pocket book of hospital care for children. Guidelines for the management of common childhood illnesses. 2nd edn. Geneva, Switzerland: WHO; 2013.
Coda Zabetta CD, Iskander IF, Greco C, Bellarosa C, Demarini S, Tiribelli C, et al. Bilistick: a low-cost point-of-care system to measure total plasma bilirubin. Neonatology. 2013;103:177–81.
Acknowledgements
This study was made possible in part through the generous support of the Saving Lives at Birth partners: the United States Agency for International Development (USAID), the Government of Norway, the Bill & Melinda Gates Foundation, Grand Challenges Canada, and the UK Government. It was prepared by the “Stop Kernicterus in Nigeria” consortium and Bilimetrix, srl and does not necessarily reflect the views of the Saving Lives at Birth partners.”
Author contributions
The study results from the concerted contributions of the entire “Stop Kernicterus in Nigeria” (SKIN) team who also reviewed and approved the manuscript. Trieste (ITA): C Greco, C Tiribelli; Asaba (NGA): A Okolo, OU Chima; Lagos (NGA): Z Imam,; A Odunsi, S Olaifa; Jos(NGA): F Bode-Thomas, C Isichei, CS Yilgwan, Z Hassan, D Shwe, AO Ofakunrin, H Abdu, E Olagbaju, VC Pam, JO Abba, SN Attah; Zaria(NGA): WN Ogala, LHassan, F Abdullahi, S Purdue; Kano(NGA): BW Jibir, IY Mohammed, HA Usman, M Abdusalam, SU Abdullahi, F Usman, A Kuliya-Gwarzo, FI Tsiga-Ahmad, L Umar.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
41372_2018_94_MOESM3_ESM.docx
Supplement Figure 1. Receiver-Operator-Characteristic (ROC) curve measuring the power of the Multiple Logistic Regression model for predicting ABE(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Diala, U.M., Wennberg, R.P., Abdulkadir, I. et al. Patterns of acute bilirubin encephalopathy in Nigeria: a multicenter pre-intervention study. J Perinatol 38, 873–880 (2018). https://doi.org/10.1038/s41372-018-0094-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0094-y
This article is cited by
-
Modified Kramer’s versus Kramer’s Method for Clinical Assessment of Jaundice in Term and Near-Term Neonates
Indian Journal of Pediatrics (2024)
-
Antenatal jaundice instruction and acute bilirubin encephalopathy in Nigeria
Pediatric Research (2023)
-
Detecting acute bilirubin encephalopathy in neonates based on multimodal MRI with deep learning
Pediatric Research (2022)
-
High levels of unbound bilirubin are associated with acute bilirubin encephalopathy in post-exchange transfusion neonates
Italian Journal of Pediatrics (2021)
-
Commentary on the Don Ostrow Trieste Yellow Retreat 2019: a successful biennium, what next?
Pediatric Research (2020)