Abstract
Whole-day movement guidelines for improving health, recommend that adults engage in at least 150 min week−1 of moderate-to-vigorous aerobic physical activity and limit their sedentary time. In young adults, higher systolic blood pressure variability (BPV) is a precursor for the development of hypertension. The impact of habitual activity that comprises (inter)national guidelines on BPV is unclear. We tested the hypothesis that less habitual physical activity and greater sedentary time would be associated with larger BPV. Ninety-two normotensive participants [age: 19–38 years, body mass index (BMI): 23.6 ± 3.3 kg/m2, 44♀] wore an activPAL monitor on their thigh for 7.0 ± 0.3 days. Ten minutes of supine systolic arterial pressure was measured via finger photoplethysmography (115 ± 11 mmHg). Beat-by-beat systolic BPV was measured using the average real variability index (1.1 ± 0.6 mmHg). Relationships between habitual activity outcomes and BPV were assessed via multiple regressions adjusted for age, sex, and BMI. Moderate-intensity physical activity (average: 36 ± 19 min day−1; β = −0.010, p = 0.02) and time spent in sedentary bouts >1-h (245 ± 134 min day−1; β = 0.002, p < 0.001), but not light-intensity activity, vigorous-intensity activity, standing time, sedentary breaks, or time spent in sedentary bouts <1-h (all, p > 0.10) were predictors of systolic BPV. Higher moderate physical activity and lower prolonged sedentary time were associated with attenuated systolic BPV responses in young adults. These findings highlight the cardiovascular benefits of habitual activity among younger adults and suggest that simple strategies such as reducing long periods of uninterrupted sitting and increasing moderate-intensity physical activity may be efficacious for reducing the risk of developing or delaying the onset of hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Ross R, Tremblay M. Introduction to the Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45:v–xi.
Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN) – terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75.
Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370:591–603.
Padwal RS, Bienek A, McAlister FA, Campbell NRC. Epidemiology of hypertension in Canada: an update. Can J Cardiol. 2016;32:687–94.
da Silva GO, Santini LB, Farah BQ, Germano-Soares AH, Correia MA, Ritti-Dias RM. Effects of breaking up prolonged sitting on cardiovascular parameters: a systematic review. Int J Sports Med. 2022;43:97–106.
Arroll B, Beaglehole R. Does physical activity lower blood pressure: a critical review of the clinical trials. J Clin Epidemiol. 1992;45:439–47.
De Venecia T, Lu M, Figueredo VM. Hypertension in young adults. Postgrad Med. 2016;128:201–7.
Mena LJ, Felix VG, Melgarejo JD, Maestre GE. 24‐hour blood pressure variability assessed by average real variability: a systematic review and meta‐analysis. J Am Heart Assoc. 2022;6:e006895.
Bilo G, Dolan E, O’Brien E, Facchetti R, Soranna D, Zambon A, et al. The impact of systolic and diastolic blood pressure variability on mortality is age dependent: data from the Dublin Outcome Study. Eur J Prev Cardiol. 2020;27:355–64.
Rosei EA, Chiarini G, Rizzoni D. How important is blood pressure variability? Eur Hear J Suppl. 2020;22: Supplement_E E1–6.
Kinoshita H, Saku K, Mano J, Mannoji H, Kanaya S, Sunagawa K. Very short-term beat-by-beat blood pressure variability in the supine position at rest correlates well with the nocturnal blood pressure variability assessed by ambulatory blood pressure monitoring. Hypertens Res. 2022;45:1008–17.
Frattola A, Parati G, Cuspidi C, Albini F, Mancia G. Prognostic value of 24-hour blood pressure variability. J Hypertens. 1993;11:1133–7.
Palatini P, Penzo M, Racioppa A, Zugno E, Guzzardi G, Anaclerio M, et al. Clinical relevance of nighttime blood pressure and of daytime blood pressure variability. Arch Intern Med. 1992;152:1855–60.
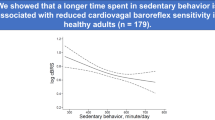
Mori S, Kosaki K, Matsui M, Takahashi K, Yoshioka M, Tarumi T, et al. Sedentary behavior is associated with reduced cardiovagal baroreflex sensitivity in healthy adults. Hypertens Res. 2022;45:1193–202.
O’Brien MW, Al-Hinnawi A, Wu Y, Petterson JL, Shivgulam ME, Johns JA, et al. The influence of habitual breaks in sedentary time on cardiovagal baroreflex function. Appl Physiol Nutr Metab. 2021;46:1143–6.
Colón NV, Santana Bagur JL, Ramírez-Marrero FA. Associations between blood pressure variability, salt intake, physical activity, and sedentary time in HIV+ hispanics: 1345. Med Sci Sport Exerc. 2021;53:442.
Paterson C, Fryer S, Stone K, Zieff G, Turner L, Stoner L. The effects of acute exposure to prolonged sitting, with and without interruption, on peripheral blood pressure among adults: a systematic review and meta-analysis. Sport Med. 2022;52:1369–83.
Shivgulam ME, O’Brien MW, Johns JA, Petterson JL, Wu Y, Frayne RJ, et al. Impact of habitual sedentary patterns on popliteal artery endothelial-dependent vasodilation in healthy adults. Vasc Med. 2022;27:120–6.
O’Brien MW, Johns JA, Williams TD, Kimmerly DS. Sex does not influence impairments in popliteal endothelial-dependent vasodilator or vasoconstrictor responses following prolonged sitting. J Appl Physiol. 2019;127:679–87.
Mena L, Pintos S, Queipo NV, Aizpúrua JA, Maestre G, Sulbarán T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23:505–11.
Pierdomenico SD, Di Nicola M, Esposito AL, Di Mascio R, Ballone E, Lapenna D, et al. Prognostic value of different indices of blood pressure variability in hypertensive patients. Am J Hypertens. 2009;22:842–7.
Edwardson CL, Winkler EAH, Bodicoat DH, Yates T, Davies MJ, Dunstan DW, et al. Considerations when using the activPAL monitor in field-based research with adult populations. J Sport Heal Sci 2017;6:162–78.
Johns JA, Frayne RJ, Goreham JA, Kimmerly DS, O’Brien MW. The bout cadence method improves the quantification of stepping cadence in free-living conditions. Gait Posture. 2020;79:96–101.
O’Brien MW, Johns JA, Fowles JR, Kimmerly DS. Validity of the activPAL and height-adjusted curvilinear cadence-METs equations in healthy adults. Meas Phys Educ Exerc Sci. 2020;24:147–56.
Sala R, Malacarne M, Pagani M, Lucini D. Evidence of increased cardiac parasympathetic drive in subjects meeting current physical activity recommendations. Clin Auton Res. 2015;25:285–91.
Stewart KJ, Ouyang P, Bacher AC, Lima S, Shapiro EP. Exercise effects on cardiac size and left ventricular diastolic function: relationships to changes in fitness, fatness, blood pressure and insulin resistance. Heart. 2006;92:893–8.
Vittinghoff E, Shiboski S, Glidden D, McCulloch C. Regression methods in biostatistics: linear, logistic, survival and repeated measures models. (New York Springer, 2004).
O’Brien MW, Al-Hinnawi A, Wu Y, Petterson JL, Shivgulam ME, Johns JA, et al. The influence of habitual breaks in sedentary time on cardiovagal baroreflex function. Appli Physiol, Nutr Metab. 2021;46:1143–6.
Credeur DP, Miller SM, Jones R, Stoner L, Dolbow DR, Fryer SM, et al. Impact of prolonged sitting on peripheral and central vascular health. Am J Cardiol. 2019;123:260–6.
Sobierajski FM, Purdy GM, Usselman CW, Skow RJ, James MA, Chari RS, et al. Maternal physical activity is associated with improved blood pressure regulation during late pregnancy. Can J Cardiol. 2018;34:485–91.
Tudor-Locke C, Han H, Aguiar E, Barreira T, Schuna JJ, Kang M, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sport Med. 2018;52:776–88.
O’Brien MW, Wu Y, Petterson JL, Bray NW, Kimmerly DS. Validity of the ActivPAL monitor to distinguish postures: a systematic review. Gait Posture. 2022;94:107–13.
Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS data brief. MD: National Center for Health Statistics. 2017;289.
Bakker EA, van Bakel BMA, Aengevaeren WRM, Meindersma EP, Snoek JA, Waskowsky WM, et al. Sedentary behaviour in cardiovascular disease patients: Risk group identification and the impact of cardiac rehabilitation. Int J Cardiol. 2021;326:194–201.
Funding
Canadian Foundation for Innovation: Leader’s Opportunity Fund (DSK), Faculty of Health Research Development (DSK), and Nova Scotia Health Research Foundation (NSHRF) Development/Innovation (DSK) grants. MWO was supported by a CIHR Post-Doctoral Fellowship Award (#181747) and a Dalhousie University Department of Medicine University Internal Medicine Research Foundation Research Fellowship Award. MES was supported by a Heart & Stroke BrightRed Scholarship. BDS and JLP were supported by a Fredrick Banting and Charles Best CIHR Masters Awards. BDS and MES were supported by Nova Scotia Graduate Scholarships.
Author information
Authors and Affiliations
Contributions
BDS and MWO conceived the study. All authors contributed to data collection and/or data analysis. BDS and MWO drafted the manuscript. All authors edited the manuscript and approved of the final version of the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All protocols and procedures conformed to the Declaration of Helsinki and were approved by the Dalhousie University Health Sciences Research Ethics Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schwartz, B.D., Shivgulam, M.E., Petterson, J.L. et al. More moderate-intensity physical activity and less prolonged sedentary time are associated with better very short-term systolic blood pressure variability in healthy adults. J Hum Hypertens 37, 1015–1020 (2023). https://doi.org/10.1038/s41371-023-00832-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00832-y