Abstract
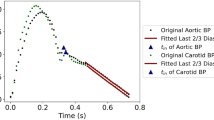
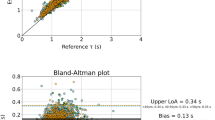
Early-life exposure to high blood pressure (BP) is associated with cardiovascular target organ damage but not all BP-related risk is attributable to systolic and diastolic BP alone. In adolescence, aortic wave separation (WS) parameters are associated with increased left ventricular mass index (LVMI) but this approach is limited by the requirement for aortic flow measurements. Several methods for estimating the aortic flow waveform from pressure waveforms have emerged, but their accuracy and associations with LVMI have never been tested in adolescents, which was the aim of our study. Carotid pressure waveforms were acquired by tonometry from 58 adolescents (age 16 ± 1.5 years, 59% female). Measured (aortic) flow and LVMI were acquired via 2D echocardiography. Three pressure-only approximations of aortic flow were synthesized, including triangular, excess, and individualized-physiologic flow. A 4th aortic flow (average flow) was approximated from the average of all 58 measured flow waveforms. Forward (Pf) and backward (Pb) pressure and reflection magnitude (Rm) were derived from WS analysis. The individualized-physiologic flow produced the best approximations of Pf (mean difference ± SD, −0.15 ± 2.38 mmHg), Pb (0.14 ± 0.25 mmHg), and Rm (0.01 ± 0.02 mmHg). Pf derived using measured, individualized-physiologic, and average flow, was similarly associated with LVMI adjusting for age, brachial systolic BP, cardiac output, and BMI (P ≤ 0.03 all). Pb derived using all flow waveforms was associated with LVMI and all associations yielded similar effect estimates. Of the estimated flow waveforms, individualized-physiologic flow yielded the best approximation of WS parameters and may provide important physiological and clinical insight among adolescents.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available upon reasonable request.
References
Bell CS, Samuel JP, Samuels JA. Prevalence of hypertension in children: applying the new American Academy of Pediatrics Clinical Practice Guideline. Hypertension. 2019;73:148–52.
Berenson GS, Wattigney WA, Tracy RE, Newman WP, Srinivasan SR, Webber LS, et al. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (the Bogalusa Heart Study). Am J Cardiol. 1992;70:851–8.
Yang L, Magnussen CG, Yang L, Bovet P, Xi B. Elevated blood pressure in childhood or adolescence and cardiovascular outcomes in adulthood: a systematic review. Hypertension. 2020;75:948–55.
Westerhof N, Sipkema P, van den Bos GC, Elzinga G. Forward and backward waves in the arterial system. Cardiovascular Res. 1972;6:648–56.
Cooper LL, Rong J, Benjamin EJ, Larson MG, Levy D, Vita JA, et al. Components of hemodynamic load and cardiovascular events the framingham heart study. Circulation. 2015;131:354–61.
Zamani P, Lilly SM, Segers P, Jacobs DR, Bluemke DA, Duprez DA, et al. Pulsatile load components, resistive load and incident heart failure: The Multi-Ethnic Study of Atherosclerosis (MESA). J Card Fail. 2016;22:988–95.
Zamani P, Jacobs DR, Segers P, Duprez DA, Brumback L, Kronmal RA, et al. Reflection magnitude as a predictor of mortality the multi-ethnic study of atherosclerosis. Hypertension. 2014;64:958–64.
Pierce GL, Pajaniappan M, Dipietro A, Darracott-Woei-A-Sack K, Kapuku GK. Abnormal central pulsatile hemodynamics in adolescents with obesity: Higher aortic forward pressure wave amplitude is independently associated with greater left ventricular mass. Hypertension. 2016;68:1200–7.
Westerhof BE, Guelen I, Westerhof N, Karemaker JM, Avolio A. Quantification of wave reflection in the human aorta from pressure alone: a proof of principle. Hypertension. 2006;48:595–601.
Kips JG, Rietzschel ER, De Buyzere ML, Westerhof BE, Gillebert TC, Van Bortel LM, et al. Evaluation of noninvasive methods to assess wave reflection and pulse transit time from the pressure waveform alone. Hypertension. 2009;53:142–9.
Shenouda N, Stock JM, Patik JC, Chirinos JA, Edwards DG. Personalized physiologic flow waveforms improve wave reflection estimates compared to triangular flow waveforms in adults. Am J Physiol-Heart Circulatory Physiol. 2021;320:H1802–12.
Qasem A, Avolio A. Determination of aortic pulse wave velocity from waveform decomposition of the central aortic pressure pulse. Hypertension. 2008;51:188–95.
Hametner B, Wassertheurer S, Kropf J, Mayer C, Holzinger A, Eber B, et al. Wave reflection quantification based on pressure waveforms alone-methods, comparison, and clinical covariates. Computer Methods Prog Biomedicine. 2013;109:250–9.
Kelly R, Fitchett D. Noninvasive determination of aortic input impedance and external left ventricular power output: a validation and repeatability study of a new technique. J Am Coll Cardiol. 1992;20:952–63.
Khir AW, O’Brien A, Gibbs JSR, Parker KH. Determination of wave speed and wave separation in the arteries. J Biomech. 2001;34:1145–55.
Armstrong MK, Schultz MG, Hughes AD, Picone DS, Black JA, Dwyer N, et al. Excess pressure as an analogue of blood flow velocity. J Hypertension. 2021;39:421–7.
Kapuku GK, Ge D, Vemulapalli S, Harshfield GA, Treiber FA, Snieder H. Change of genetic determinants of left ventricular structure in adolescence: Longitudinal evidence from the Georgia Cardiovascular Twin Study. Am J Hypertension. 2008;21:799–805.
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr. 1989;2:358–67.
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, et al. Left ventricular mass and body size in normotensive children and adults: Assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–60.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8.
Lin LI-K. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255.
McBride G. A proposal for strength-of-agreement criteria for Lin’s concordance correlation coefficient. NIWA Client Rep. 2005;45:307–10.
Hittner JB, May K, Silver NC. A Monte Carlo evaluation of tests for comparing dependent correlations. J Gen Psychol. 2003;130:149–68.
Heckman MG, Davis JM, Crowson CS. Post Hoc power calculations: an inappropriate method for interpreting the findings of a research study. J Rheumatol. 2022;49:867–70.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical Practice Guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
Weber T, Wassertheurer S, Rammer M, Haiden A, Hametner B, Eber B. Wave reflections, assessed with a novel method for pulse wave separation, are associated with end-organ damage and clinical outcomes. Hypertension. 2012;60:534–41.
Lai CC, Sun D, Cen R, Wang J, Li S, Fernandez-Alonso C, et al. Impact of long-term burden of excessive adiposity and elevated blood pressure from childhood on adulthood left ventricular remodeling patterns: The Bogalusa Heart Study. J Am Coll Cardiol. 2014;64:1580–7.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N. Engl J Med. 1990;322:1561–6.
Funding
This study was supported by Child Health Discovery Institute pilot grant (awarded to Dr. Pierce), Medical College of Georgia, Augusta University. GLP is supported by grants from NIH R01 AG063790 and the American Heart Association 19TPA34910016, and by the Russell B. Day and Florence D. Day Chair in Liberal Arts and Sciences at the University of Iowa. MKA is supported by a National Institutes of Health Iowa Training Program in Kidney and Hypertension Research Fellowship grant (T32DK007690). JAC is supported by NIH grants R01 HL121510, U01 TR003734, U01 TR00373401S1, UO1 HL160277, R33 HL146390, R01 HL153646, K24 AG070459, R01 AG058969, R01 HL104106, P01 HL094307, R03 HL146874, R56 HL136730, R01 HL157108, R01 HL155764, R01-HL155599, R01 HL157264, and 1R01 HL153646. He has recently consulted for Bayer, Sanifit, Fukuda-Denshi, Bristol-Myers Squibb, JNJ, Edwards Life Sciences, Merck, NGM Biopharmaceuticals and the Galway-Mayo Institute of Technology. He received University of Pennsylvania research grants from National Institutes of Health, Fukuda-Denshi, Bristol-Myers Squibb, Microsoft and Abbott. He is named as inventor in a University of Pennsylvania patent for the use of inorganic nitrates/nitrites for the treatment of Heart Failure and Preserved Ejection Fraction and for the use of biomarkers in heart failure with preserved ejection fraction. He has received payments for editorial roles from the American Heart Association, the American College of Cardiology and Wiley. He has received research device loans from Atcor Medical, Fukuda-Denshi, Unex, Uscom, NDD Medical Technologies, Microsoft and MicroVision Medical.
Author information
Authors and Affiliations
Contributions
MA—Conception, data interpretation and manuscript preparation and revision. JC—Data interpretation, and critical manuscript revision. GK—Data interpretation and critical manuscript revision. GP—Data interpretation and critical manuscript revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Armstrong, M.K., Chirinos, J.A., Kapuku, G.K. et al. Aortic pressure-only wave separation analysis in adolescents: accuracy and associations with left ventricular mass index. J Hum Hypertens 37, 1119–1125 (2023). https://doi.org/10.1038/s41371-022-00757-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00757-y