Abstract
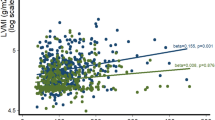
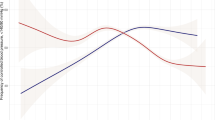
Hypertension-mediated organ damage (HMOD) at cardiac level include a variety of abnormal phenotypes of recognized adverse prognostic value. Although the risk of cardiac HMOD is related with the severity of BP elevation, the interaction of numerous non-hemodynamic factors plays a relevant role in this unfavorable dynamic process. In particular, sex-related differences in cardiovascular (CV) risk factors and HMOD have been increasingly described. The objective of the present review is to provide comprehensive, updated information on sex-related differences in cardiac HMOD, focusing on the most important manifestations of subclinical hypertensive heart disease such as left ventricular hypertrophy (LVH), LV systolic and diastolic dysfunction, left atrial and aortic dilatation. Current evidence, based on cross-sectional and longitudinal observational studies as well as real-world registries and randomized controlled trials, suggests that women are more at risk of developing (and maintaining) LVH, concentric remodeling and subclinical LV dysfunction, namely the morpho-functional features of heart failure with preserved ejection fraction. It should be pointed out, however, that further studies are needed to fill the gap in defining gender-based optimal therapeutic strategies in order to protect women’s hearts.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:2284–309.
Le TT, Lim V, Ibrahim R, Teo MT, Bryant J, Ang B, et al. The remodelling index risk stratifies patients with hypertensive left ventricular hypertrophy. Eur Heart J Cardiovasc Imaging. 2021;22:670–9.
Hoang K, Zhao Y, Gardin JM, Carnethon M, Mukamal K, Yanez D, et al. LV mass as a predictor of CVD events in older adults with and without metabolic syndrome and diabetes. JACC Cardiovasc Imaging. 2015;8:1007–15.
Tripepi G, D’Arrigo G, Mallamaci F, London G, Tangri N, Hsu JY, et al. Prognostic values of left ventricular mass index in chronic kidney disease patients. Nephrol Dial Transpl. 2021;36:665–72.
Zhang H, Hu L, Wei XJ. Prognostic value of left ventricular hypertrophy in hypertensive patients: a meta-analysis of electrocardiographic studies. Clin Hypertens. 2020;22:254–60.
Devereux RB, Wachtell K, Gerdts E, Boman K, Nieminen MS, Papademetriou V, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA. 2004;292:2350–6.
Pierdomenico SD, Lapenna D, Cuccurullo F. Regression of echocardiographic left ventricular hypertrophy after 2 years of therapy reduces cardiovascular risk in patients with essential hypertension. Am J Hypertens. 2008;21:464–70.
Sheng Y, Li M, Xu M, Zhang Y, Xu J, Huang Y, et al. Left ventricular and atrial remodelling in hypertensive patients using thresholds from international guidelines and EMINCA data. Eur Heart J Cardiovasc Imaging. 2022;23:166–74.
Ikejder Y, Sebbani M, Hendy I, Khramz M, Khatouri A, Bendriss L. Impact of arterial hypertension on left atrial size and function. Biomed Res Int. 2020;2020:2587530.
Lilja-Cyron A, Bang CN, Gerdts E, Larstorp AC, Kjeldsen SE, Julius S, et al. Aortic root dilatation in hypertensive patients with left ventricular hypertrophy-application of a new multivariate predictive model. The Life Study. Rev Cardiovasc Med. 2022;23:95.
Nakanishi K, Daimon M, Yoshida Y, Ishiwata J, Sawada N, Hirokawa M, et al. Blood pressure categorization and subclinical left ventricular dysfunction in antihypertensive medication-naive subjects. ESC Heart Fail. 2022;9:1766–74.
Mancia G, Zanchetti A, Agabiti-Rosei E, Benemio G, De Cesaris R, Fogari R, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment induced regression of left ventricular hypertrophy. SAMPLE Study Group. Study on Ambulatory Monitoring of Blood Pressure and Lisinopril Evaluation. Circulation. 1997;95:1464–70.
Sivén SS, Niiranen TJ, Langén VL, Puukka PJ, Kantola IM, Jula AM. Home versus office blood pressure: longitudinal relations with left ventricular hypertrophy: the Finn-Home study. J Hypertens. 2017;35:266–71.
Nwabuo CC, Vasan RS. Pathophysiology of hypertensive heart disease: beyond left ventricular hypertrophy. Curr Hypertens Rep. 2020;22:11.
Cosenso-Martin LN, Vaz-de-Melo RO, Pereira LR, Cesarino CB, Yugar-Toledo JC, Cipullo JP, et al. Angiotensin-converting enzyme insertion/deletion polymorphism, 24-h blood pressure profile and left ventricular hypertrophy in hypertensive individuals: a cross-sectional study. Eur J Med Res. 2015;20:74.
Pi M, Ye R, Han X, Armstrong B, Liu X, Chen Y, et al. Cardiovascular interactions between fibroblast growth factor-23 and angiotensin ii. Sci Rep. 2018;8:12398.
Song WH, Lin YH, Sun K, Zhang YH, Song Y, Hou LB, et al. A functional variant in the coding region of CAMTA2 is associated with left ventricular hypertrophy by affecting the activation of Nkx2.5-dependent transcription. J Hypertens. 2016;34:942–9.
Ahmad FS, Cai X, Kunkel K, Ricardo AC, Lash JP, Raj DS, et al. CRIC Study Investigators. Racial/ethnic differences in left ventricular structure and function in chronic kidney disease: The Chronic Renal Insufficiency Cohort. Am J Hypertens. 2017;30:822–9.
Lucà F, Abrignani MG, Parrini I, Di Fusco SA, Giubilato S, Rao CM, et al. Update on management of cardiovascular diseases in women. J Clin Med. 2022;11:1176.
Pfeilschifter J, Koditz R, Pfohl M, Schatz H. Changes in proinflammatory cytokine activity after menopause. Endocr Rev. 2002;23:90–119.
Sabbatini AR, Kararigas G. Estrogen-related mechanisms in sex differences of hypertension and target organ damage. Biol Sex Differ. 2020;11:31.
Li S, Gupte AA. The role of estrogen in cardiac metabolism and diastolic function. Methodist Debakey Cardiovasc J. 2017;13:4–8.
Pedersen LR, Kristensen AMD, Petersen SS, Vaduganathan M, Bhatt DL, Juel J, et al. Prognostic implications of left ventricular hypertrophy diagnosed on electrocardiogram vs echocardiography. J Clin Hypertens. 2020;22:1647–58.
Vasan RS, Song RJ, Xanthakis V, Beiser A, DeCarli C, Mitchell GF, et al. Hypertension-mediated organ damage prevalence, correlates, and prognosis in the community. Hypertension. 2022;79:505–15.
Tanaka K, Tanaka F, Onoda T, Tanno K, Ohsawa M, Sakata K, et al. Iwate-Kenco Study Group Prognostic Value of Electrocardiographic Left Ventricular Hypertrophy on Cardiovascular Risk in a Non-Hypertensive Community-Based Population. Am J Hypertens. 2018;31:895–901.
Perrone-Filardi P, Coca A, Galderisi M, Paolillo S, Alpendurada F, de Simone G, et al. Non-invasive cardiovascular imaging for evaluating subclinical target organ damage in hypertensive patients: A consensus paper from the European Association of Cardiovascular Imaging (EACVI), the European Society of Cardiology Council on Hypertension, and the European Society of Hypertension (ESH). Eur Heart J Cardiovasc Imaging. 2017;18:945–60.
Cuspidi C, Rescaldani M, Sala C, Negri F, Grassi G, Mancia G. Prevalence of electrocardiographic left ventricular hypertrophy in human hypertension: an updated review. J Hypertens. 2012;30:2066–73.
dos Santos JPA, Ribeiro ALP, Andrade-Junior D, Marcolino MS. Prevalence of electrocardiographic abnormalities in primary care patients according to sex and age group. A retrospective observational study. Sao Paulo Med J. 2018;136:20–8.
Cuspidi C, Sala C, Negri F, Mancia G, Morganti A. Italian Society of Hypertension. Prevalence of left-ventricular hypertrophy in hypertension: an updated review of echocardiographic studies. J Hum Hypertens. 2012;26:343–9.
Gerdts E, Okin PM, de Simone G, Cramariuc D, Wachtell K, Boman K, et al. Gender differences in left ventricular structure and function during antihypertensive treatment: the Losartan Intervention for Endpoint Reduction in Hypertension Study. Hypertension. 2008;51:1109–14.
de Simone G, Devereux RB, Izzo R, Girfoglio D, Lee ET, Howard BV, et al. Lack of reduction of left ventricular mass in treated hypertension: the Strong Heart Study. J Am Heart Assoc. 2013;2:e000144.
Gerdts E, Izzo R, Mancusi C, Losi MA, Manzi MV, Canciello G, et al. Left ventricular hypertrophy offsets the sex difference in cardiovascular risk (the Campania Salute Network). Int J Cardiol. 2018;258:257–61.
Cai A, Liu L, Zhou D, Tang S, Zhou Y, Feng Y. Influences of achieved SBP on age and sex-related left ventricular structural alteration in community hypertensive populations. J Hypertens. 2022;40:1170–8.
de Simone G, Mancusi C, Izzo R, Losi MA, Ferrara LA. Obesity and hypertensive heart disease: focus on body composition and sex difference. Diabetol Metab Syndr. 2016;8:79.
Nunez E, Arnett DK, Benjamin EJ, Oakes JM, Liebson PR, Skelton TN. Comparison of the prognostic value of left ventricular hypertrophy in African-American men versus women. Am J Cardiol. 2004;94:1383–90.
Okin PM, Gerdts E, Kjeldsen SE, Julius S, Edelman JM, Dahlöf B, et al. Losartan Intervention for Endpoint Reduction in Hypertension Study Investigators. Gender differences in regression of electrocardiographic left ventricular hypertrophy during antihypertensive therapy. Hypertension 2008;52:100–6.
Gerdts E, Okin PM, de Simone G, Cramariuc D, Wachtell K, Boman K, et al. Gender differences in left ventricular structure and function during antihypertensive treatment: the Losartan Intervention for Endpoint Reduction in Hypertension Study. Hypertension 2008;51:1109–14.
Lønnebakken MT, Izzo R, Mancusi C, Gerdts E, Losi MA, Canciello G, et al. Left ventricular hypertrophy regression during antihypertensive treatment in an outpatient clinic (the Campania Salute Network. Am Heart Assoc. 2017;6:e004152.
Voorhees AP, Han HC. Biomechanics of cardiac function. Compr Physiol. 2016;5:1623–44.
Pichler G, Redon J, Martínez F, Solaz E, Calaforra O, Andrés MS, et al. Cardiac magnetic resonance-derived fibrosis, strain and molecular biomarkers of fibrosis in hypertensive heart disease. J Hypertens. 2020;38:2036–42.
Zanchetti A, Cuspidi C, Comarella L, Agabiti Rosei A, Ambrosioni E, Chiariello M, et al. Left ventricular diastolic dysfunction in elderly hypertensives: results of the APROS-diadys study. J Hypertens. 2007;25:2158–67.
Fujimoto N, Okada Y, Shibata S, Best SA, Bivens TB, Levine BD, et al. Effects of sex and hypertension subtype on haemodynamics and left ventricular diastolic function in older patients with stage 1 hypertension. J Hypertens. 2013;31:2282–9.
Hoshida S, Shinoda Y, Ikeoka K, Fukuoka H, Inui H, Watanabe T. Age- and sex-related differences in diastolic function and cardiac dimensions in a hypertensive population. ESC Heart Fail. 2016;3:270–7.
Cai A, Zhou D, Liu L, Zhou Y, Tang S, Feng Y. Age-related alterations in cardiac and arterial structure and function in hypertensive women and men. Clin Hypertens. 2021;23:1322–34.
Sotomi Y, Hikoso S, Nakatani D, Mizuno H, Okada K, Dohi T, et al. PURSUIT‐HFpEF Investigators. Sex differences in heart failure with preserved ejection fraction. J Am Heart Assoc. 2021;10:e018574.
Khan SS, Beach LB, Yancy CW. Sex-based differences in heart failure: JACC Focus Seminar 7/7. J Am Coll Cardiol. 2022;79:1530–41.
Tadic M, Cuspidi C, Celic V, Ivanovic B, Pencic B, Grassi G. The influence of sex on left ventricular strain in hypertensive population. J Hypertens. 2019;37:50–6.
Stacey RB, Hundley WG. Integrating measures of myocardial fibrosis in the transition from hypertensive heart disease to heart failure. Curr Hypertens Rep. 2021;23:22.
Chen XJ, Sun XL, Zhang Q, Gao XL, Liang YJ, Jiang J, et al. Uncontrolled blood pressure as an independent risk factor of early impaired left ventricular systolic function in treated hypertension. Echocardiography. 2016;33:1488–94.
de Simone G, Devereux RB, Koren MJ, Mensah GA, Casale PN, Laragh JH. Midwall left ventricular mechanics. An independent predictor of cardiovascular risk in arterial hypertension. Circulation. 1996;93:259–65.
Biering-Sørensen T, Biering-Sørensen SR, Olsen FJ, Sengeløv M, Jørgensen PG, Mogelvang R, et al. Global longitudinal strain by echocardiography predicts long-term risk of cardiovascular morbidity and mortality in a low-risk general population: The Copenhagen City Heart Study. Circ Cardiovasc Imaging. 2017;10:e005521.
Saito M, Khan F, Stoklosa T, Iannaccone A, Negishi K, Marwick TH. Prognostic implications of lv strain risk score in asymptomatic patients with hypertensive heart disease. JACC Cardiovasc Imaging. 2016;9:911–21.
Modin D, Biering-Sørensen SR, Mogelvang R, Landler N, Jensen JS, Biering-Sørensen T. Prognostic value of echocardiography in hypertensive versus non-hypertensive participants from the general population. Hypertension. 2018;71:742–51.
Tadic M, Sala C, Carugo S, Mancia G, Grassi G, Cuspidi C. Myocardial strain in hypertension: a meta-analysis of two-dimensional speckle tracking echocardiographic studies. J Hypertens. 2021;39:2103–12.
Park JH, Lee JH, Lee SY, Choi JO, Shin MS, Kim MJ, et al. Normal 2- dimensional strain values of the left ventricle: a sub-study of the normal echocardiographic measurements in Korean Population Study. J Cardiovasc Ultrasound. 2016;24:285–93.
Kuznetsova T, Herbots L, Richart T, D’hooge J, Thijs L, Fagard RH, et al. Left ventricular strain and strain rate in a general population. Eur Heart J. 2008;29:2014–23.
Kocabay G, Muraru D, Peluso D, Cucchini U, Mihaila S, Padayattil-Jose S, et al. Normal left ventricular mechanics by two-dimensional speckle-tracking echocardiography. Reference values in healthy adults. Rev Esp Cardiol. 2014;67:651–8.
Hung CL, Gonçalves A, Shah AM, Cheng S, Kitzman D, Solomon SD. Age- and sex-related influences on left ventricular mechanics in elderly individuals free of prevalent heart failure: The ARIC Study (Atherosclerosis Risk in Communities). Circ Cardiovasc Imaging. 2017;10:e004510.
Douglas P. The left atrium. A biomarker of chronic diastolic dysfunction and cardiovascular disease risk. J Am Coll Cardiol. 2003;42:1206–7.
Peng J, Laukkanen JA, Zhao Q, Wang L, Zhang X, Li G. Association of left atrial enlargement with ventricular remodeling in hypertensive Chinese elderly. Echocardiography. 2017;34:491–5.
Mancusi C, Canciello G, Izzo R, Damiano S, Grimaldi MG, de Luca N, et al. Left atrial dilatation: a target organ damage in young to middle-age hypertensive patients. The Campania Salute Network. Int J Cardiol. 2018;265:229–33.
Soullier C, Niamkey JT, Ricci JE, Messner-Pellenc P, Brunet X, Schuster I. Hypertensive patients with left ventricular hypertrophy have global left atrial dysfunction and impaired atrio-ventricular coupling. J Hypertens. 2016;34:1615–20.
Nagarajaro HS, Penman AD, Taylor HA, Mosley TH, Butler K, Skelton TN, et al. The predictive value of left atrial size for incident ischemic stroke and all-cause mortality in African Americans. The Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2008;39:2701–6.
Bombelli M, Facchetti R, Cuspidi C, Villa P, Dozio D, Brambilla G, et al. Prognostic significance of left atrial enlargement in a general population: results of the PAMELA study. Hypertension. 2014;64:1205–11.
Wachtell K, Devereux RB, Lyle PA, Okin PM, Gerdts E. The left atrium, atrial fibrillation, and the risk of stroke in hypertensive patients with left ventricular hypertrophy. Ther Adv Cardiovasc Dis. 2008;2:507–13.
Aurigemma GP, Gottdiener JS, Arnold AM, Chinali M, Hill JC, Kitzman D. Left atrial volume and geometry in healthy aging. The Cardiovascular Health Study. Circ Cardiovasc Imaging. 2009;2:282–9.
Gerdts E, Oikarinen L, Palmieri V, Otterstad JE, Wachtell K, Boman K, et al. Correlates of left atrial size in hypertensive patients with left ventricular hypertrophy: the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Hypertension. 2002;39:739–43.
Cuspidi C, Meani S, Fusi V, Valerio C, Catini E, Sala C, et al. Prevalence and correlates of left atrial enlargement in essential hypertension: role of ventricular geometry and the metabolic syndrome: the Evaluation of Target Organ Damage in Hypertension study. J Hypertens. 2005;23:875–82.
Cuspidi C, Negri F, Lonati L, Muiesan ML, Capra A, Milan A, et al. Working Group on Heart and Hypertension of the Italian Society of Hypertension. Prevalence and correlates of echocardiographic left atrial enlargement in hypertensive outpatients in clinical practice. Clin Exp Hypertens. 2011;33:328–35.
Cuspidi C, Rescaldani M, Sala C. Prevalence of echocardiographic left-atrial enlargement in hypertension: a systematic review of recent clinical studies. Am J Hypertens. 2013;26:456–64.
Halland H, Lonnebakken MT, Pristaj N, Saeed S, Midtbø H, Einarsen E, et al. Sex differences in subclinical cardiac disease in overweight and obesity (the FATCOR study). Nutr Metab Cardiovasc Dis. 2018;28:1054–60.
Palmieri V, Bella JN, Arnett DK, Roman MJ, Oberman A, Kitzman DW, et al. Aortic root dilatation at sinuses of Valsalva and aortic regurgitation in hypertensive and normotensive subjects: the Hypertension Genetic Epidemiology Network Study. Hypertension. 2001;37:1229–35.
Bella JN, Wachtell K, Boman K, Palmieri V, Papademetriou V, Gerdts E, et al. Relation of left ventricular geometry and function to aortic root dilatation in patients with systemic hypertension and left ventricular hypertrophy (the LIFE study). Am J Cardiol. 2002;89:337–41.
Cipolli JA, Souza FA, Ferreira-Sae MC, Pio-Magalhães JA, Figueiredo ES, Vidotti VG, et al. Sex-specific hemodynamic and non-hemodynamic determinants of aortic root size in hypertensive subjects with left ventricular hypertrophy. Hypertens Res. 2009;32:956–61.
Lønnebakken MT, Izzo R, Mancusi C, Losi MA, Stabile E, Rozza F, et al. Aortic root dimension and arterial stiffness in arterial hypertension: the Campania Salute Network. J Hypertens. 2016;34:1109–14.
Canciello G, Mancusi C, Losi MA, Izzo R, Trimarco B, de Simone G, et al. Aortic root dilatation is associated with incident cardiovascular events in a population of treated hypertensive patients: the Campania salute network. Am J Hypertens. 2018;31:1317–23.
Leone D, Airale L, Bernardi S, Mingrone G, Astarita A, Cesareo M, et al. Prognostic role of the ascending aorta dilatation in patients with arterial hypertension. J Hypertens. 2021;39:1163–9.
Cuspidi C, Meani S, Fusi V, Valerio C, Sala C, Zanchetti A. Prevalence and correlates of aortic root dilatation in patients with essential hypertension relationship with cardiac and extra-cardiac organ damage. J Hypertens. 2006;24:573–80.
Milan A, Avenatti E, Tosello F, Iannaccone A, Leone D, Magnino C, et al. Aortic root dilatation in essential hypertension: prevalence according to new reference values. J Hypertens. 2013;31:1189–95.
Covella M, Milan A, Totaro S, Cuspidi C, Re A, Rabbia F, et al. Echocardiographic aortic root dilatation in hypertensive patients: a systematic review and meta-analysis. J Hypertens. 2014;32:1928–35.
Milan A, Degli Esposti D, Salvetti M, Izzo R, Moreo A, Pucci G, et al. Working Group on Heart and Hypertension of the Italian Society of Hypertension. Prevalence of proximal ascending aorta and target organ damage in hypertensive patients: the multicentric ARGO-SIIA project (Aortic Remodelling in hypertension of the Italian Society of Hypertension). J Hypertens. 2019;37:57–64.
Biffi A, Rea F, Iannaccone T, Filippelli A, Mancia G, Corrao G. Sex differences in the adherence of antihypertensive drugs: a systematic review with meta-analyses. BMJ Open. 2020;10:e036418.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441–50.
Skeete J, Ramsey E, Battle S, DiPette DJ. Sex-based differences in hypertension: understanding the trends. Clin Hypertens. 2021;23:1129–32.
Author information
Authors and Affiliations
Contributions
CC planned the general design of the review and wrote the first draft; EG and CS carried out the research and analysis of the relevant literature, and prepared the figures. MT contributed to the final draft preparation of the paper. All authors made their critical contributions to the final paper and its subsequent revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cuspidi, C., Gherbesi, E., Sala, C. et al. Sex, gender, and subclinical hypertensiveorgan damage—heart. J Hum Hypertens 37, 626–633 (2023). https://doi.org/10.1038/s41371-022-00750-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00750-5
This article is cited by
-
Journal of Human Hypertension special issue on sex and gender differences in hypertension
Journal of Human Hypertension (2023)
-
Hypertensive organ damage: the vulnerable heart of women
Journal of Human Hypertension (2023)