Abstract
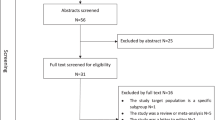
This review aims to explore the burden of hypertension among refugees in the Middle East by reporting its prevalence, risk factors and access to care. A comprehensive literature search was performed using Web of Science, Ovid MEDLINE, PubMed, SCOPUS, CINHAL+, WHO Regional Office for the Eastern Mediterranean (EMRO) and United Nations High Commissioner for Refugees (UNHCR) on articles spanning from 1948 until 2020. Most studies were cross-sectional in design. After applying eligibility criteria 17 articles and 4 reports were included. Findings showed that hypertension represents a major burden among refugees. Hypertension risk factors present among the refugee population included increased salt intake, physical inactivity, and smoking. The majority of hypertensive refugees sought care for their condition at the public health care services. Barriers to seeking care included high cost of healthcare, accessibility to provided services, and lack of knowledge for the need to seek care. Non-adherence to medication among refugees was primarily linked to cost and lack of symptoms. This review highlights the need for further studies to shed light on the importance of targeting hypertension among refugees, to lower morbidity and mortality, in addition to providing adequate healthcare services to this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev. Nephrol. 2020;16:223–37.
Zhou B, Bentham J, di Cesare M, Bixby H, Danaei G, Cowan MJ, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389:37–55.
Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–94.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334–57. 2020
Yusufali A, Khatib R, Islam S, AlHabib K, Kelishadi R, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in the middle east. J Hypertension. 2017;35:1457–64.
UNHCR. Figures at a Glance. https://www.unhcr.org/figures-at-a-glance.html.
UNHCR. Middle East - Global Focus. 2020. https://reporting.unhcr.org/node/36?y=2020.
United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Government of Iraq and IOM share findings of first ever nationwide migration profile- Iraq, ReliefWeb. 2019. https://reliefweb.int/report/iraq/government-iraq-and-iom-share-findings-first-ever-nationwide-migration-profile-enarku.
UNRWA. Palestine refugees. https://www.unrwa.org/palestine-refugees.
UNHCR. Syria refugee crisis explained, UN refugees. 2020. https://www.unrefugees.org/news/syria-refugee-crisis-explained.
Loesche D. Lebanon still has the highest refugees density, statista. 2018. https://www.statista.com/chart/14323/countries-with-most-refugees-per-1000-inhabitants.
UNHCR. Responding to the challenge of non-communicable diseases. https://www.unhcr.org/protection/health/5e1352b67/responding-challenge-non-communicable-diseases.html.
Langlois EV, Haines A, Tomson G, Ghaffar A. RefugeES: TOWARDs better access to health-care services. Lancet 2016;387:319–21.
World Health Organization. Hypertension. 2019. https://www.who.int/news-room/fact-sheets/detail/hypertension.
Mendola D, Busetta A. Health and living conditions of refugees and asylum-seekers: a survey of informal settlements in italy. Refugee Surv Q. 2018;37:477–505.
Rehr M, Shoaib M, Ellithy S, Okour S, Ariti C, Ait-Bouziad I et al. Prevalence of non-communicable diseases and access to care among non-camp Syrian refugees in northern Jordan. Confl Health 2018; 12. https://doi.org/10.1186/s13031-018-0168-7.
Guterres A, Spiegel P. The state of the world’s refugees: Adapting health responses to urban environments. JAMA. 2012;308:673–4.
Doocy S, Lyles E, Roberton T, Akhu-Zaheya L, Oweis A, Burnham G. Prevalence and care-seeking for chronic diseases among Syrian refugees in Jordan. BMC Public Health. 2015;15:1097.
Boulle P, Sibourd-Baudry A, Ansbro É, Prieto Merino D, Saleh N, Zeidan RK, et al. Cardiovascular disease among Syrian refugees: a descriptive study of patients in two Médecins Sans Frontières clinics in northern Lebanon. Confl Health. 2019;13:37.
WHO Stepwise Approach for Non-Communicable Diseases Risk Factors Surveillance-Lebanon, WHO. 2017.
Sethi S, Jonsson R, Skaff R, Tyler F. Community-based noncommunicable disease care for Syrian refugees in Lebanon. Glob Health Sci Pract. 2017;5:495–506.
Mateen FJ, Carone M, Al-Saedy H, Nyce S, Ghosn J, Mutuerandu T, et al. Medical conditions among Iraqi refugees in Jordan: data from the United Nations Refugee Assistance Information System. Bull World Health Organ. 2012;90:444–51.
Doocy S, Sirois A, Tileva M, Storey JD, Burnham G. Chronic disease and disability among Iraqi populations displaced in Jordan and Syria. Int J Health Plan Manag. 2013; 28. https://doi.org/10.1002/hpm.2119.
Doocy S, Lyles E, Hanquart B, Woodman LSTM. Prevalence, care-seeking, and health service utilization for non-communicable diseases among Syrian refugees and host communities in Lebanon. Confl Health 2016; 10. https://doi.org/10.1186/s13031-016-0088-3.
Doocy S, Lyles E, Akhu-Zaheya L, Oweis A, Al Ward N, Burton A. Health service utilization among Syrian refugees with chronic health conditions in Jordan. PLoS ONE 2016; 11. https://doi.org/10.1371/journal.pone.0150088.
Mousa HSA, Yousef S, Riccardo F, Zeidan W, Sabatinelli G. Hyperglycaemia, hypertension and their risk factors among Palestine refugees served by UNRWA. East Mediterranean Health J. 2010;16:460–5.
Massad SG, Khalili M, Karmally W, Abdalla M, Khammash U, Mehari G-M et al. Metabolic syndrome among refugee women from the west bank, Palestine: A cross-sectional study. Nutrients 2018; 10. https://doi.org/10.3390/nu10081118.
Strong J, Varady C, Chahda N, Doocy S, Burnham G. Health status and health needs of older refugees from Syria in Lebanon. Confl Health 2015; 9. https://doi.org/10.1186/s13031-014-0029-y.
Eryurt MA, Menet MG. Noncommunicable diseases among syrian refugees in turkey: an emerging problem for a vulnerable group. J Immigr Minority Health. 2020;22:44–9.
Balcilar M. Health Status Survey of Syrian Refugees in Turkey: Non-communicable Disease Risk Factor Surveillance among Syrian Refugees Living in Turkey. 2016.
Abukhdeir HF, Caplan LS, Reese L, Alema-Mensah E. Factors affecting the prevalence of chronic diseases in Palestinian people: an analysis of data from the Palestinian Central Bureau of Statistics. East Mediterranean Health J. 2013;19:307–13.
Khader A, Farajallah L, Shahin Y, Hababeh M, Abu-Zayed I, Kochi A, et al. Cohort monitoring of persons with hypertension: An illustrated example from a primary healthcare clinic for Palestine refugees in Jordan. Tropical Med Int Health. 2012;17:1163–70.
UNHCR. Health access and utilization survey among Syrian refugees in Lebanon—November 2019—Lebanon, ReliefWeb. https://reliefweb.int/report/lebanon/health-access-and-utilization-survey-among-syrian-refugees-lebanon-november-2019.
Doocy S, Lyles E, Roberton T, Weiss W, Burnham G. Syrian Refugee Health Access Survey in Jordan. UNHCR 2014.
Doocy S, Paik KE, Lyles E, Tam HH, Fahed Z, Winkler E et al. Guidelines and mHealth to Improve Quality of Hypertension and Type 2 Diabetes Care for Vulnerable Populations in Lebanon: Longitudinal Cohort Study. JMIR mHealth and uHealth 2017; 5. https://doi.org/10.2196/mhealth.7745.
Khader A, Farajallah L, Shahin Y, Hababeh M, Abu-Zayed I, Zachariah R, et al. Hypertension and treatment outcomes in Palestine refugees in United Nations Relief and Works Agency primary health care clinics in Jordan. Tropical Med Int Health. 2014;19:1276–83.
Kayali M, Moussally K, Lakis C, Abrash MA, Sawan C, Reid A et al. Treating Syrian refugees with diabetes and hypertension in Shatila refugee camp, Lebanon: Médecins Sans Frontières model of care and treatment outcomes. Confl Health 2019; 13. https://doi.org/10.1186/s13031-019-0191-3.
Cherfan M, Blacher J, Asmar R, Chahine MN, Zeidan RK, Farah R, et al. Prevalence and risk factors of hypertension: A nationwide cross-sectional study in Lebanon. J Clin Hypertension. 2018;20:867–79.
Yurekli AA, Bilir N, Husain MJ. Projecting burden of hypertension and its management in Turkey, 2015-2030. PLoS ONE. 2019;14:e0221556 https://doi.org/10.1371/journal.pone.0221556.
Khader Y, Batieha A, Jaddou H, Rawashdeh SI, El-Khateeb M, Hyassat D et al. Hypertension in Jordan: prevalence, awareness, control, and Its Associated Factors. Int J Hypertens. 2019. https://doi.org/10.1155/2019/3210617.
UNRWA. Health Department Annual Report. 2018. www.unrwa.org.
Centers for Disease Control and Prevention. Health of resettled iraqi refugees—San Diego County, California, October 2007–September 2009. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5949a2.htm.
American Heart Association. Know your risk factors for high blood pressure. https://www.heart.org/en/health-topics/high-blood-pressure/why-high-blood-pressure-is-a-silent-killer/know-your-risk-factors-for-high-blood-pressure.
Ahmad A, Oparil S. Hypertension in women: recent advances and lingering questions. Hypertension. 2017;70:19–26.
Wenger NK, Arnold A, Noel C, Merz B, Cooper-Dehoff RM, Ferdinand KC, et al. Hypertension across a woman’s life cycle HHS public access. J Am Coll Cardiol. 2018;71:1797–1813.
Michalak L, Trocki K. Alcohol and islam: an overview. Contemp Drug Probl. 2006;33:523–62.
Samanic CM, Barbour KE, Liu Y, Wang Y, Fang J, Lu H, et al. Prevalence of self-reported hypertension and antihypertensive medication use by county and rural-urban classification—United States, 2017. MMWR Morbidity Mortal Wkly Rep. 2020;69:533–9.
Executive Report of the Food Security Assessment. West Bank and Gaza Strip. http://www.fao.org/3/j1575e/j1575e01.pdf.
Akik C, Ghattas H, Mesmar S, Rabkin M, El-Sadr WM, Fouad FM. Host country responses to non-communicable diseases amongst Syrian refugees: a review. Confl Health. 2019;13:8.
Verme P, Gigliarano C, Wieser C, Hedlund K, Petzoldt M, Santacroce M. The welfare of Syrian refugees: evidence from Jordan and Lebanon. Washington, DC: World Bank 2016. https://www.worldbank.org/en/topic/poverty/publication/the-welfare-of-syrian-refugees-evidence-from-jordan-and-lebanon.
UNHCR. Survey finds Syrian refugees in Lebanon became poorer, more vulnerable in 2017. 2018. https://www.unhcr.org/news/briefing/2018/1/5a548d174/survey-finds-syrian-refugees-lebanon-poorer-vulnerable-2017.html.
Burnier M, Egan BM. Adherence in hypertension: a review of prevalence, risk factors, impact, and management. Circulation Res. 2019;124:1124–40.
Centers for Disease Control and Prevention. Hypertension Communications Kit. https://www.cdc.gov/bloodpressure/communications_kit.htm.
World Health Organization. Control of hypertension with medication: a comparative analysis of national surveys in 20 countries. WHO 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zibara, V., Costanian, C., Al Haddad, N. et al. Epidemiology and management of hypertension among refugees in the Middle East: a review of the literature. J Hum Hypertens 35, 657–666 (2021). https://doi.org/10.1038/s41371-021-00508-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00508-5
This article is cited by
-
Deliveries in Lebanon, the Country with the Highest Refugee Density in the World: A Descriptive Review
Maternal and Child Health Journal (2024)
-
Challenges of managing hypertension in Pakistan - a review
Clinical Hypertension (2023)
-
Spotlight on hypertension in the Middle-East
Journal of Human Hypertension (2022)